In patients undergoing cardiac surgery, the benefit of levosimendan in terms of survival was not shown in multicentre or in high-quality trials; however, levosimendan therapy was associated with reduced mortality in patients with preoperative ventricular systolic dysfunction, according to a new meta-analysis published in the journal Critical Care.
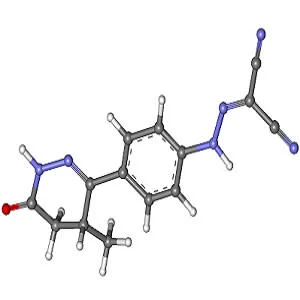
Levosimendan is an inotropic agent that enhances myocardial contractility without increasing myocardial oxygen demand in patients with low cardiac systolic dysfunction. Clinical studies have reported that levosimendan therapy improves survival in patients undergoing cardiac surgery. However, recently published large-scale trials did not provide evidence for this benefit.
The objective of this meta-analysis was to assess the survival benefits of levosimendan in patients undergoing cardiac surgery. Previous meta-analyses showed that patients with low ejection fraction (EF) benefit more from levosimendan therapy than patients with normal EF. Therefore, researchers performed subgroup analyses according to the preoperative EF of enrolled patients.
The analysis included 17 randomised clinical trials (2,756 patients) that investigated levosimendan therapy versus control in patients undergoing cardiac surgery. Individual patient data from each study were compiled. Meta-analyses were performed for primary outcomes, secondary outcomes and serious adverse events. The risk of bias was assessed using the Cochrane risk-of-bias tool.
Results of the analysis show that levosimendan therapy was associated with a significant reduction in 30-day mortality and reduced the risk of death in single-centre trials and in subgroup trials of inferior quality; however, in multicentre and in high-quality subgroup-analysis trials, no significant difference in mortality was observed between patients who received levosimendan therapy and controls.
The results also show that, in high-quality subgroup trials, levosimendan therapy was associated with reduced mortality in patients in a preoperative low-EF subgroup. Similarly, only patients in the preoperative low-EF subgroup benefited in terms of reduced risk of renal replacement therapy. Furthermore, levosimendan therapy was associated with a significant reduction in intensive care unit (ICU) length of stay.
"Levosimendan might improve renal function in cardiac surgery due to its ability to improve cardiac systolic function and systemic haemodynamics," the authors write. "In acute decompensated heart failure, levosimendan has an immediate renoprotective effect, which is mediated by an increase in renal blood flow resulting from selective renal arterial and venous vasodilating action. One study also indicated that levosimendan therapy induced vasodilation, preferentially of preglomerular resistance vessels, thereby increasing both renal blood flow and glomerular filtration rate without jeopardising renal oxygenation after cardiac surgery with cardiopulmonary bypass."
The improvement in cardiac systolic function induced by levosimendan is due to two mechanisms – vasodilation and increased contractility, the authors say. In this meta-analysis, postoperative hypotension was documented in four trials (1,600 patients). Pooled analysis showed no association between levosimendan and postoperative hypotension. A possible reason for this may be that the reduction in systemic vascular resistance is compensated for by an increased cardiac index.
"Since most of these hypotension episodes often occurred following the administration of a loading dose, hypotension may be avoided by eliminating the loading dose while the favourable haemodynamic effects of levosimendan can be obtained through continuous infusion," the authors explain.
Source: Critical Care
Image Credit: MarinaVladivostok
References:
Chen, Qi-Hong et al. (2017) Effect of levosimendan on prognosis in adult patients undergoing cardiac surgery: a meta-analysis of randomized controlled trials. Critical Care. doi.org/10.1186/s13054-017-1848-1
Latest Articles
cardiac surgery, mortality, Levosimendan, preoperative ventricular systolic dysfunction
In patients undergoing cardiac surgery, the benefit of levosimendan in terms of survival was not shown in multicentre or in high-quality trials; however, levosimendan therapy was associated with reduced mortality in patients with preoperative ventricular