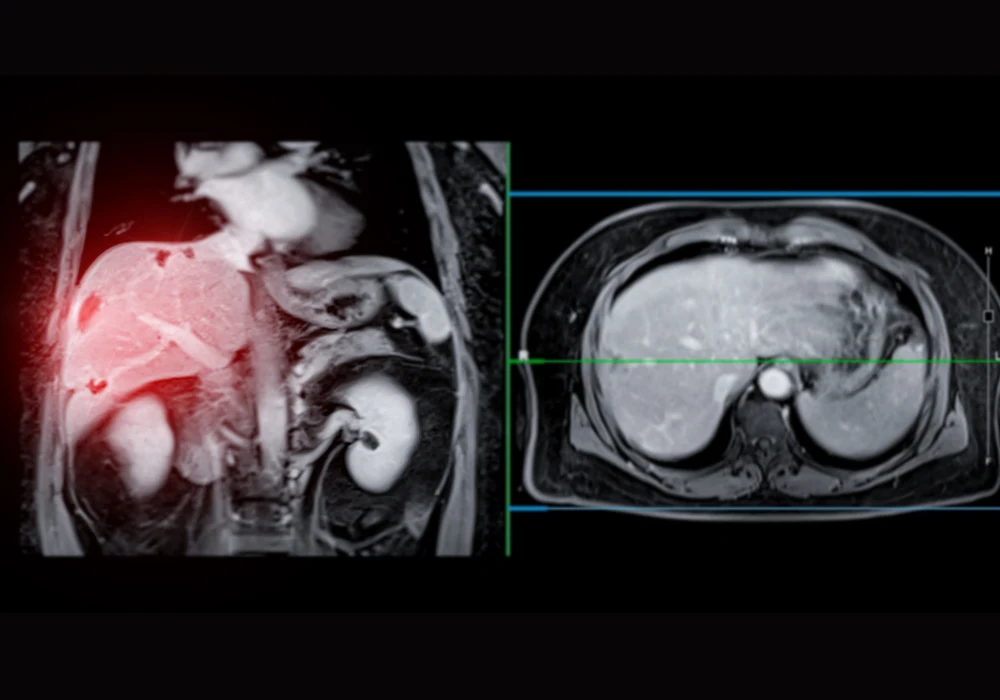
Magnetic resonance imaging (MRI) is a cornerstone of liver lesion detection, particularly when enhanced with gadoxetate disodium during the hepatobiliary phase. While high-field MRI systems at 1.5 T or 3 T have well-established flip angle (FA) protocols to maximise image quality, the rise of mid-field systems at 0.55 T—offering cost-efficiency, comfort and fewer artefacts—calls for tailored imaging parameters. In this context, determining the optimal FA for hepatobiliary imaging at 0.55 T is crucial, especially in patients with metastatic neuroendocrine tumours.
Establishing Theoretical and Clinical Benchmarks
To identify the most effective FA for liver imaging at 0.55 T, researchers initiated a study combining theoretical modelling with a prospective clinical trial. Initial signal intensity calculations, based on established MRI physics, predicted peak liver enhancement in the 23–28° range. These estimates laid the groundwork for clinical validation using actual patient data. From February to December 2023, fourteen patients with known or suspected metastatic neuroendocrine tumours underwent hepatobiliary-phase liver MRI using a low-field scanner. The protocol incorporated a series of T1-weighted VIBE sequences enhanced with deep learning denoising and Dixon water-fat separation, with FAs ranging from 10° to 70°.
Must Read: MRI Texture Analysis in Liver Biopsy Complications
To ensure robust assessment, radiologists blinded to the FA values placed regions of interest on dominant liver lesions, hepatic lobes and the portal vein. This allowed for the calculation of liver-lesion contrast, liver-vessel contrast and liver signal intensity, all expressed as normalised percentages relative to the maximum observed values per patient. These metrics were then statistically evaluated using Wilcoxon ranked-sum tests to identify significant performance differences between FA values.
Clinical Results and Interpretation
The study revealed that a FA of 30° consistently delivered superior liver-lesion and liver-vessel contrast. Specifically, liver-lesion contrast peaked at 97.7% at 30°, showing a marked improvement over both lower FAs (10–20°) and higher ones (40–70°). Similarly, liver-vessel contrast was highest at 30° (96.0%), surpassing other values, particularly those below 20° or above 60°. However, the highest liver signal intensity was recorded at a FA of 20°, where the value reached nearly 100%, suggesting that this angle may be preferable when pure liver signal clarity is the priority.
Importantly, while these findings align with prior research conducted at higher field strengths—which reported optimal FAs between 25° and 40° for image quality and lesion detection—the current study refines this understanding for the unique dynamics of 0.55 T systems. Notably, increased flip angles beyond 40° yielded diminishing returns, particularly for liver-lesion visibility, highlighting the non-linear relationship between FA and image contrast at lower field strengths.
Study Limitations and Practical Considerations
Despite offering valuable insights, the study's limitations should be acknowledged. The sample size was relatively small, with only 14 participants, of whom only five underwent imaging with FAs extending to 70°. Moreover, all patients had a similar lesion type, limiting broader generalisability. The design also did not incorporate sensitivity or specificity assessments, and contrast acquisitions were obtained sequentially, which may have introduced time-related bias in contrast uptake at higher FAs.
Another constraint involved the use of deep-learning denoising, which precluded consistent noise quantification. As a result, contrast-to-noise ratios (CNR) were not measured, and analysis focused instead on contrast between structures. However, these limitations do not undermine the relevance of the results for clinical practice, where image quality and lesion conspicuity remain the primary objectives.
The study successfully identified a FA of 30° as optimal for liver-lesion and liver-vessel contrast, and 20° for peak liver signal intensity, when performing hepatobiliary-phase imaging at 0.55 T using gadoxetate disodium. These findings not only provide practical guidance for radiologists adapting protocols for mid-field MRI systems, but also reaffirm the clinical viability of low-field imaging in oncology settings. As 0.55 T systems continue to gain traction due to their accessibility and comfort, such protocol refinements are essential to ensuring diagnostic accuracy does not come at the cost of reduced image quality.
Source: American Journal of Roentgenology
Image Credit: iStock