At this year’s Euroanaesthesia 2019 in Vienna, Austria, Prof. Caterina Aurilio (Naples, Italy), talked about acute pain management in the ICU. She started her presentation with the definition of pain as outlined by the International Association for the Study of Pain (IASP). Pain is an "unnecessary sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage."
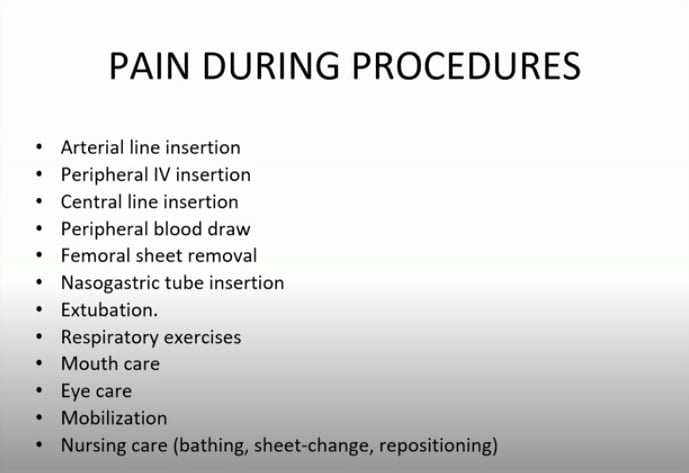
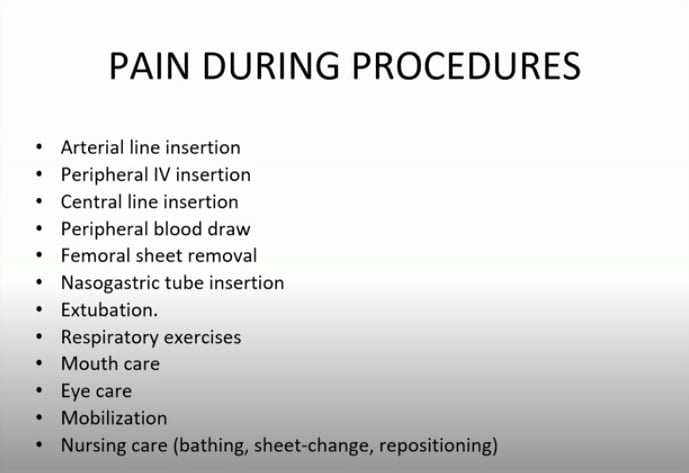
She highlighted the fact that critically ill patients often suffer from diverse comorbidities. In addition, pain could occur due to various causes, including trauma, post-surgical pain, burns, spastic, cancer, and/or neuropathic pain. Pain also occurs in many patients during procedures, some of which are outlined in the slide below:
Prof. Aurilio went on to talk about the baseline predictors of higher self-reported pain intensity during ICU admission. These included younger age, support to conduct daily activities, and the number of comorbidities. She highlighted the fact that despite the need for analgesia in ICU patients, many patients are undertreated. She mentioned findings from different clinical studies which demonstrated the incidence of pain in ICU patients.
In one study, 82% of the patients remembered pain or discomfort associated with the endotracheal tube; in another study, 82% of cardiac surgery patients reported pain as their most traumatic memory of the ICU one week after discharge, and 38% recalled pain as their most traumatic memory six months later. In yet another study, 17% of patients remembered experiencing severe pain six months after their ICU stay, and 18% were deemed to be at high risk of developing post-traumatic stress disorder (PTSD).
Prof. Aurilio also talked about measuring pain in the ICU. She talked about the NRS-V tool, which she said is the tool of choice for the ICU setting because it is the most feasible self-reporting scale for measuring the intensity of pain in critically ill patients.
For patients who cannot communicate, pain could be measured by using the critical care pain observation tool which evaluates the patient's facial expression, their body movements, their compliance with the ventilator, vocalisation, and muscle tension. Based on these factors, clinicians can determine if a patient is in pain or not, and if yes, what is the intensity of that pain.
As far as management of pain is concerned, Prof. Aurilio explained that opioids are the first line of treatment for pain in the ICU, but in the era of excessive use of opioids, it is important to be careful and to use a lower dose of opioids. That is because opioids increase the risk of delirium, and respiratory depression and can also increase the patient's length of stay in the ICU as well as have a negative impact on patient outcomes.
When talking about analgosedation, Prof. Aurilio talked about the use of ketamine in the ICU, and how it could decrease analgesic consumption in the ICU. Also, in patients who develop opioid tolerance and dependence, ketamine and magnesium could be used to provide analgesia and to prevent withdrawal. However, she pointed out that more trials are needed to further confirm the role of ketamine for analgosedation. Dexmedetomidine is another option, and it has an opioid-sparing effect which could benefit patients with morbid obesity and obstructive sleep apnoea. Use of dexmedetomidine infusion could help reduce the consumption of morphine, which could be beneficial, especially in patients with opioid-induced hyperalgesia.
In conclusion, Prof. Aurilio said that pain management in the ICU should not only address acute pain but should also aim to prevent the development of chronic postoperative pain and ongoing opioid use. So far, there is no single medication or technique that has proven to be the most effective in either acute pain management in the ICU or as a preventive measure for chronic pain. She also recommended the use of personalised pain management in the ICU and to use strategies that involve the lowest possible dose of opioids, with the aim of the earliest possible decline of the dose and slow transition to non-opioid medications.
Source: Prof. Catarina Aurilio's presentation at Euroanaesthesia 2019
Image Credit: Prof. Caterina Aurilio
Latest Articles
ICU, opioids, pain management, Acute Pain, euroanaesthesia 2019, #EA19
At this year’s Euroanaesthesia 2019 in Vienna, Austria, Prof. Caterina Aurilio talked about acute pain management in the ICU.










