Checklists and training are essential when transporting the ICU patient, according to Andreas Valentin, Vienna, speaking at the European Society of Intensive Care Medicine (ESICM) congress in Berlin on 6 October.
His advice was simple:
1. Keep extrinsic risk at the lowest possible level;
2. Be familiar with the equipment used during the transport;
3. Expect surprises!
Whether the patient is transferred within the hospital, usually for a diagnostic or interventional procedure, or interhospital to another ICU, they should arrive at least in the same condition as at departure, with no critical incidents, no adverse events and no equipment failure. However, it is not as easy as it seems, and the literature shows the types of problems that can occur, said Valentin.
The risks include:
A study of critical events during land-based interfacility transport by Singh (2014) found that critical events were associated with mechanical ventilation, haemodynamic instability and transport duration. Parmentier-Decrug and collegues in a 2013 study looked at adverse events in 262 mechanically ventilated ICU patients requiring transport for CT; 45% of adverse events occurred during transport, and 32.8% were equipment-related. A study of intrahospital transport by a specialised team Kue et al. 2011) found clinically significant adverse events in 1.7% of transports, excluding technical problems. Top of the list of events was hypoxia > 5 minutes and hypotension. Droogh and colleagues explored inter-hospital transport of critically ill patients in a 2012 study that found 55 technical problems in 353 interhospital transports in a mobile ICU. Beckman studied incidents related to intra-hospital transfer (2004). Reasons for incidents included poor communication, inadequate monitoring, incorrect set up of equipment, artificial airway malpositioning and incorrect positioning of patients. 39% were due to equipment problems, including battery/power supply. Another issue is the need to be familiar with the ventilator interface. In a simulation study by Templier and colleagues of 20 emergency physicians with no prior experience with the tested ventilators there was a markedly different error rate between the two machines. In addition, decision making on transport can vary between intensivists. Van Lieshout in a study of 78 heads of Dutch ICUs, provided with 16 case vignettes found great variation in deciding on interhospital transfer.
The accompanying intensivist needs to think in a structured way about what to do if oxygen saturation decreases. Other equipment problems to consider are displacement of sensors, bad signals, deterioration of perfusion, airway obstruction, pneumothorax, problems with hoses and valves, the ventilator and gas supply. Syringe pumps can develop problems as the result of a vertical displacement manoeuvre. They can get an infusion bolus if raised up, and retrograde aspiration if lowered. This might lead to haemodynamic instability, blood pressure peaks or sudden loss of blood pressure.
Berube et al. (2013) analysed the impact of a preventive programme on occurrence of incidents during transport of critically ill patients. Their programme included checklists and testing of patients' status simulating transport - the patient was connected to transport equipment in the ICU and observed for 5-10 minutes and equipment checked. The programme was effective as 103 incidents reduced to 70 following the intervention.
2. Transport team - education and training
3. Patient optimisation and preparation - establishing and securing the airway, stabilisation on the transport ventilator before transport
4. Equipment check
5. Route planning
Brunsveld-Reinders et al. (2015) Crit Care 2015 provide examples of checklists for the pre-transport, transport and post-transport stages.
Claire Pillar
Managing editor, ICU Management
Top image source: freeimages.com
His advice was simple:
1. Keep extrinsic risk at the lowest possible level;
2. Be familiar with the equipment used during the transport;
3. Expect surprises!
Whether the patient is transferred within the hospital, usually for a diagnostic or interventional procedure, or interhospital to another ICU, they should arrive at least in the same condition as at departure, with no critical incidents, no adverse events and no equipment failure. However, it is not as easy as it seems, and the literature shows the types of problems that can occur, said Valentin.
Risks of Transporting Critically Ill Patients
The intrinsic risk is the severity of illness and susceptibility to physiologic changes associated with the change in environment. The extrinsic risk comes from downgrading the intensity of care, changes in equipment, absence of backup supplies, staff, and possible difficulties in detecting deterioration.The risks include:
- Technical complications, eg displacement of tubes and lines
- Pathophysiological deterioriation, eg increased intracranial pressure,arterial hypotension, decrease in oxygen saturation
- Inadequate monitoring of cardiovascular and pulmonary function due to less sophisticated monitors or equipment/ interference due to motion etc.
- Inadequate therapy due to lack of appropriate equipment: many transportation ventilators cannot deliver the same modes or levels of ventilation as a high-end ICU ventilator
- Additional movements, eg lifting or tilting of patients from bed to trolley, and acceleration forces during air or ambulance transport
- Lack of immediate access to additional investigations or therapy, eg no chest x-ray in ambulance to exclude a pneumothorax
- Limited number of people involved in the transport, lack of more senior people immediately to hand.
A study of critical events during land-based interfacility transport by Singh (2014) found that critical events were associated with mechanical ventilation, haemodynamic instability and transport duration. Parmentier-Decrug and collegues in a 2013 study looked at adverse events in 262 mechanically ventilated ICU patients requiring transport for CT; 45% of adverse events occurred during transport, and 32.8% were equipment-related. A study of intrahospital transport by a specialised team Kue et al. 2011) found clinically significant adverse events in 1.7% of transports, excluding technical problems. Top of the list of events was hypoxia > 5 minutes and hypotension. Droogh and colleagues explored inter-hospital transport of critically ill patients in a 2012 study that found 55 technical problems in 353 interhospital transports in a mobile ICU. Beckman studied incidents related to intra-hospital transfer (2004). Reasons for incidents included poor communication, inadequate monitoring, incorrect set up of equipment, artificial airway malpositioning and incorrect positioning of patients. 39% were due to equipment problems, including battery/power supply. Another issue is the need to be familiar with the ventilator interface. In a simulation study by Templier and colleagues of 20 emergency physicians with no prior experience with the tested ventilators there was a markedly different error rate between the two machines. In addition, decision making on transport can vary between intensivists. Van Lieshout in a study of 78 heads of Dutch ICUs, provided with 16 case vignettes found great variation in deciding on interhospital transfer.
The accompanying intensivist needs to think in a structured way about what to do if oxygen saturation decreases. Other equipment problems to consider are displacement of sensors, bad signals, deterioration of perfusion, airway obstruction, pneumothorax, problems with hoses and valves, the ventilator and gas supply. Syringe pumps can develop problems as the result of a vertical displacement manoeuvre. They can get an infusion bolus if raised up, and retrograde aspiration if lowered. This might lead to haemodynamic instability, blood pressure peaks or sudden loss of blood pressure.
Training
Training is available, for example as a module in Patient-Centred Acute Training (PACT), ESICM’s multidisciplinary distance learning programme for intensive care training. Fanara et al. have published recommendations for intrahospital transport of critically ill patients. These include checklists for preparing the patients, breathing, circulation, the transport team, transport organisation and clinical stability of the patient.Berube et al. (2013) analysed the impact of a preventive programme on occurrence of incidents during transport of critically ill patients. Their programme included checklists and testing of patients' status simulating transport - the patient was connected to transport equipment in the ICU and observed for 5-10 minutes and equipment checked. The programme was effective as 103 incidents reduced to 70 following the intervention.
Questions to Ask Before Transporting a Critically Ill Patient
Before transporting a patient, intensivists need to ask:- What is the aim?
- Will the results have clinical consequences?
- Will the expected benefit outweigh the risks?
- Is the patient stable enough?
- Is the time right?
Equipment
- Monitor
- Defribillator
- Mechanical ventilator - but be aware that in many portable ventilators the airway pressure is dependent on the pressure of the oxygen cylinders
- Oxygen bottles
- Syringe pumps
- Suction equipment
- Emergency kit (including material to establish an airway)
Staffing
There should be at least two attending staff, a doctor and a nurse, and a porter for intrashospital transport, and additional staff from outside in interhospital transfers (eg ambulance crew). There could be a dedicated transfer team. Fried, in a 2010 audit of intrahospital transfers in Scotland found that dedicated transport teams had a much lower incidence of unsecured medical equipment. (1% as against 18%).Route
This is not necessarily the fastest route. When planning you need to calculate the time a cylinder with pressurised oxygen will last. Ask if the patient is properly secured, and if the ambulance is prepared for the distance to be travelled with battery power and a sufficient number of wall sockets.Arrival and Handover
- Assessment of patient and environment
- Careful movement of the patient (secure airway)
- Establish new monitoring
- Establish new ventilator
- Complete handover
- Documentation
Important Steps
1. Decision to transport - Is this transport really necessary?2. Transport team - education and training
3. Patient optimisation and preparation - establishing and securing the airway, stabilisation on the transport ventilator before transport
4. Equipment check
5. Route planning
Brunsveld-Reinders et al. (2015) Crit Care 2015 provide examples of checklists for the pre-transport, transport and post-transport stages.
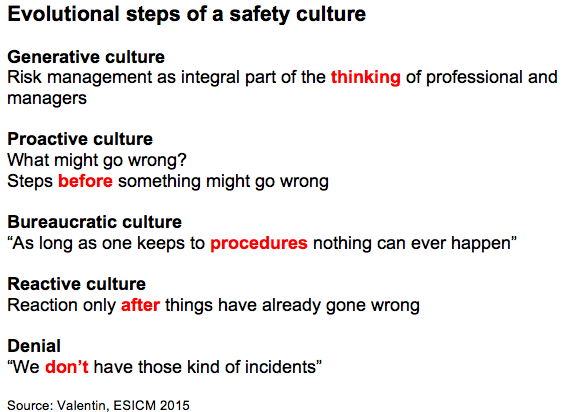
Safety Culture
Developing a safety culture requires evolutional steps, said Valentin. Above all, the ICU staff need to explore the risk before they are in the risk.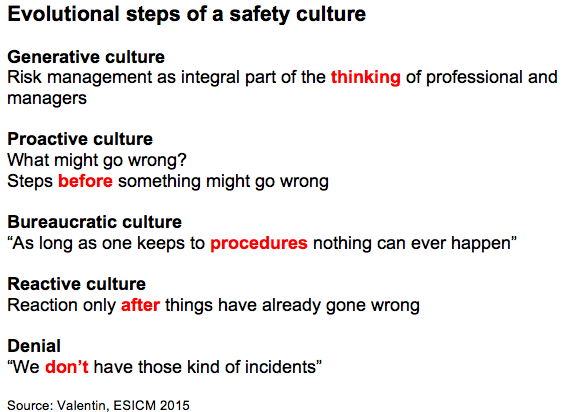
Claire Pillar
Managing editor, ICU Management
Top image source: freeimages.com
Latest Articles
ICU, Critical illness, Transport, Patients
How to transport a critically ill patient within a hospital or between hospitals. The risks, what to consider and equipment. Summary of presentation by Andreas Valentin at the European Society of Intensive Care Medicine congress in Berlin, October 2015.



























