Dr. Ulf Guenther from Germany made an excellent presentation today at Euroanaesthesia 2019 #EA19 on assessing delirium in the ICU. Dr. Guenther has spent a large part of his research career dealing with delirium, and he shared his insight with respect to the clinical impact, diagnosis, risk factors, and management of delirium in the ICU.
According to Dr. Guenther, acute inattention is the core feature of delirium that clinicians must prove or exclude when determining if a patient has delirium. He pointed out that as patients grow older, the risk of delirium in such patients increases if they undergo surgery. Dementia, for example, is the most severe variant of cognitive dysfunction. The rate of dementia will inevitably increase because people are not only getting older, they are also getting higher rates of cognitive deficiency. People with impaired cognitive function are at high risk of delirium postoperatively.
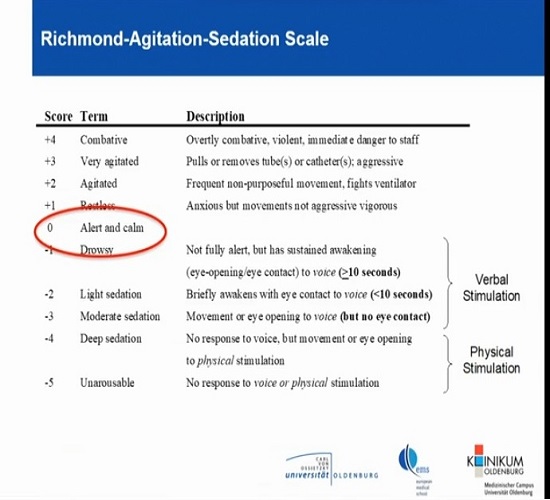
Dr. Guenther discussed the Richmond Agitation Sedation Scale (RASS) that is used to measure agitation or sedation in hospitalised patients, and that helps describe their level of alertness or agitation. Obtaining the RASS score is the first step in administering the Confusion Assessment Method in the ICU (CAM-ICU), a tool that is used to detect delirium in intensive care unit patients.
Dr. Guenther also explained how one could figure out if a patient is suffering from inattention. He explained that you could approach the patient, ask them to squeeze your hand; and then you can go further with your test and ask them to squeeze your hand when you read out the letter A. You can use words like SAVEAHAART or CASABLANCA but you should not read out the word; just read out the letters, says Dr. Guenther. If the patient makes two errors, he is okay, but if you observe more than two errors, you have more or less proven inattention. Also, he advised that it is important to make sure that this inattention is acute and is a new onset feature. If a patient already suffers from dementia, they would not be able to perform this test.
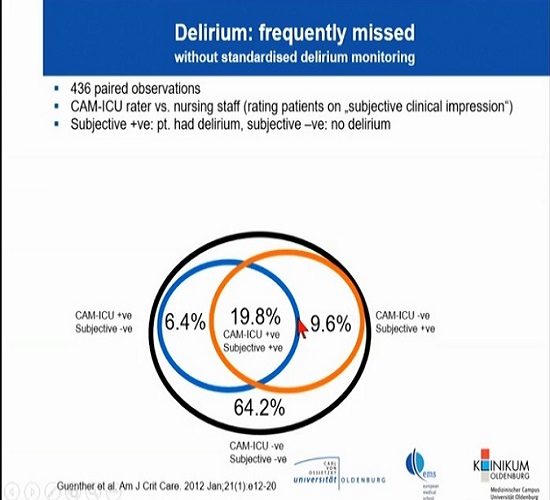
According to Dr. Guenther, subjective assessment of delirium is not as accurate as one that is based on the CAM-ICU tool. He highlighted the findings of a study which compared subjective evaluation with CAM-ICU results, and there was a significant difference between the results. CAM-ICU agreed with clinical impression in only about 19.8% of cases. He emphasised on the importance of using the right tools and accurately assessing delirium because back in the day, when we did not have the CAM-ICU, patients received psychotropic medication without a proper diagnosis. Therefore, if you want to know whether the patient has delirium or not, you have to use proper tools such as the CAM-ICU which has high sensitivity of about 90% and specificity of nearly 100%. If the CAM-ICU tells you that the patient is not delirious, then its probably true.
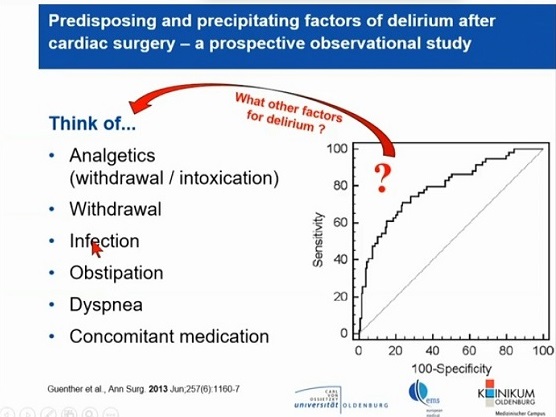
Dr. Guenther highlighted some major risk factors of delirium, which include old age, cognitive impairment, length of cardiopulmonary bypass, and the Charlson Co-morbidity Index. These are statistically independent factors of delirium and should be taken as such.
Other factors that could affect delirium include:
Finally, Dr. Guenther talked about the ABCDED bundle, an excellent strategy to be used when tackling this condition.
- Awake - even if a patient is sedated and requires sedation, you still need to wake up these patients to assess them and perform the wake-up test.
- Spontaneous Breathing which is always a goal in the ICU as we want to see a certain degree of spontaneous breathing
- Some units rely on Continuous use of benzodiazepines, which increases the risk of delirium. and also has an impact on delirium assessment and waking patients up.
- Delirium assessment, which is essential for proper management of these patients. Studies show that by introduce CAM-ICU in the intensive care unit, the use of haloperidol was reduced from 18 to 16mg.
- Early mobility is very important, and the goal should be to get patients out of bed as soon as possible. The alertness and vigilance of patients who are in an upright position is much higher than when they are lying in bed. Dr. Guenther pointed out that the culture of a unit changes if the default position of the patient is upright. Also, studies show that the length of delirium decreases from 4 days to 2 days in the early mobility group; the rate of patients leaving the hospital physically independent increases from 1/3 to almost 2/3 if efforts for early mobility are successfully made. It might be a lot of work, but it is worth it for the patients.
- It is important to include the Family and not underestimate the role they can play in improving patient outcomes. Dr. Guenther pointed out that family is helpless and they don’t touch anything because they have such respect for our work. We should try to involve them, and they can sometimes come up with very very interesting ideas.
In conclusion, Dr. Guenther highlighted the need to find a common language within your unit and a common style of sedating patients and treating pain, and you need to reduce the number of psychotropic drugs that are being used. You have to reduce the widespread use of certain drugs in your unit. This can help reduce the incidence of delirium and can also ensure patients experience early mobility and recovery in the ICU.
Source: Live coverage of Dr. Ulf Guenther's presentation
Image and slides credit: From live session of Dr. Ulf Guenther's presentation
Latest Articles
ICU, delirium, CAM-ICU, assessing delirium
Dr. Ulf Guenther from Germany made an excellent presentation today at Euroanaesthesia 2019 #EA19 on assessing delirium in the ICU. Dr. Guenther has spent...










