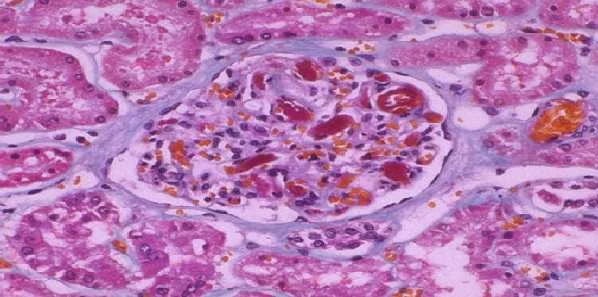
Based on results of a new study, high levels of two novel urinary biomarkers early in critical illness correlate with adverse long-term outcomes in patients with acute kidney injury (AKI). The combination of tissue inhibitor metalloproteinase-2 (TIMP-2) and IGF-binding protein-7 (IGFBP7) can identify patients with AKI who are at greater risk of death or requiring renal replacement therapy, such as dialysis or kidney transplant, over the next nine months.
The findings of the international, multicentre study led by the University of Pittsburgh School of Medicine are published online in the Journal of the American Society of Nephrology.
The two biomarkers are indicators of cell stress and injury, key components in the development of AKI, according to researchers. AKI is a condition that usually affects those in intensive care, and can occur hours to days after serious infections, surgery or taking certain medications.
"We found that not only do these biomarkers predict the development of AKI but, at high levels, they also tell us about long-term prognosis," said senior author John Kellum, MD, a critical care physician at UPMC and director of the Center for Critical Care Nephrology at the University of Pittsburgh. "This should greatly aid clinicians and researchers attempting to address this too-common complication."
For this study, Dr. Kellum's team enrolled 692 critically ill patients at 35 medical centres in Europe and North America. The primary analysis evaluated the outcomes of patients using a biomarker test (NeproCheck) within the first day of arrival into the intensive care unit. The team found strong associations between the biomarker combination and the risk of renal replacement therapy or death.
AKI is largely asymptomatic, lacking warning signs such as pain, shortness of breath or other clinical symptoms, particularly in the early stages when intervention is most beneficial, the research team explained. The incidence of AKI is high amongst critically ill patients, with up to 50 percent developing some degree of AKI during their illness, increasing the risk of death due to kidney failure.
In September 2014, the U.S. Food and Drug Administration (FDA) gave Astute Medical clearance for marketing the NephroCheck test, designed to predict the risk of sudden kidney injury within 12 hours. The FDA's review included two clinical studies evaluating the test's safety and effectiveness. The studies compared the clinical diagnoses of more than 500 critically ill subjects at 23 hospitals to NephroCheck test results. NephroCheck accurately predicted 92 percent of AKI cases in one study and 76 percent in the other, although it also incorrectly gave a positive result in about half of people without AKI, the FDA said.
Source: University of Pittsburgh Schools of the Health Sciences
Image Credit: Pixgood.com
The findings of the international, multicentre study led by the University of Pittsburgh School of Medicine are published online in the Journal of the American Society of Nephrology.
The two biomarkers are indicators of cell stress and injury, key components in the development of AKI, according to researchers. AKI is a condition that usually affects those in intensive care, and can occur hours to days after serious infections, surgery or taking certain medications.
"We found that not only do these biomarkers predict the development of AKI but, at high levels, they also tell us about long-term prognosis," said senior author John Kellum, MD, a critical care physician at UPMC and director of the Center for Critical Care Nephrology at the University of Pittsburgh. "This should greatly aid clinicians and researchers attempting to address this too-common complication."
For this study, Dr. Kellum's team enrolled 692 critically ill patients at 35 medical centres in Europe and North America. The primary analysis evaluated the outcomes of patients using a biomarker test (NeproCheck) within the first day of arrival into the intensive care unit. The team found strong associations between the biomarker combination and the risk of renal replacement therapy or death.
AKI is largely asymptomatic, lacking warning signs such as pain, shortness of breath or other clinical symptoms, particularly in the early stages when intervention is most beneficial, the research team explained. The incidence of AKI is high amongst critically ill patients, with up to 50 percent developing some degree of AKI during their illness, increasing the risk of death due to kidney failure.
In September 2014, the U.S. Food and Drug Administration (FDA) gave Astute Medical clearance for marketing the NephroCheck test, designed to predict the risk of sudden kidney injury within 12 hours. The FDA's review included two clinical studies evaluating the test's safety and effectiveness. The studies compared the clinical diagnoses of more than 500 critically ill subjects at 23 hospitals to NephroCheck test results. NephroCheck accurately predicted 92 percent of AKI cases in one study and 76 percent in the other, although it also incorrectly gave a positive result in about half of people without AKI, the FDA said.
Source: University of Pittsburgh Schools of the Health Sciences
Image Credit: Pixgood.com
References:
Kellum JA, Silenau FE, Murugan R et al. (2015) Classifying AKI by urine output versus serum creatinine level. JASN, Published online before print January 7, 2015, doi: 10.1681/ASN.2014070724
Latest Articles
Infections, AKI, kidney, Biomarkers, acute kidney injury, urinary
Based on results of a new study, high levels of two novel urinary biomarkers early in critical illness correlate with adverse long-term outcomes in patient...