Invasive pulmonary aspergillosis (IPA) is a major cause of morbidity and mortality, particularly in patients with haematological malignancies. A delay in treatment is associated with substantially increased hospital mortality. However, treatment is expensive, and can have serious side effects. From a clinical point of view, there is therefore a strong need for prompt recognition and proper onset of treatment to ensure an optimal patient outcome. In this diagnostic dilemma, imaging still plays an important role.
Like with other lung diseases, computed tomography (CT) has been proven to be more sensitive than radiography in revealing subtle pathology. As such, the imaging criteria of the EORTC/MSG (European Organisation for Research and Treatment of Cancer, US Mycoses Study Group) guidelines for the presence of IPA refer to specific CT findings (dense, well-circumscribed lesions with or without a halo sign, air crescent sign, cavity). Also, the guidelines published by the Infectious Diseases Working Party of the German Society of Haematology and Oncology (AGIHO) in 2012 state that in patients with granulocytopenia, high resolution computed tomography (HRCT) should be preferred to chest x-ray for primary diagnosis in high-risk patients
Chest X-ray's Diagnostic Value is Limited by Low Sensitivity
Although CT is currently recommended as the preferred method if there is strong clinical suspicion of an infection, chest X-ray (CXR) remains the first-line imaging method because of its immediate availability and lower organisational demands. Also, guidelines by the American College of Radiology and the Infectious Disease Society of America mention chest radiography as the first-line method for the work up of a patient with neutropenic fever, but do emphasise the low sensitivity of CXR.
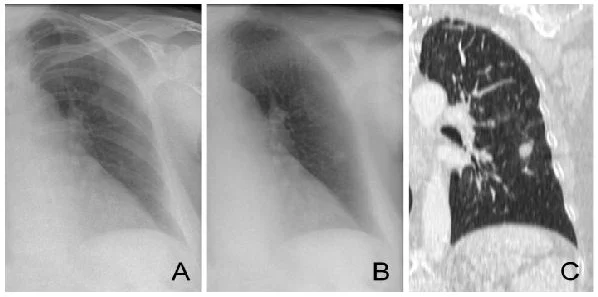
Early recognition of IPA on CXR would trigger an immediate CT examination of the patient in order to render morphology and accelerate the diagnosis, providing a chance to hasten the onset of treatment. By using an advanced image processing solution called bone suppression imaging (BSI), this study aimed to increase the value of chest radiographs (CXR) in the diagnostic workup of neutropenic patients who are suspected of IPA. If BSI would improve detection of IPA, and so possibly avoid delay in treatment, it could result in an optimised use of CXR in immunocompromised patients at risk of developing IPA.
Methods and Materials for the Observer Study
The frontal CXRs of 105 suspected cases of IPA were retrospectively retrieved from the image archives of four hospitals (three academic and one non-academic hospital) and anonymised. Radiographs could contain single or multiple sites of infection. The diagnoses of invasive aspergillus as an underlying disease were taken from the clinical patient charts and included the presence of typical CT findings in all diseased patients. Neutropenic patients with signs of fever with a normal chest radiograph functioned as control subjects. The absence of disease in these control subjects was confirmed by a negative CT after the CXR. Both upright as well as bedside acquisitions were included.
Five radiologists (with 3-17 years of experience) and two residents (third and fifth year of residency) participated in an observer study for the detection of IPA on CXRs with and without bone suppressed images (ClearRead BSI 3.2; Riverain Technologies). This software solution suppresses bone structures in chest x-rays, which can obscure abnormalities. Both the original and bone suppressed images can be visualised side by side or as a stack of two images. Both images are equivalent in terms of size and gradation characteristics, with the exception of overlying rib structures.
For each image, observers scored the likelihood of focal infectious lesions being present on a continuous scale (0 = not suspicious, 100 = very suspicious). Cases that were assigned an average score above 75 were classified as obvious cases, between 50 and 75 as moderately subtle cases, below 50 but higher than 25 as subtle cases, and below 25 as very subtle cases. The area under the receiver operating characteristics curve (AUC) served as the performance measure. Sensitivity and specificity were calculated by considering only the lungs with a suspiciousness score of greater than 50 to be positive.
Results Show Higher CXR Sensitivity with Bone Suppression
Of the total 105 suspected cases, there were 78 diseased lungs and 132 normal lungs. Radiographs of 128 lungs were obtained upright, and 82 lungs were acquired at the bedside. With respect to the conspicuity of pathology, diseased lungs were classified as being obvious in 17, moderately subtle in 21, subtle in 15, and very subtle in 25 cases.
The average AUC for only CXRs was 0.815. Performance significantly increased, to 0.853, when evaluation was aided with BSI (p = 0.01). Sensitivity increased from 49 percent to 66 percent with BSI, while specificity decreased from 95 percent to 90 percent.
Also, an analysis for the different subsets of subtlety classification based on reader scores showed that the very subtle cases benefitted the most from BSI. The AUC for very subtle cases increased from 0.579 to 0.659 (p = 0.02), AUC for subtle cases increased from 0.809 to 0.856 (p = 0.07). For the detection of moderately subtle and obvious cases baseline performance was already very good (AUC = 0.954 and 0.995, respectively) and did not significantly increase with BSI (0.968 and 0.992, p = 0.26 and p = 0.44, respectively).
Conclusion
The detection of IPA in CXRs can be improved when their evaluation is aided by bone suppressed images. BSI improved the sensitivity of the CXR examination, outweighing a small loss in specificity. Despite its inferiority to CT, CXR still represents an important role in the workup of febrile neutropenic patients, serving as a diagnostic screening procedure that is readily available, relatively easy to perform and providing immediate diagnostic information.
Prospective studies will have to prove the impact of a substantially improved radiographic technique on the role of radiography in diagnosing IPA more promptly and triggering CT examinations for further morphological analysis.
Image Credit: National Center for Biotechnology Information, US National Library of Medicine
Like with other lung diseases, computed tomography (CT) has been proven to be more sensitive than radiography in revealing subtle pathology. As such, the imaging criteria of the EORTC/MSG (European Organisation for Research and Treatment of Cancer, US Mycoses Study Group) guidelines for the presence of IPA refer to specific CT findings (dense, well-circumscribed lesions with or without a halo sign, air crescent sign, cavity). Also, the guidelines published by the Infectious Diseases Working Party of the German Society of Haematology and Oncology (AGIHO) in 2012 state that in patients with granulocytopenia, high resolution computed tomography (HRCT) should be preferred to chest x-ray for primary diagnosis in high-risk patients
Chest X-ray's Diagnostic Value is Limited by Low Sensitivity
Although CT is currently recommended as the preferred method if there is strong clinical suspicion of an infection, chest X-ray (CXR) remains the first-line imaging method because of its immediate availability and lower organisational demands. Also, guidelines by the American College of Radiology and the Infectious Disease Society of America mention chest radiography as the first-line method for the work up of a patient with neutropenic fever, but do emphasise the low sensitivity of CXR.
Early recognition of IPA on CXR would trigger an immediate CT examination of the patient in order to render morphology and accelerate the diagnosis, providing a chance to hasten the onset of treatment. By using an advanced image processing solution called bone suppression imaging (BSI), this study aimed to increase the value of chest radiographs (CXR) in the diagnostic workup of neutropenic patients who are suspected of IPA. If BSI would improve detection of IPA, and so possibly avoid delay in treatment, it could result in an optimised use of CXR in immunocompromised patients at risk of developing IPA.
Methods and Materials for the Observer Study
The frontal CXRs of 105 suspected cases of IPA were retrospectively retrieved from the image archives of four hospitals (three academic and one non-academic hospital) and anonymised. Radiographs could contain single or multiple sites of infection. The diagnoses of invasive aspergillus as an underlying disease were taken from the clinical patient charts and included the presence of typical CT findings in all diseased patients. Neutropenic patients with signs of fever with a normal chest radiograph functioned as control subjects. The absence of disease in these control subjects was confirmed by a negative CT after the CXR. Both upright as well as bedside acquisitions were included.
Five radiologists (with 3-17 years of experience) and two residents (third and fifth year of residency) participated in an observer study for the detection of IPA on CXRs with and without bone suppressed images (ClearRead BSI 3.2; Riverain Technologies). This software solution suppresses bone structures in chest x-rays, which can obscure abnormalities. Both the original and bone suppressed images can be visualised side by side or as a stack of two images. Both images are equivalent in terms of size and gradation characteristics, with the exception of overlying rib structures.
For each image, observers scored the likelihood of focal infectious lesions being present on a continuous scale (0 = not suspicious, 100 = very suspicious). Cases that were assigned an average score above 75 were classified as obvious cases, between 50 and 75 as moderately subtle cases, below 50 but higher than 25 as subtle cases, and below 25 as very subtle cases. The area under the receiver operating characteristics curve (AUC) served as the performance measure. Sensitivity and specificity were calculated by considering only the lungs with a suspiciousness score of greater than 50 to be positive.
Results Show Higher CXR Sensitivity with Bone Suppression
Of the total 105 suspected cases, there were 78 diseased lungs and 132 normal lungs. Radiographs of 128 lungs were obtained upright, and 82 lungs were acquired at the bedside. With respect to the conspicuity of pathology, diseased lungs were classified as being obvious in 17, moderately subtle in 21, subtle in 15, and very subtle in 25 cases.
The average AUC for only CXRs was 0.815. Performance significantly increased, to 0.853, when evaluation was aided with BSI (p = 0.01). Sensitivity increased from 49 percent to 66 percent with BSI, while specificity decreased from 95 percent to 90 percent.
Also, an analysis for the different subsets of subtlety classification based on reader scores showed that the very subtle cases benefitted the most from BSI. The AUC for very subtle cases increased from 0.579 to 0.659 (p = 0.02), AUC for subtle cases increased from 0.809 to 0.856 (p = 0.07). For the detection of moderately subtle and obvious cases baseline performance was already very good (AUC = 0.954 and 0.995, respectively) and did not significantly increase with BSI (0.968 and 0.992, p = 0.26 and p = 0.44, respectively).
Conclusion
The detection of IPA in CXRs can be improved when their evaluation is aided by bone suppressed images. BSI improved the sensitivity of the CXR examination, outweighing a small loss in specificity. Despite its inferiority to CT, CXR still represents an important role in the workup of febrile neutropenic patients, serving as a diagnostic screening procedure that is readily available, relatively easy to perform and providing immediate diagnostic information.
Prospective studies will have to prove the impact of a substantially improved radiographic technique on the role of radiography in diagnosing IPA more promptly and triggering CT examinations for further morphological analysis.
Image Credit: National Center for Biotechnology Information, US National Library of Medicine
References:
Schalekamp S, van Ginneken B, van den Berk I A H, Hartmann I J C,
Snoeren M M, Odink A E, van Lankeren W, Pegge S A H, Schijf L J,
Karssemeijer N, Schaefer-Prokop C M (2014) Bone Suppression Increases
the Visibility of Invasive Pulmonary Aspergillosis in Chest Radiographs.
PLoS One. 2014; 9(10): e108551. PMCID: PMC4184785
Latest Articles
CT, X-ray, radiography, chest, aspergillosis
Invasive pulmonary aspergillosis (IPA) is a major cause of morbidity and mortality, particularly in patients with haematological malignancies. A delay in t...