Pancreatic ductal adenocarcinoma (PDAC) remains among the most lethal cancers globally due to its frequent late diagnosis and limited treatment options. While surgical resection offers the only curative potential, few patients qualify for this intervention at the time of diagnosis. Early detection through imaging is therefore paramount. Radiologists play a vital role in identifying early indicators of malignancy and monitoring conditions associated with elevated risk, including anatomical variants and cystic pancreatic lesions. Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) have become indispensable tools in this context, especially for high-risk individuals.
Recognising Early Imaging Signs of PDAC
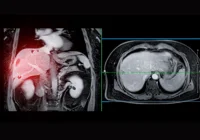
The nonspecific nature of PDAC symptoms often delays clinical diagnosis, underscoring the need for radiologists to detect early imaging markers. MRI outperforms CT in identifying small or isoattenuating pancreatic lesions, which are frequently missed on standard imaging protocols. Key early signs include main pancreatic duct (MPD) dilation, contour deformities, focal atrophy and the “double duct” sign—simultaneous dilation of the bile and pancreatic ducts. Retrospective studies have revealed that such indicators often appear on imaging months or even a year before clinical diagnosis. The presence of MPD calibre changes, focal pancreatic atrophy or pancreatic fat infiltration should prompt further evaluation through advanced imaging or endoscopic ultrasound.
Must Read: uPAR Immuno-PET: Advancing Pancreatic Cancer Imaging and Therapy
High-Risk Anatomical Variants and Lesions
Certain congenital and acquired pancreaticobiliary conditions increase PDAC risk. Pancreas divisum and annular pancreas are notable congenital variants, with the former occasionally linked to recurrent pancreatitis. More significantly, pancreaticobiliary maljunctions (PBM) have been associated with malignancy due to the reflux of pancreatic enzymes into the bile duct. MRI with MRCP sequences is the gold standard for evaluating these anomalies.
Cystic lesions also warrant attention. Intraductal papillary mucinous neoplasms (IPMNs), especially those involving the main duct or both main and branch ducts, carry a substantial risk of malignant transformation. Branch duct IPMNs (BD-IPMNs), although less aggressive, still present a tangible long-term risk. Features such as cyst size over 30–40 mm, mural nodules and MPD dilation over 10 mm signal higher malignancy potential. Mucinous cystic neoplasms (MCNs), predominantly found in women, typically present as solitary cysts in the pancreatic body or tail and also harbour malignant potential. Imaging characteristics, including cyst wall thickening and the presence of enhancing nodules or septations, help differentiate MCNs from benign entities.
Surveillance and Screening in High-Risk Populations
Given the impracticality of general population screening due to low disease prevalence and high cost, focus has shifted to surveillance in genetically predisposed individuals or those with significant family history. Guidelines recommend alternating MRI with MRCP and endoscopic ultrasound for such patients. Studies have shown higher detection rates of early-stage, resectable cancers within these groups when enrolled in regular surveillance programmes.
However, full MRI protocols are time-consuming, often exceeding 30 minutes, which challenges their routine application. To mitigate this, abbreviated MRI protocols have been proposed, reducing scan times to 15–20 minutes by excluding certain sequences. These streamlined approaches are especially effective in follow-ups for cystic lesions like IPMNs. Emerging technologies such as artificial intelligence and radiomics may further enhance early detection by enabling opportunistic screening on routine imaging performed for unrelated indications.
Effective early detection of PDAC hinges on the radiologist’s ability to identify subtle changes suggestive of malignancy in at-risk individuals. MRI remains the imaging modality of choice for evaluating and monitoring pancreatic lesions, offering detailed assessment without radiation exposure. While screening the general population is not justified, targeted surveillance of high-risk individuals using tailored MRI protocols is crucial. Standardised reporting and incorporation of advanced imaging techniques promise to refine early diagnosis pathways and potentially improve survival outcomes in pancreatic cancer.
Source: European Journal of Radiology
Image Credit: iStock