ICU Management & Practice, Volume 17 - Issue 1, 2017
Invasive ventilatory support, one of the most frequently applied strategies in intensive care unit (ICU) patients, is increasingly recognised as a potentially dangerous intervention. Recognition of so–called ventilator– induced lung injury and the broad acceptance of lung–protective ventilation strategies in ICUs worldwide led to noticeable changes in ventilatory management (Putensen et al. 2009; Briel et al. 2010): low tidal volumes and higher levels of positive end–expiratory pressure (PEEP), respectively, to prevent overdistension and repeatedly opening and closing, are increasingly used in patients with acute respiratory distress syndrome (ARDS) (Checkley et al. 2008; Sutherasan et al. 2014; Esteban et al. 2013; Bellani et al. 2016). A high driving pressure level was recently documented as another potentially modifiable factor in ventilator–induced lung injury in one meta-analysis (Amato et al. 2015) and one large observational study (Bellani et al. 2016; Laffey et al. 2016) of ARDS patients. However, it remains uncertain what is the best way to lower the driving pressure level and also whether a strategy aiming at a lower driving pressure truly affects outcome.
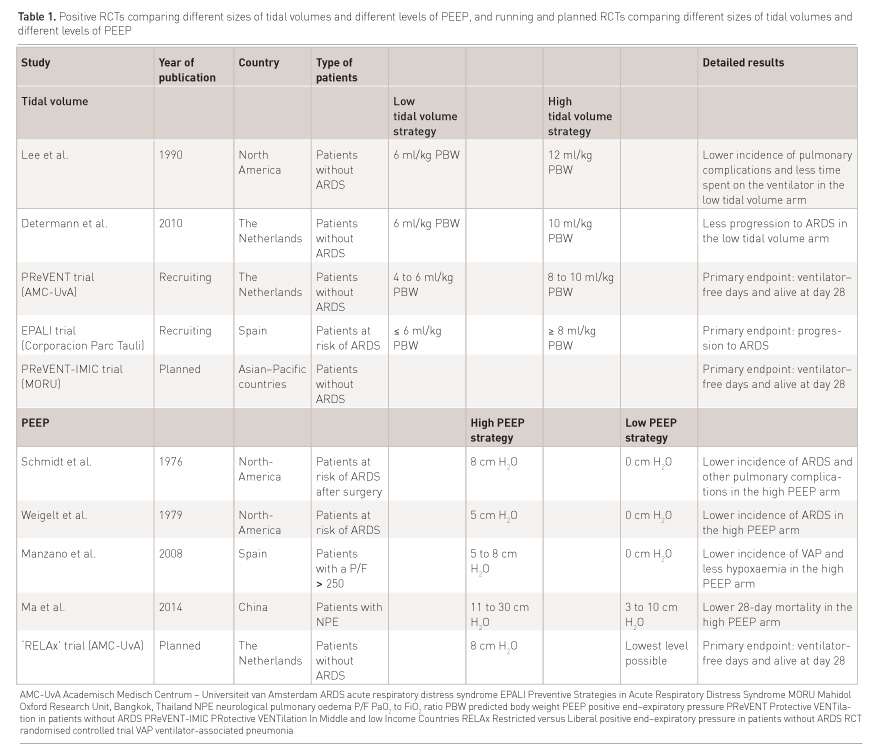
While it is likely that these protective, or potentially protective strategies also benefit patients without ARDS (Serpa Neto et al. 2014a; 2015a; 2014b), changes in ventilatory support in these patients have been less impressive, and ventilator settings known to cause ventilator–induced lung injury in ARDS patients continue to be used in patients without ARDS (Azevedo et al. 2013; Lellouche et al. 2012). This is possibly due to the lack of robust and convincing randomised controlled trial (RCT) evidence for benefit of lung–protective ventilation strategies in patients without ARDS. We discuss the available evidence for benefit of protective ventilation strategies in patients without ARDS, including the use of low tidal volumes, higher levels of PEEP and lower driving pressure levels (Table 1).
Low Tidal Volumes
Evidence for benefit in patients without ARDS
Results of two RCTs suggest benefit from tidal volume reductions in critically ill patients without ARDS (Lee et al. 1990; Determann et al. 2010). One North American group of investigators studied the safety of tidal volume reduction from 12 to 6 ml/kg predicted body weight (PBW) in a cohort of ICU patients without ARDS (Lee et al. 1990). They found tidal volume reduction to be associated with a lower number of pulmonary complications and less time spent on the ventilator. A group of investigators in the Netherlands compared ventilation using tidal volumes of 10 ml/kg PBW with one using 6 ml/kg PBW (Determann et al. 2010). They found tidal volume reduction to be associated with less progression to ARDS. Time spent on the ventilator, however, was not different in this RCT.
Three meta-analyses including several observational studies as well as the two aforementioned RCTs (Serpa Neto et al. 2012; 2014a; 2015a) suggest tidal volume reduction to reduce time spent on the ventilator, duration of stay in the ICU and hospital, and also to prevent progression to ARDS.
Arguments against low tidal volumes in patients without ARDS
Several arguments against tidal volume reduction in patients without ARDS have been suggested. The compensatory higher respiratory rates needed with use of low tidal volumes could cause discomfort that potentially increases sedation needs (Ferguson 2012), risks of muscle weakness (Lipshutz and Gropper 2013), patient–ventilator asynchronies (Kallet et al. 2006; Kallet et al. 2001a) and atelectasis (Kallet et al. 2001b). Whether these assumed disadvantages of tidal volume reduction blunt the beneficial effects of prevention of overstretching of lung tissue seems unlikely, especially when considering that a tidal volume size of ~ 6 ml/kg PBW is seen as normal, and also most efficient in healthy mammals (Tenney & Remmers 1963). Certainly, critically ill invasively ventilated patients could never be seen as healthy individuals, but if one considers these patients may develop atelectases we may even want to reduce tidal volume even below what we call normal.
Current Practice
Recent observational studies suggest that tidal volumes in patients without ARDS are often high, and at least higher than what is presumed safe for patients with ARDS (Linko et al. 2009; Chang et al. 2013; Elmer et al. 2013; Serpa Neto et al. 2016a). Interestingly, tidal volumes are also frequently higher than what ICU physicians say they prefer (Rose et al. 2014). Whereas the small decrease in tidal volumes over the last decade seems promising (Esteban et al. 2013; Serpa Neto et al. 2016a), still more than 30% of patients receive ventilatory support with tidal volumes >8 ml/kg PBW (Serpa Neto et al. 2016a).
See Also: Acute Respiratory Distress Syndrome: The Era of Prevention
PEEP in Patients Without ARDS
Evidence for Benefit
The results of four RCTs suggest benefit from higher levels of PEEP in critically ill patients without ARDS (Ma et al. 2014; Schmidt et al. 1976; Weigelt et al. 1979; Manzano et al. 2008). One Chinese group of investigators compared a strategy using PEEP between 11 and 30cm H2O with one using PEEP between 3 and 10 cm H2O (Ma et al. 2014). They found a higher level of PEEP to be associated with a larger number of patients that survived till day 28. Another team of investigators compared PEEP of 8 cm H2O with PEEP of 0cm H2O (Schmidt et al. 1976). They found a higher level of PEEP to be associated with less progression to ARDS. The same results came from a RCT by a North American group of investigators comparing PEEP of 5cm H2O with PEEP of 0cm H2O (Weigelt et al. 1979). Lastly, one Spanish RCT comparing PEEP of 5 to 8cm H2O with PEEP of 0cm H2O showed a lower incidence of ventilator–associated pneumonia in patients ventilated with higher levels of PEEP (Manzano et al. 2008).
One recently published meta-analysis that used data from all 21 investigations of PEEP in ICU patients without ARDS (Pepe et al. 1984; Nelson et al. 1987; Michalopoulos et al. 1998; Lago Borges et al. 2014; Carroll et al. 1988; Celebi et al. 2007; Borges et al. 2012; Borges et al. 2013; Holland et al. 2007; Dyhr et al. 2002; Marvel et al. 1986; Murphy et al. 1983; Zurick et al. 1982; Good et al. 1979; Vigil & Clevenger 1996; Cujec et al. 1993; Feeley et al. 1975), including the four positive RCTs mentioned above, however, suggests no benefit from using higher levels of PEEP regarding important clinical outcomes like mortality, duration of ventilation, and development of ARDS or pneumonia (Serpa Neto et al. 2016b). Of note, quality of the meta-analysed studies was at times low to very low, and there was substantial heterogeneity amongst the metaanalysed studies.
In the absence of high quality RCTs in ICU patients we may want to consider the results of RCTs comparing different levels of PEEP during intraoperative ventilation. The results of three well–performed RCTs suggest benefit from higher levels of PEEP in surgery patients without ARDS (Futier et al. 2013; Severgnini et al. 2013; Ge et al. 2013). Of note, these three RCTs all compared bundles of ventilation, i.e., a combination of low tidal volumes plus a higher level of PEEP vs. a combination of high tidal volumes plus lower levels of PEEP, which makes it difficult if not impossible to determine the individual effect of the higher levels of PEEP in these patients. A large RCT comparing high levels of PEEP with low levels of PEEP with similar tidal volumes during intraoperative ventilation, though, found no benefit of higher levels of PEEP regarding development of postoperative pulmonary complications (PROVE Network Investigators for the Clinical Trial Network of the European Society of Anaesthesiology et al. 2014). In addition a recent individual patient data meta-analysis using data from these four RCTs of intraoperative ventilation found a clear association between improved outcome and the intraoperative use of low tidal volumes, and not the use of higher levels of PEEP (Serpa Neto et al. 2015b).
Arguments Against Use of Higher Levels of PEEP
Two frequently mentioned arguments against the use of higher levels of PEEP in ICU patients without ARDS include the impact on the haemodynamic system (PROVE Network Investigators for the Clinical Trial Network of the European Society of Anaesthesiology et al. 2014), and the risk of overdistension (Serpa Neto et al. 2016c). Similar to other interventions, it could be that the beneficial effects of PEEP are not linear to its level, but rather U–shaped (Li et al. 2015; Gurudatt 2012; Bellamy 2006). The best level of PEEP then must be somewhere in between a (too) low and a (too) high level of PEEP. Indeed, a too low level of PEEP may fail to recruit sufficient amounts of collapsed lung tissue while increasing the afterload of the right ventricle of the heart. A too high level of PEEP may be able to recruit large amounts of collapsed lung tissue but also cause overdistension of nondependent lung tissue. Likely, the presence and severity of ARDS influences the shape of this hypothetical curve, which may at least in part explain why higher levels of PEEP have been found to be beneficial only in patients with moderate and severe ARDS, while not resulting in better outcomes in patients with mild ARDS (Briel et al. 2010) and patients without ARDS (Serpa Neto et al. 2016b).
Current
Practice
A large worldwide observational international study showed that the average PEEP level used in patients without ARDS is low, with more than 50% of patients on PEEP ≤5cm H2O (Serpa Neto et al. 2016a). In these patients the level of PEEP did not change much over recent years (Esteban et al. 2013; Serpa Neto et al. 2016a), although there are regional differences in use of PEEP. For instance, in the Netherlands, PEEP levels in patients without ARDS were found to be surprisingly higher compared to levels in neighbouring European countries in one large observational study (van IJzendoorn et al. 2014).
Driving Pressure in Patients Without ARDS
Evidence for Benefit
There is very little direct clinical evidence for beneficial effects of lower driving pressure levels, as there have been no RCTs that tested a ventilation strategy that aimed for lower driving pressure levels, neither in ARDS patients, nor in ICU patients without ARDS. One recent observational study in critically ill patients found lower driving pressures to be associated with lower mortality rates (Serpa Neto et al. 2016a).
In the absence of RCTs in ICU patients we may want to consider the results of a recently published individual patient data meta-analysis including RCTs comparing different ventilation strategies during intraoperative ventilation (Serpa Neto et al. 2016). This meta-analysis suggests, firstly, that the driving pressure level per se seems to be associated with occurrence of postoperative pulmonary complications, and secondly that changes in the level of PEEP that resulted in a rise of the driving pressure level are associated with an increased occurrence of postoperative pulmonary complications. One plausible explanation could be that the rise of the driving pressure level is caused by overdistension induced by higher levels of PEEP, which may result in postoperative pulmonary complications, but this hypothesis remains to be tested in RCTs.
Arguments
Against Low Driving Pressures
All studies performed so far comprise subanalyses of protective ventilation strategies using a certain level of PEEP with low tidal volumes. The balance between disadvantages and advantages of strategies specifically aiming at lower driving pressure levels remains uncertain. It is even more uncertain if a strategy aiming at a lower driving pressure is feasible, i.e., really reduces the driving pressure level below a certain level at which we consider the driving pressure level to be safe. Actually, we do not have a clue what we can call a safe driving pressure level. One additional problem is that patients without ARDS are more often receiving supported modes rather than mandatory modes of ventilation. This is where we encounter another hurdle: how to measure the driving pressure adequately in those patients?
Current
Practice
A recently published large worldwide observational study shows the driving pressure level in patients without ARDS to vary between 9 and 13cm H2O (Serpa Neto et al. 2016a). Other studies are highly needed to confirm this finding, and of course RCTs that test whether a ventilation strategy aiming for lower driving pressure levels really improves outcome of patients without ARDS.
Future Directions
There is a clear need for robust evidence from well–powered RCTs for use of low tidal volumes, PEEP and strategies that aim at low driving pressure levels in critically ill patients without ARDS. At present, two European multicentre RCTs, the Protective Ventilation in Patients without ARDS at Start of Ventilation (PReVENT) trial (AMC-UvA n.d.), and the Preventive Strategies in Acute Respiratory Distress Syndrome (EPALI) trial (Corporacion Parc Tauli n.d.) are investigating the impact of tidal volume reduction on outcome of ICU patients without ARDS. PReVENT is a Dutch multicentre RCT comparing low tidal volumes (4 to 6ml/kg PBW) with conventional tidal volumes (8 to 10ml/kg PBW) but a maximum plateau pressure of 25 cm H2O (AMC-UvA n.d.). EPALI is a Spanish multicentre RCT comparing low tidal volumes (≤6ml/kg PBW) to conventional tidal volumes (8ml/kg PBW) in patients at risk for ARDS (Corporacion Parc Tauli n.d.). The primary endpoints of PReVENT and EPALI are the number of ventilator–free days and alive at day 28, and development of ARDS respectively. We ourselves have also initiated a multicentre RCT comparing low to high tidal volumes in Asian countries, the Protective Ventilation in Patients without ARDS at Start of Ventilation in Middle Income Countries (PReVENT-IMIC) (MORU, n.d.), using the same endpoint as in PReVENT. The REstricted versus Liberal positive end–expiratory pressure in patients without ARDS (RELAx) trial, a multicentre RCT comparing a standard level of PEEP of 8cm H2O with the lowest possible level of PEEP in ICU patients without ARDS, is planned to start in the Netherlands in 2017. To the best of our knowledge no other RCTs that compare ventilation strategies aiming at different driving pressure levels in ICU patients without ARDS are presently planned.
Conflicts
of interest
Fabienne Simonis declares that she has no
conflict of interest. Marcus J. Schultz declares that he has no conflict of
interest. Antonio Artigas Raventós declares that he has no conflict of
interest.
Abbreviations
AMC-UvA Academisch Medisch Centrum
ARDS acute respiratory distress syndrome
MORU Mahidol Oxford Research Unit, Bangkok, Thailand
PBW predicted body weight
PEEP positive end-expiratory pressure
RCT randomised controlled trial
References:
Amato MBP, Meade MO, Slutsky AS et al. (2015) Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med, 372(8): 747–55.
AMC-UvA, Academisch Medisch Centrum - Universiteit van Amsterdam. PRotective VENTilation in Patients without ARDS (PReVENT-NL). In: ClinicalTrials.gov NLM Identifier: NCT02153294.
Azevedo LC, Park M, Salluh JIF et al. (2013) Clinical outcomes of patients requiring ventilatory support in Brazilian intensive care units: a multicenter, prospective, cohort study. Crit Care, 17(2): R63.
Bellamy MC (2006) Wet, dry or something else? Br J Anaesth, 97(6), 755–757.
Bellani G, Laffey JG, Pham T et al. (2016) Epidemiology, patterns of care, and mortality for patients with Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. JAMA, 315(8): 788–800.
Borges DL, Nina VJ, Costa Mde A et al. (2013) Effects of different PEEP levels on respiratory mechanics and oxygenation after coronary artery bypass grafting. Rev Bras Cir Cardiovasc, 28(3), 380–5.
Borges JB, Suarez-Sipmann F, Bohm SH et al. (2012) Regional lung perfusion estimated by electrical impedance tomography in a piglet model of lung collapse. J Appl Physiol (1985), 112(1): 225–36.
Briel M, Meade M, Mercat A et al. (2010) Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA, 303(9): 865–73.
Carroll GC, Tuman KJ, Braverman B:et al. (1988) Minimal positive end-expiratory pressure (PEEP) may be “best PEEP”. Chest, 93(5), 1020–5.
Celebi S, Köner O, Menda F et al. (2007) The pulmonary and hemodynamic effects of two different recruitment maneuvers after cardiac surgery. Anesth Analg, 104(2): 384–90.
Chang SY, Dabbagh O, Gajic O et al. (2013) Contemporary ventilator management in patients with and at risk of ALI/ARDS. Respir Care, 58(4): 578–88.
Checkley W, Brower R, Korpak A et al. (2008) Effects of a clinical trial on mechanical ventilation practices in patients with acute lung injury. Am J Respir Crit Care Med, 177(11): 1215–22.
Corporacion Parc Tauli, Corporacion Parc Tauli. Preventive Strategies in Acute Respiratory Distress Syndrome (ARDS) (EPALI). In: ClinicalTrials.gov
Cujec B, Polasek P, Mayers I et al. (1993) Positive end-expiratory pressure increases the right-to-left shunt in mechanically ventilated patients with patent foramen ovale. Ann Intern Med, 119(9): 887–94.
Determann RM, Royakkers A, Wolthuis EK et al. (2010) Ventilation with lower tidal volumes as compared with conventional tidal volumes for patients without acute lung injury: a preventive randomized controlled trial. Crit Care, 14(1): R1.
Dyhr T, Laursen N, Larsson A (2002) Effects of lung recruitment maneuver and positive end-expiratory pressure on lung volume, respiratory mechanics and alveolar gas mixing in patients ventilated after cardiac surgery. Acta Anaesthesiol Scand, 46(6): 717–25.
Elmer J, Hou P, Wilcox SR et al. (2013. Acute respiratory distress syndrome after spontaneous intracerebral hemorrhage. Crit Care Med, 41(8): 1992–2001.
Esteban A, Frutos-Vivar F, Muriel A et al. (2013) Evolution of mortality over time in patients receiving mechanical ventilation. American journal of respiratory and critical care medicine, 188(2): 220–30.
Feeley TW, Saumarez R, Klick JM et al. 1975. Positive end-expiratory pressure in weaning patients from controlled ventilation. A prospective randomised trial. Lancet, 2(7938): 725–9.
Ferguson ND (2012) Low tidal volumes for all? JAMA , 308(16): 689–90.
Futier E, Constantin JM, Paugam-Burtz C et al. (2013) A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med, 369(5): 428–37.
Ge Y, Yuan L, Jiang X et al. (2013) [Effect of lung protection mechanical ventilation on respiratory function in the elderly undergoing spinal fusion]. Zhong Nan Da Xue Xue Bao Yi Xue Ban = Journal of Central South University. Medical sciences, 38(1): 81–5.
Good JTJr, Wolz JF, Anderson JT et al. (1979) The routine use of positive end-expiratory pressure after open heart surgery. Chest, 76(4): 397–400.
Gurudatt CL (2012) Perioperative fluid therapy: How much is not too much? Indian J Anaesth, 56(4): 323–5.
Holland A, Thuemer O, Schelenz C et al. (2007) Positive end-expiratory pressure does not affect indocyanine green plasma disappearance rate or gastric mucosal perfusion after cardiac surgery. Eur J Anaesth, 24(2): 141–7.
Kallet RH, Campbell AR, Dicker RA et al. (2006) Effects of tidal volume on work of breathing during lung-protective ventilation in patients with acute lung injury and acute respiratory distress syndrome. Crit Care Med, 34(1): 8–14.
Kallet RH, Corral W, Silverman H et al. (2001) Implementation of a low tidal volume ventilation protocol for patients with acute lung injury or acute respiratory distress syndrome. Respir Care, 46(10): 1024–37.
Kallet RH, Siobal MS, Alonso JA et al. (2001) Lung collapse during low tidal volume ventilation in acute respiratory distress syndrome. Respir Care, 46(1): 49–52.
Laffey JG, Bellani G, Pham T et al. (2016) Potentially modifiable factors contributing to outcome from acute respiratory distress syndrome: the LUNG SAFE study. Intensive Care Med, 42(12):1865-76.
Lago Borges D, José da Silva Nina V, Pereira Baldez TE et al. (2014) Effects of positive end-expiratory pressure on mechanical ventilation duration after coronary artery bypass grafting: a randomized clinical trial. Ann Thorac Cardiovasc Surg, 20 Suppl: 773–7.
Lee PC, Helsmoortel CM, Cohn SM et al. (1990) Are low tidal volumes safe? Chest, 97(2): 430–4.
Lellouche F, Dionne S, Simard S et al. (2012) High tidal volumes in mechanically ventilated patients increase organ dysfunction after cardiac surgery. Anesthesiology, 116(5): 1072–82.
Li Y, Bai Z, Li M et al. (2015) U-shaped relationship between early blood glucose and mortality in critically ill children. BMC Pediatrics, 15: 1–9.
Linko R, Okkonen M, Pettilä V et al. (2009. Acute respiratory failure in intensive care units. FINNALI: a prospective cohort study. Intensive Care Med, 35(8): 1352–61.
Lipshutz AKM, Gropper MA (2013) Acquired neuromuscular weakness and early mobilization in the intensive care unit. Anesthesiology, 118(1): 202–15.
Ma C, Liang D, Zheng F (2014) [Effect of high positive end-expiratory pressure for mechanical ventilation in the treatment of neurological pulmonary edema]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue, 26(5): 339–42.
Manzano F, Fernández-Mondéjar E, Colmenero M et al. (2008) Positive-end expiratory pressure reduces incidence of ventilator-associated pneumonia in nonhypoxemic patients. Crit Care Med, 36(8): 2225–31.
Marvel SL, Elliott CG, Tocino I et al. (1986) Positive end-expiratory pressure following coronary artery bypass grafting. Chest, 90(4): 537–41.
Michalopoulos A, Anthi A, Rellos K et al. (1998) Effects of positive end-expiratory pressure (PEEP) in cardiac surgery patients. Respir Med, 92(6): 858–62.
Murphy DA, Finlayson DC, Craver JM et al. (1983) Effect of positive end-expiratory pressure on excessive mediastinal bleeding after cardiac operations. A controlled study. J Thorac Cardiovasc Surg, 85(6): 864–9.
Nelson LD, Civetta JM, Hudson-Civetta J (1987) Titrating positive end-expiratory pressure therapy in patients with early, moderate arterial hypoxemia. Crit Care Med, 15(1): 14–9.
Pepe PE, Hudson LD, Carrico CJ (1984) Early application of positive end-expiratory pressure in patients at risk for the adult respiratory-distress syndrome. N Engl J Med, 311(5): 281–6.
PROVE Network Investigators for the Clinical Trial Network of the European Society of Anaesthesiology et al. (2014) High versus low positive end-expiratory pressure during general anaesthesia for open abdominal surgery (PROVHILO trial): a multicentre randomised controlled trial. Lancet (London, England), 384(9942): 495–503.
Putensen C, Theuerkauf N, Zinserling J et al. (2009) Meta-analysis: ventilation strategies and outcomes of the acute respiratory distress syndrome and acute lung injury. Ann Intern Med, 151(8): 566–76.
Rose L, Kenny L, Tait G et al. (2014) Ventilator settings and monitoring parameter targets for initiation of continuous mandatory ventilation: a questionnaire study. J Crit Care, 29(1): 123–7.
Schmidt GB, O'Neill WW, Kotb K et al. (1976) Continuous positive airway pressure in the prophylaxis of the adult respiratory distress syndrome. Surg Gynecol Obstet, 143(4): 613–8.
Serpa Neto A, Cardoso SO, Manetta JA et al. (2012) Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome: a meta-analysis. JAMA, 308(16): 1651–9.
Serpa Neto A, Simonis FD, Barbas CS et al. (2014a) Association between tidal volume size, duration of ventilation, and sedation needs in patients without acute respiratory distress syndrome: an individual patient data meta-analysis. Intensive Care Med, 40(7): 950–7.
Serpa Neto A, Nagtzaam L, Schultz MJ (2014b) Ventilation with lower tidal volumes for critically ill patients without the acute respiratory distress syndrome: a systematic translational review and meta-analysis. Curr Opin Crit Care, 20(1): 25–32.
Serpa Neto A, Simonis FD, Barbas CS et al. (2015a) Lung-protective ventilation with low tidal volumes and the occurrence of pulmonary complications in patients without acute respiratory distress syndrome. Crit Care Med, 43(10): 2155–63.
Serpa Neto A, Hemmes SN, Barbas CS et al. (2015b) Protective versus conventional ventilation for surgery. Anesthesiology, 123(1), 66–78.
Serpa Neto A, Barbas CSV, Simonis FD et al. (2016a) Epidemiological characteristics, practice of ventilation, and clinical outcome in patients at risk of acute respiratory distress syndrome in intensive care units from 16 countries (PRoVENT): an international, multicentre, prospective study. Lancet Respir Med, 4(11):882–93.
Serpa Neto A, Filho RR, Cherpanath T et al. (2016b) Associations between positive end-expiratory pressure and outcome of patients without ARDS at onset of ventilation: a systematic review and meta-analysis of randomized controlled trials. Ann Intensive Care, 6(1): 109.
Serpa Neto A, Hemmes SNT, Barbas CS et al. (2016c) Association between driving pressure and development of postoperative pulmonary complications in patients undergoing mechanical ventilation for general anaesthesia: a meta-analysis of individual patient data. Lancet Respir Med, 4(4): 272–80.
Severgnini P, Selmo G, Lanza C et al. (2013) Protective mechanical ventilation during general anesthesia for open abdominal surgery improves postoperative pulmonary function. Anesthesiology, 118(6), 1307–21.
Sutherasan Y, D’Antini D, Pelosi P (2014) Advances in ventilator-associated lung injury: prevention is the target. Expert Rev Respir Med, 8(2): 233–48.
Tenney SM, Remmers JE (1963) Comparative quantitative morphology of the mammalian lung: diffusing area. Nature, 197: 54–6.
van IJzendoorn MC, Koopmans M, Strauch U et al. (2014) Ventilator settings in ICUs: comparing a Dutch with a global cohort. Crit Care, 18(Suppl 1): P277.
Vigil AR, Clevenger FW (1996) The effects of positive end-expiratory pressure of intrapulmonary shunt and ventilatory deadspace in nonhypoxic trauma patients. J Trauma, 40(4): 618-22.
Weigelt JA, Mitchell RA, Snyder WH (1979) Early positive end-expiratory pressure in the adult respiratory distress syndrome. Arch Surg, 114(4): 497–501.
Zurick AM, Urzua J, Ghattas M et al. (1982) Failure of positive end-expiratory pressure to decrease postoperative bleeding after cardiac surgery. Ann Thorac Surg, 34(6): 608–11.









