Extracorporeal membrane oxygenation (ECMO) use is on the rise, but patients on ECMO often experience major complications, such as acute brain injury (ABI), which doubles or triples in-hospital mortality rates. ABI is more prevalent in venoarterial (VA) ECMO compared to venovenous (VV) ECMO, especially in cases involving extracorporeal cardiopulmonary resuscitation (ECPR), with 27–32% of patients experiencing ABI during ECMO despite its survival benefits.
While protocolised neurological monitoring can improve ABI detection, it is only implemented in limited ECMO centres. The ICU management of ECMO patients, particularly those with ABI, is inconsistent across centres and lacks standardised guidelines and high-quality evidence.
As ECMO usage increases, establishing clinical guidelines and focused research on neurological monitoring and managing ABI is crucial to improving patient care and outcomes. The current variability in practices offers an opportunity to standardise neurological care in ECMO. To address this, an international multidisciplinary panel of experts from neurology, critical care, surgery, and other ECMO-related fields developed consensus recommendations and scientific statements on neurological monitoring and management for adult ECMO patients, endorsed by the Extracorporeal Life Support Organization (ELSO). They identified five key areas needing recommendations:
- Neurological monitoring
- Early post-cannulation physiological targets related to ABI
- Neurological therapies, including medical and surgical interventions
- Neurological prognostication
- Neurological follow-up and outcomes
The panel provided evidence-based recommendations and highlighted knowledge gaps for future research.
Neuromonitoring/Neuroimaging
1.1. Implementing standardised neuromonitoring and involving neurological expertise is recommended for ECMO patients who are at high risk of developing acute brain injury (ABI).
1.2. Continuous cerebral oximetry is recommended to monitor ongoing trends and facilitate early detection of ABI, particularly in patients on peripheral VA ECMO who are at risk for differential hypoxia.
1.3. Intermittent EEG and somatosensory evoked potentials (SSEP) are recommended, especially for comatose patients. Continuous EEG, if available, is particularly beneficial for detecting non-convulsive seizures in these patients.
1.4. Routine pupil assessment is recommended, with consideration for the use of pupillometry when available.
1.5. Early neuroimaging is recommended for ECMO patients at risk of ABI, guided by physical examination findings and neuromonitoring results.
Bedside Management
2.1. Serial arterial blood gas sampling is recommended during the first 24 hours of ECMO support.
2.2. Avoiding arterial hypoxaemia (PaO2 < 70 mmHg) is recommended.
2.3. Avoiding severe arterial hyperoxia (PaO2 > 300 mmHg) is recommended, especially in VA ECMO patients, due to the high risk of reperfusion injury.
2.4. For patients with hypercapnia (PaCO2 > 45 mmHg), it is recommended to avoid rapid changes in PaCO2 during the first 24 hours of ECMO support.
2.5. Continuous core temperature monitoring and active prevention of fever (> 37.7 °C) are recommended.
2.6. Mild to moderate hypothermia (33–36 °C) for 24–48 hours may be considered reasonable in VA ECMO, particularly in cases involving ECPR.
2.7. Hypothermia is not recommended in VV ECMO patients.
2.8. Since optimal ECMO flow and blood pressure targets are not well established, avoiding hypotension and maintaining a mean arterial pressure > 70 mmHg is recommended. Individualised blood pressure goals based on patient comorbidities should be considered until more data is available.
2.9. Individualised blood pressure management tailored to the patient’s dynamic cerebral autoregulation function may be reasonable in ECMO patients.
Interventional Neurology, Neurosurgery, and Neurocritical Care
3.1. Neurological consultation is recommended for any acute neurological changes.
3.2. A non-contrast head CT is recommended to rule out intracranial haemorrhage (ICH) in patients with suspected stroke during ECMO.
3.3. Tissue plasminogen activator (tPA) is not recommended for acute ischaemic stroke in ECMO due to the high risk of bleeding associated with systemic anticoagulation and platelet dysfunction.
3.4. Mechanical thrombectomy is recommended for acute large vessel occlusion.
3.5. Stepwise management of acute intracranial hypertension is recommended.
3.6. The decision to perform decompressive craniectomy for stroke should be made based on a risk-benefit discussion between the multidisciplinary medical team and the patient’s surrogate.
3.7. Careful monitoring of systemic anticoagulation and its resumption after decompressive craniectomy is recommended.
3.8. Prolonged cessation of systemic anticoagulation (more than 2 days) is recommended for acute intracranial haemorrhage during VV ECMO.
3.9. VA ECMO can be maintained without anticoagulation, though it carries a higher risk of thromboembolism. Clinicians should weigh the risks of anticoagulation and bleeding against the risks of running VA ECMO without systemic anticoagulation. VV ECMO can be maintained without anticoagulation for longer due to a lower risk of thromboembolism.
3.10. Early cessation and careful resumption of anticoagulation, along with repeated neuroimaging, are recommended for ECMO-associated ischaemic stroke and intracranial haemorrhage.
3.11. Due to limited data, no specific recommendations on anticoagulation reversal in ECMO are provided.
3.12. Placement of an extra-ventricular drain may be considered for patients with few management options and a high risk of death from intraventricular haemorrhage and hydrocephalus.
3.13. The use of monitors for intracranial pressure and/or brain tissue oxygenation should be considered with caution, as current data do not demonstrate improved outcomes with such monitoring in ECMO patients.
Neurological Prognostication
4.1. For prognostication in extracorporeal cardiopulmonary resuscitation (ECPR), a multimodal, multidisciplinary approach incorporating clinical and neurological examinations, electrophysiological tests, and neuroimaging is recommended.
4.2. Relying on a single factor or tool, such as brain imaging alone, is not recommended for determining patient prognosis.
4.3. Brain death determination should be based on evidence of severe brain injury from imaging, neurological examination, and an apnoea test, following the official guidelines and laws of the specific country. If an apnoea test is difficult, a cerebral angiogram or nuclear scan (radionuclide brain scan) is recommended as an alternative test.
4.4. Regular meetings and goal-of-care discussions with the patient’s surrogate, reflecting the patient’s preferences, are recommended.
Long-Term Outcomes and Quality of Life
Pre-Discharge Care
5.1.1. Clinical examination and use of the modified Rankin Scale before discharge are recommended. Neuroimaging, preferably a conventional MRI of the brain after decannulation, is reasonable for patients with neurological or cognitive dysfunction.
5.1.2. Outpatient care planning should include careful scheduling of visits (ideally at 3, 6, and 12 months post-discharge), selecting appropriate locations for visits (preferably ECMO clinics or neurologist), and addressing ECMO-related comorbidities and complications (such as vascular issues, myopathy, chronic infections, and cardiopulmonary recovery).
5.1.3. Comprehensive education and psychosocial support for patients, their family members, and caretakers are recommended.
5.1.4. Assessing and developing a nutritional plan to support optimal recovery is recommended.
5.2. Post-Discharge Care
5.2.1. Regular neurological and quality-of-life assessments are recommended.
5.2.2. clinical examination by a neurological specialist, neuroimaging (preferably MRI), and other relevant tests are recommended for patients with neurological complications.
5.2.3. Follow-up with disease-specific specialists tailored to the underlying condition and comorbidities, including pulmonologists, cardiologists, neurologists, nephrologists, gastroenterologists, and haematologists, is recommended as needed.
5.2.4. Follow-up with the primary care physician is recommended.
5.2.5. Establishing a centralised and secure data repository to store and share patient information with outpatient healthcare providers is recommended.
The impact of acute brain injury (ABI) on morbidity and mortality in ECMO patients is significant, making early detection and timely intervention crucial for improving outcomes. Therefore, standardised neurological monitoring and specialised neurological expertise are recommended for ECMO patients. These consensus recommendations and scientific statements are designed to guide the monitoring, prevention, and management of ABI associated with ECMO. Where available, multidisciplinary care is strongly encouraged to enhance the likelihood of favourable long-term outcomes and quality of life. Ongoing and further research into predisposing factors, prevention strategies, neuroimaging techniques, and management approaches is needed to reduce or prevent such serious adverse events in ECMO patients.
Source: Critical Care
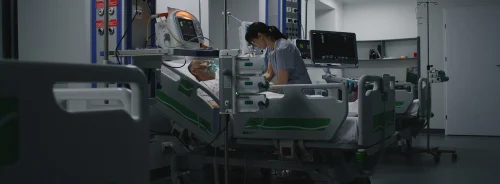
Image Credit: iStock