Implementing change in the ICU is not easy, but change management, managed implementation of checklists and bundles and electronic records are all measures that can be used to put guidelines into practice. Speakers from Sweden, France and the UK addressed the issues in a session at the European Society of Intensive Care Medicine 2015 congress in Berlin, 3-7 October.
Her own ICU, Karolinska Huddinge is a multiprofessional, multidisciplinary mixed medical and surgical ICU. One-third of their patients are gravely immunosuppressed, and they have a large proportion of patients who have had abdominal surgery and are susceptible to infection. They have in place an infection control team with very low staff turnover, enthusiastic support from the local manager and a dedicated resource for screening and registration of ICU-acquired infections weekly. They check point prevalence on compliance to infection control measures every month, feedback the results to the staff, hold regular education sessions, and also ask nurses if doctors comply. However, they still experienced central venous catheter (CVC)-related infections. In Spring 2015 they implemented a “Scrub the Hub” initiative, disinfecting access sites prior to CVC use, a measure that has proven effective as a stepwise intervention (Munoz-Price et al. 2012).
They motivated the staff to take the time to scrub the hub and wait for it to dry by including different routines, as seen in a video Scrub The Hub Sweden (in Swedish). As Agvald-Öhman said, you also need to have fun when following the guidelines. Answering questions from delegates, Agbald-Öhman mentioned that their programme used a coach, paid for from research and government monies. They had access to the coach for year, both on site and by video. “Ensuring compliance has a beginning, but no end”, said Agvald-Öhman.
Electronic patient records make available measurements via predefined queries, and a regular report should be produced and available to the care team. The RAND corporation report on Factors Affecting Physician Professional Satisfaction and Their Implications for Patient Care, Health Systems, and Health Policy found that most EMRs fail to support efficient and effective clinical work, and that many clinicians feel demoralised rather than supported by EMR technology. The patient data management system must help avert medical error and support protocol adherence while avoiding alert overload. Computerised support can also be of use for nursing staff, for example in planning, preparing and administering drugs. However, a data model that adequately supports these varying functional requirements is lacking. Future PDSM applications are likely to include these.
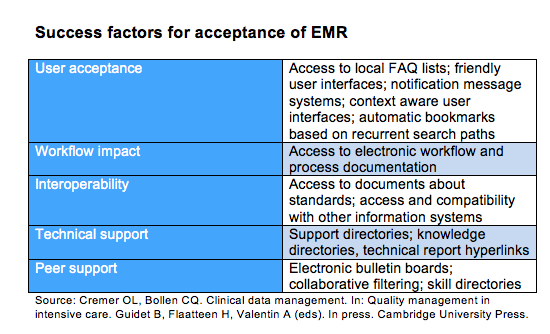
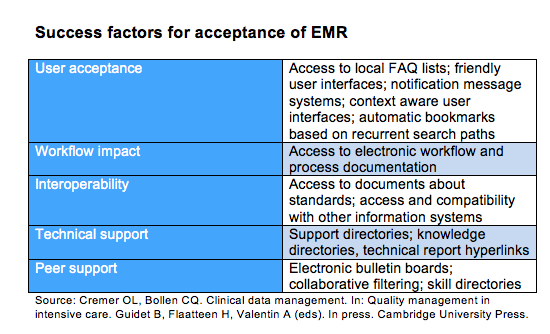
Success factors for acceptance of EMR are user acceptance, workflow impact, interoperability, technical support and peer support. Patient-oriented information views are needed, organised by clinical concepts, active problems, haemodynamics, renal function, coagulation etc.
A simulation-based study on the effect of an electronic checklist on critical care provider workload, errors and performance (Thongprayoon et al. 2014) found significantly reduced provider workload and errors without any measurable difference in the amount of time required for checklist completion. Pickering et al. (2015), in their study of implementation of a clinician designed, human-centred EMR viewer in the ICU, found that time spent on pre-round data gathering per patient decreased from 12 to 9 minutes. One approach is to identify a target population that could be treated through an algorithm. Semler et al. (2015) conducted a a randomised controlled trial of an electronic tool for the evaluation and treatment of sepsis in the ICU. This picked up more patients that had sepsis but were not septic at admission, and could assist with early recognition of patients. They concluded that a comprehensive electronic sepsis evaluation and management tool is feasible and safe, but did not influence guideline compliance or clinical outcomes, perhaps due to low use.
Specific Areas
Electronic reminders for writing handover summaries could include mandatory administrative tasks, an electronic patient journey board, and electronic tools to facilitate quick and clear handover summary generation. The Airway, breathing, circulation, disability and exposure (ABCDE) approach could be used for a checklist for intrahospital transport.
We need to insist on quality guidelines, acceptability of guidelines and ergonomic electronic systems, said Guidet. Management is important, as are leader commitment, feedback, learning curve, and monitoring patients’ response to the intervention. If it is implemented top down and not integrated, it will not work.
Checklists and Care Bundles
Andrew Rhodes, London, discussed the use of checklists and care bundles. “You can’t just take a checklist and put it into practice”, said Rhodes. You need to develop the change management necessary.
Rhodes noted that a checklist is not just a checklist, and in the Michigan programme, which aimed to reduce catheter-related bloodstream infections in the ICU, they created social networks, reinforced efforts to cooperate with interventions, and had a 9-month implementation period. A senior executive was assigned to work with the ICUs, they had an ICU physician and nurse leader, monthly meetings, and the team leaders received instruction on the science of safety, regular input from infection control teams and feedback.
Safer care is achieved with the following actions:
Session co-chair Julian Bion, Birmingham, observed that the paradox is that over time things get better, and it’s very hard to tell why or explain why. Participation in quality improvement programmes produces benefits for populations even though some of the content of those packages turn out not to be entirely right. If the intervention is behavioural there needs to be local ownership over the whole programme. Feedback is very important, accompanied by interventions allowing opportunity for reflection.
Hans Flaatten, Bergen, concurred that intensive care medicine has tools, electronic records and checklists, and still humans are at the sharp end. It still comes back to the human factor as to how we implement evidence-based medicine.
Julian Bion advised attendees to leave with two thoughts - become a patient and invite a medical sociologist to join a ward round.
Claire Pillar
Managing editor, ICU Management
Leadership
Intensive care leaders are trouble shooters, not trouble finders. It is difficult to implement guidelines, but leaders can introduce systems for cultural, behavioural and systemic change to enable change from the ground up, according to Christina Agvald-Öhman, Stockholm. Her practical tips included:- Be a leader not a boss, a trouble shooter not a trouble finder.
- A leader celebrates good results with the team.
- Strive for improvement to increase patient satisfaction.
- Find good examples, such as the Matching Michigan project.
- Do what research tells us is the best.
- Create an environment for sustainability.
- Motivate the team. If 10% of the staff are motivated, they can inspire the others.
Her own ICU, Karolinska Huddinge is a multiprofessional, multidisciplinary mixed medical and surgical ICU. One-third of their patients are gravely immunosuppressed, and they have a large proportion of patients who have had abdominal surgery and are susceptible to infection. They have in place an infection control team with very low staff turnover, enthusiastic support from the local manager and a dedicated resource for screening and registration of ICU-acquired infections weekly. They check point prevalence on compliance to infection control measures every month, feedback the results to the staff, hold regular education sessions, and also ask nurses if doctors comply. However, they still experienced central venous catheter (CVC)-related infections. In Spring 2015 they implemented a “Scrub the Hub” initiative, disinfecting access sites prior to CVC use, a measure that has proven effective as a stepwise intervention (Munoz-Price et al. 2012).
They motivated the staff to take the time to scrub the hub and wait for it to dry by including different routines, as seen in a video Scrub The Hub Sweden (in Swedish). As Agvald-Öhman said, you also need to have fun when following the guidelines. Answering questions from delegates, Agbald-Öhman mentioned that their programme used a coach, paid for from research and government monies. They had access to the coach for year, both on site and by video. “Ensuring compliance has a beginning, but no end”, said Agvald-Öhman.
Electronic Records
Bertrand Guidet outlined the possibilities of using electronic records to create compliance to guidelines, and previewed a monograph he has co-edited with Hans Flaatten and Andreas Valentin, Quality Management in Intensive Care, due to be published in 2016 by Cambridge University Press. Practical approaches for implementation of a clinical practice guideline are adoption of change, diffusion, dissemination and implementation. You need leaders and the whole team pushing together to make changes, said Guidet.Electronic patient records make available measurements via predefined queries, and a regular report should be produced and available to the care team. The RAND corporation report on Factors Affecting Physician Professional Satisfaction and Their Implications for Patient Care, Health Systems, and Health Policy found that most EMRs fail to support efficient and effective clinical work, and that many clinicians feel demoralised rather than supported by EMR technology. The patient data management system must help avert medical error and support protocol adherence while avoiding alert overload. Computerised support can also be of use for nursing staff, for example in planning, preparing and administering drugs. However, a data model that adequately supports these varying functional requirements is lacking. Future PDSM applications are likely to include these.
Success factors for acceptance of EMR are user acceptance, workflow impact, interoperability, technical support and peer support. Patient-oriented information views are needed, organised by clinical concepts, active problems, haemodynamics, renal function, coagulation etc.
A simulation-based study on the effect of an electronic checklist on critical care provider workload, errors and performance (Thongprayoon et al. 2014) found significantly reduced provider workload and errors without any measurable difference in the amount of time required for checklist completion. Pickering et al. (2015), in their study of implementation of a clinician designed, human-centred EMR viewer in the ICU, found that time spent on pre-round data gathering per patient decreased from 12 to 9 minutes. One approach is to identify a target population that could be treated through an algorithm. Semler et al. (2015) conducted a a randomised controlled trial of an electronic tool for the evaluation and treatment of sepsis in the ICU. This picked up more patients that had sepsis but were not septic at admission, and could assist with early recognition of patients. They concluded that a comprehensive electronic sepsis evaluation and management tool is feasible and safe, but did not influence guideline compliance or clinical outcomes, perhaps due to low use.
Specific Areas
Electronic reminders for writing handover summaries could include mandatory administrative tasks, an electronic patient journey board, and electronic tools to facilitate quick and clear handover summary generation. The Airway, breathing, circulation, disability and exposure (ABCDE) approach could be used for a checklist for intrahospital transport.
We need to insist on quality guidelines, acceptability of guidelines and ergonomic electronic systems, said Guidet. Management is important, as are leader commitment, feedback, learning curve, and monitoring patients’ response to the intervention. If it is implemented top down and not integrated, it will not work.
Checklists and Care Bundles
Andrew Rhodes, London, discussed the use of checklists and care bundles. “You can’t just take a checklist and put it into practice”, said Rhodes. You need to develop the change management necessary.
Rhodes noted that a checklist is not just a checklist, and in the Michigan programme, which aimed to reduce catheter-related bloodstream infections in the ICU, they created social networks, reinforced efforts to cooperate with interventions, and had a 9-month implementation period. A senior executive was assigned to work with the ICUs, they had an ICU physician and nurse leader, monthly meetings, and the team leaders received instruction on the science of safety, regular input from infection control teams and feedback.
Safer care is achieved with the following actions:
- Summarise and simplify.
- Measure and provide feedback on outcomes
- Improve culture by building expectations of performance standards into work processes.
Session co-chair Julian Bion, Birmingham, observed that the paradox is that over time things get better, and it’s very hard to tell why or explain why. Participation in quality improvement programmes produces benefits for populations even though some of the content of those packages turn out not to be entirely right. If the intervention is behavioural there needs to be local ownership over the whole programme. Feedback is very important, accompanied by interventions allowing opportunity for reflection.
Hans Flaatten, Bergen, concurred that intensive care medicine has tools, electronic records and checklists, and still humans are at the sharp end. It still comes back to the human factor as to how we implement evidence-based medicine.
Julian Bion advised attendees to leave with two thoughts - become a patient and invite a medical sociologist to join a ward round.
Claire Pillar
Managing editor, ICU Management
Latest Articles
Intensive care, clinical guidelines, leadership, implementation
How to get better at implementing clinical practice guidelines in the intensive care unit - via leadership, checklists and electronic records.










