ICU Management & Practice, Volume 17 - Issue 3, 2017
Optimising nutrition and metabolism post-ICU for recovery of functional lean body mass and quality of life.
In-hospital mortality following intensive care unit (ICU)
care has consistently declined in recent years (Kaukonen et al. 2014). However,
these data reveal many of these ICU “survivors” are not returning home to
functional lives after the ICU, but instead to rehabilitation and nursing home
settings where it is unclear if they ever returned to a meaningful quality of
life (QoL). As in-hospital ICU mortality has declined, we have markedly increased
the number of patients going to rehabilitation settings (Kaukonen et al. 2014).
Once in rehabilitation, it is unclear if these ICU “survivors” ever return home
as we know; ~40% of mortality within the first year of ICU stay occurs post-ICU
discharge (Weycker et al. 2003). Unfortunately for those who do survive, nearly
half the survivors will not return to work in the first year following discharge
(Kamdar et al. 2017), often as a result of post-intensive care syndrome (PICS) and
weakness post-ICU (Dinglas et al. 2017).
PICS is a multi-factorial syndrome;
however, a significant component of PICS is often post-ICU weakness. This is
unfortunately not surprising as we know critically ill burn patients lose as
much as a kilogram of lean body mass (LBM) per day (Stanojcic et al. 2016).
Other ICU patients also suffer significant LBM loss, much of it in the first
7-10 days of ICU stay (Wischmeyer 2016). Patients gain weight back following the
ICU, but virtually all this regained weight is fat mass, not functional muscle
and LBM (Herridge et al. 2003). This is not surprising, as data from the burned
ICU patients demonstrates the catabolic/hypermetabolic state brought on by
critical illness can persist for up to two years following hospital discharge
and markedly hinders recovery of QoL, muscle mass and function in our ICU patients
(Stanojcic et al. 2016).
To address this epidemic, we must ask ourselves in our ICU care, “Are we creating survivors or victims?” If we are going to begin creating more survivors we must improve our post-ICU care “recovery” care and take responsibility for the deficits in strength, function, and cognition we create in the ICU. We owe it to our ICU patients to optimise and further study key recovery interventions such as nutrition delivery post-ICU if we are to end the epidemic of PICS victims.
Metabolism and caloric needs for recovery after ICU
As patients improve and enter the “recovery phase”, seminal ICU metabolic cart data and landmark studies of starvation indicate caloric and protein intake needs to increase significantly (Uehara et al. 1999; Keys et al. 1950; Hoffer and Bistrian 2012). This should occur concurrently with implementation of aggressive rehabilitation and exercise interventions. Data from the landmark “Minnesota Starvation Study”, performed at the end of World War II (Kalm and Semba 2005; Keys et al. 1950) (a study all medical students and ICU caregivers should be taught or read themselves) provides fundamental data on the nutritional targets required to recover from the fundamental severe LBM loss observed after ICU. This seminal study demonstrates a healthy 70 kg human, following a significant weight loss, requires an average of 5000 kcal/day for 6 months–2 years to fully regain lost muscle mass and weight (Keys et al. 1950). Most all ICU and major surgery patients suffer similar marked weight and LBM loss. However, in addition to this significant LBM loss, ICU survivors also suffer prolonged hypermetabolism and catabolism (which Minnesota subjects did not have as they were healthy volunteers).
Thus, we must consider this additional challenge to recovery of functional LBM, and again emphasise significant calorie/protein delivery will be required to restore lost muscle mass and QoL. ICU metabolic cart studies demonstrate during the recovery phase post-ICU, the body has a marked increase in metabolic needs, with total energy expenditure (TEE) increasing as much as ~1.7-fold above resting energy expenditure (REE) (Uehara et al. 1999). In the 2nd week following sepsis this reveals caloric need (TEE) of ~3250 kcal/d or 47 kcal/kg/d. Interestingly this is virtually identical to WHO requirements for normal, healthy humans to maintain weight. In younger trauma patients (mean age: 34), this data indicated an even greater increase in caloric need (TEE) in the 2nd week post-injury to ~4120 kcal/d or 59 kcal/kg/d, nearly identical to the 4000 kcal/d Dr. Ansel Keys showed was required to recover from starvation in young subjects in the Minnesota study. Further, need for additional protein intake has been well-described by our research group and Hoffer et al. in a number of recent publications questioning whether it is actually protein deficit and not calorie deficit that is important to improving outcome in critical illness (Hoffer and Bistrian 2012; 2014; 2015) . This data demands we ask: Is it possible our septic patients have been unable to recover their QoL post-ICU for months to years (Needham et al. 2011; Wischmeyer and San-Millan 2015; Kamdar et al. 2017; Dinglas et al. 2017) due to our lack of understanding of their fundamental metabolic needs in different phases of illness, especially following ICU and hospital discharge?
How to optimise nutrition delivery after ICU for recovery
We must ask ourselves: “Will
patients leaving our ICU be able to consume adequate calories and protein to
optimally recover?” Unfortunately, in most cases the answer is a resounding
no!... At least not without help. Recovering patients, especially elderly
individuals, are challenged by decreased appetites, persistent nausea and
constipation from opiates, and lack of education about how to optimise their
diet. Further, dysphagia following ICU stay occurs in nearly 60% of patients
who are intubated in ICUs after extubation, and approximately 50% of these
suffer from aspiration (Brodsky et al. 2017). Recent data has shown these dysphagia
symptoms persist beyond hospital discharge in one-third of intubated ARDS survivors
(Brodsky et al. 2017). Dysphagia must be actively assessed for and treated in ICU
survivors. Thus, many challenges exist to recovery of oral intake post-ICU
discharge. Actual post-ICU oral caloric intake has been explored in ICU
patients in the week following extubation. An observational study demonstrated an
average spontaneous calorie intake of 700kcal/d and the entire population
studied consumed < 50% of calorie/protein needs for 7 days (Peterson et al.
2010). These data emphasise the importance of closely observing food intake in
post-ICU patients.
Given these data and the many challenges to oral intake, patients following ICU discharge are highly unlikely to take in the required calorie and protein delivery for recovery via routine oral intake. To address this, a large body of data demonstrates that oral nutrition supplements (ONS) must become fundamental in our post-ICU and hospital discharge care. A recent meta-analysis in a wide range of hospitalised patients demonstrated ONS reduce mortality, reduce hospital complications, reduce hospital readmissions, shorten length of stay and reduce hospital costs (Cawood et al. 2012; Elia et al. 2016; Stratton et al. 2013; 2003). A large hospital database analysis of ONS use in 724,000 patients matched with controls not receiving ONS showed a 21% reduction in hospital LOS and for every US$1 spent on ONS $52.63 was saved in hospital costs (Philipson et al. 2013). Finally, a recent large post-hospital discharge randomised controlled trial of 652 patients in 78 centres studied the effect of high protein ONS (HP-ONS) with β-Hydroxy β-Methylbutyrate (HP-HMB) versus placebo ONS in elderly malnourished (Subjective Global Assessment [SGA] class B or C) hospitalised adults for 90 days following hospital discharge. Results demonstrated that HP-HMB reduced 90-day mortality ~50% relative to placebo (4.8% vs. 9.7%; relative risk 0.49, 95% confidence interval [CI], 0.27 to 0.90; p = 0.018). The number needed to treat to prevent 1 death was 20.3 (95% CI: 10.9, 121.4) (Deutz et al. 2016). As it is well known that patients recovering from sepsis and the ICU will not consume sufficient calories and protein to recover optimally, the use of HP-ONS will be essential and is strongly recommended for all patients once oral intake is resumed for at least 3 months (up to 1 year) following ICU.
You might also like:Potential Nutritional Strategies to Reduce Muscle Wasting in Early Critical Illness
Role of specific anabolic/anti-catabolic agents, vitamin D
and microbiome/probiotics in recovery
Anabolic/anticatabolic agents
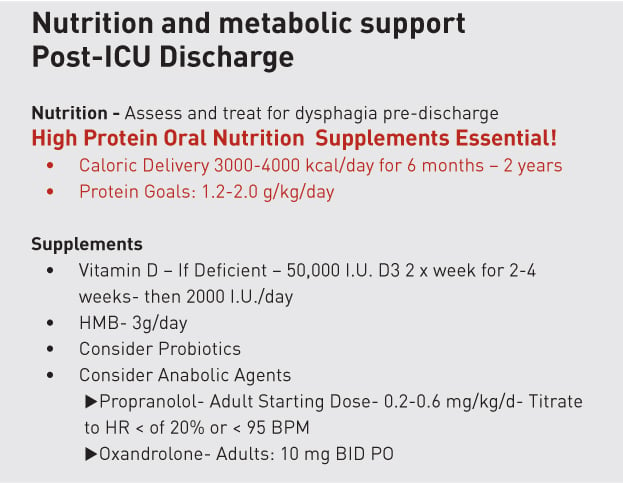
Data from the large HP-ONS trial using HMB above (Deutz et al. 2016) and other recent review articles (Stanojcic et al. 2016) emphasise that anabolic and anti-catabolic interventions, such as propranolol, oxandrolone and other agents targeted at restoring lean muscle mass (such as HMB) may be vital in optimal recovery and survival post-ICU. As shown in Table 1, it is likely targeted nutrition with adequate protein delivery and muscle recoverytargeted agents when combined with exercise will play a vital role in improving survival and recovery of QoL post-ICU (Wischmeyer and San-Millan 2015). The data for these novel anabolic/anti-catabolic agents are covered in detail by a recent review by Stanojcic and colleagues (Stanojcic et al. 2016). These interventions are summarised in Table 1.
Vitamin D
A rapidly growing body of data demonstrate a significant portion of the U.S. (and industrialised world) population is Vitamin D deficient (Holick 2007) and data in ICU and surgical patients show that Vitamin D deficiency has a significant relationship to postoperative complications and adverse ICU outcomes (Iglar and Hogan 2015; Higgins et al. 2012; Moromizato et al. 2014). A key recent RCT published in JAMA showed ICU patients with Vitamin D levels < 12 ng/ml experienced a significant improvement in hospital survival when vitamin D was aggressively supplemented (Vitamin D3 or placebo given orally or via nasogastric tube once at a dose of 540,000 IU followed by monthly maintenance doses of 90,000 IU for 5 months) (Amrein et al. 2014). This will be a difficult dose for many centres to administer if concentrated Vitamin D solutions are not available. Alternatively, a recent doubleblinded pilot RCT of 50,000 IU vitamin D3 or 100,000 IU vitamin D3 daily for 5 consecutive days enterally was conducted (Han et al. 2016). There was a significant decrease in hospital length of stay over time in the 50,000 IU D3 / day and 100,000 IU D3 /day groups compared to the placebo group (25 ± 14 and 18 ± 11 days compared to 36 ± 19 days, respectively; p = 0.03). Thus, vitamin D levels are recommended to be checked at ICU admission and once weekly after in all septic shock patients. A repletion dose of 100,000 units of Vitamin D3 for 5 days in the first week and once-twice weekly thereafter (monitoring levels) for the ICU stay in patients found to be deficient (< 30 ng/ml) is reasonable. Further, the emerging role for Vitamin D to reduce mortality in vitamin D deficient ICU patients has been recently reviewed by Christopher (2016). Correction of Vitamin D deficiency is essential for recovery of muscle mass and for optimising patient outcomes. In the post-ICU discharge setting, Vitamin D supplementation should consist of Vitamin D3 at 50,000 IU 2 x weekly for 2 weeks followed by 2000 IU/day. Larger trials on the role of vitamin D supplementation in sepsis and critical illness are currently underway.
Microbiome/probiotics
Finally, new data expanding our understanding of the microbiome in the ICU and “dysbiosis” therapies including probiotics and faecal microbiota transplantation have been described by our research group (Wischmeyer et al. 2016; McDonald et al. 2016). Dysbiosis results from many factors, including ubiquitous antibiotic use and overuse. Despite advances in antibiotic therapy, infections and mortality from often multidrug-resistant organisms (i.e. C. Difficile) are increasing. This raises the question of whether restoration of a healthy microbiome via probiotics or other “dysbiosis therapies” would be an optimal alternative, and should be a parallel treatment option with antibiotics. This may be particularly true as patients recover following ICU. Our research group’s recently published updated meta-analysis of 14 randomised controlled trials (RCT) found that probiotic therapy significantly reduced the incidence of infectious complications in the ICU (RR 0.80, 95% CI 0.68 to 0.95, p = 0.009) (Manzanares et al. 2016). Further, probiotics (Goldenberg et al. 2013) or faecal microbial transplantation (Kassam et al. 2013, Gupta et al. 2016) have been successful as an intervention in C. Difficile. Specifically, a meta-analysis looking at probiotic use for the prevention of C. Difficile-associated disease (CDAD) combined 23 studies and over 4,200 patients and found probiotics reduced CDAD incidence 64% and mitigated the side effects associated with the use of CDAD-specific therapy (Goldenberg et al. 2013). This contributes to recent recommendations that probiotics should be considered to prevent infection in ICU (criticalcarenutrition. com). It is possible that not only does a patient’s LBM and nutrition status need to be recovered, but also recovery of their microbiome may be required to optimise recovery. This may indicate that repletion or “re-sodding” of beneficial bacteria known to be lost following critical illness could begin to provide a targeted therapeutic avenue to pursue following ICU discharge.
Conclusions
In conclusion, we need to consider basic metabolism and historic understanding of starvation and recovery to employ targeted nutritional care to our critically ill patients as they recover following ICU discharge. If we are to optimise patient outcomes and start creating “survivors” we must optimise nutrition delivery post-ICU. It is clear that most patients will be unable to take in adequate nutrition using traditional oral “food”-based diets. It is essential we utilise high protein oral nutrition supplements (HP-ONS) to provide a realistic opportunity for our patients to achieve adequate calorie and protein delivery during the years required to recover functional lean body mass post-ICU discharge. We also must address issues such as dysphagia and need for targeted rehabilitation exercise efforts post-discharge. Finally, we must learn to target and incorporate nutritional therapies such as vitamin D, probiotics, and anabolic/anti-catabolic agents to optimise our patients’ chance to survive and thrive against all evolutionary odds. We have long known Mother Nature does not want our ICU patients to win this war and become “survivors…and not victims”. But, to begin winning this war on long-term ICU outcomes and give our patients back the lives they came to us to restore, we must ensure, especially post-ICU discharge, our patients get enough nutrition for enough time post-ICU discharge!
Conflict of interest
Paul Wischmeyer is an associate editor of Clinical Nutrition (Elsevier). He has received grant funding related to this work from the NIH NHLBI R34 HL109369, Canadian Institutes of Health Research, Baxter, Fresenius, Lyric Pharmaceuticals, Isomark Inc and Medtronics. Dr. Wischmeyer has served as a consultant to Nestle, Abbott, Fresenius, Baxter, Medtronics, Nutricia, and Lyric Pharmaceuticals, and Takeda for research related to this work. Dr. Wischmeyer has received honoraria or travel expenses for lectures on improving nutrition care in illness from Abbott, Fresenius and Medtronics.
Abbreviations
CDAD C. Difficile-associated disease
FMT faecal microbiota transplantation
HP-HMB β-Hydroxy β-Methylbutyrate
HP-ONS high protein oral nutrition supplements
ICU intensive care unit
ONS oral nutrition supplements
PICS post-intensive care syndrome
RCT randomised controlled trial
REE resting energy expenditure
QoL Quality of life
SGA subjective global assessment
TEE total energy expenditure
References:
Amrein K, Schnedl C, Holl A et al. (2014) Effect of high-dose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: the VITdAL-ICU randomized clinical trial. JAMA, 312: 520-30.
Brodsky MB, Huang M, Shanholtz C et al. (2017) Recovery from dysphagia symptoms after oral endotracheal intubation in acute respiratory distress syndrome survivors. A 5-year longitudinal study. Ann Am Thorac Soc, 14: 376-83.
Cawood AL, Elia M, Stratton RJ (2012) Systematic review and meta-analysis of the effects of high protein oral nutritional supplements. Ageing Res Rev, 11: 278-96.
Christopher KB (2016) Vitamin D and critical illness outcomes. Curr Opin Crit Care, 22: 332-8.
Deutz NE, Matheson EM, Matarese LE et al. (2016) Readmission and mortality in malnourished, older, hospitalized adults treated with a specialized oral nutritional supplement: A randomized clinical trial. Clin Nutr, 35: 18-26.
Dinglas VD, Aronson Friedman L, Colantuoni E et al. ( 2017) Muscle weakness and 5-year survival in acute respiratory distress syndrome survivors. Crit Care Med, 45: 446-53.
Elia M, Normand C, Norman K et al. (2016) A systematic review of the cost and cost effectiveness of using standard oral nutritional supplements in the hospital setting. Clin Nutr, 35: 370-80.
Goldenberg JZ, Ma SS, Saxton JD et al. (2013) Probiotics for the prevention of Clostridium difficile- associated diarrhea in adults and children. Cochrane Database Syst Rev, 5: CD006095.
Gupta S, Allen-Vercoe E, Petrof EO (2016) Fecal microbiota transplantation: in perspective. Therap Adv Gastroenterol, 9: 229-39.
https://www.ncbi.nlm.nih.gov/pubmed/26929784
Han JE, Jones JL, Tangpricha V et al. (2016) High dose vitamin D administration in ventilated intensive care unit patients: a pilot double blind randomized controlled trial. J Clin Transl Endocrinol, 4: 59-65.
https://www.ncbi.nlm.nih.gov/pubmed/27419080
Herridge MS, Cheung AM, Tansey CM et al. (2003) One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med, 348: 683-93.
Higgins DM, Wischmeyer PE, Queensland KM et al. (2012) Relationship of vitamin D deficiency to clinical outcomes in critically ill patients. JPEN J Parenter Enteral Nutr, 36: 713-20.
Hoffer LJ, Bistrian BR (2012) Appropriate protein provision in critical illness: a systematic and narrative review. Am J Clin Nutr, 96: 591-600.
Hoffer LJ, Bistrian BR (2014) What is the best nutritional support for critically ill patients? Hepatobiliary Surg Nutr, 3: 172-4.
Hoffer LJ, Bistrian BR (2015) Energy deficit is clinically relevant for critically ill patients: no. Intensive Care Med, 41: 339-41.
Holick MF (2007) Vitamin D deficiency. N Engl J Med, 357: 266-81.
Iglar PJ, Hogan KJ (2015) Vitamin D status and surgical outcomes: a systematic review. Patient Saf Surg, 9: 14.
Kalm LM, Semba RD (2005) They starved so that others be better fed: remembering Ancel Keys and the Minnesota experiment. J Nutr, 135: 1347-52.
Kamdar BB, Huang M, Dinglas VD et al.; National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome Network (2017) Joblessness and lost earnings after ARDS in a 1-year national multicenter study. Am J Respir Crit Care Med, 27 Apr. doi: 10.1164/rccm.201611-2327OC
Kassam Z, Lee CH, Yuan Y et al. (2013) Fecal microbiota transplantation for Clostridium difficile infection: systematic review and meta-analysis. Am J Gastroenterol, 108: 500-8.
Kaukonen KM, Bailey M, Suzuki S et al. (2014) Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000-2012. JAMA, 311: 1308-16.
Keys A, Brozek J, Henschel A et al. (1950) The biology of human starvation, Vols. I–II. Minneapolis, MN: University of Minnesota Press.
Manzanares W, Lemieux M, Langlois PL et al. (2016) Probiotic and synbiotic therapy in critical illness: a systematic review and meta-analysis. Crit Care, 20: 262.
McDonald D, Ackermann G, Khailova L et al. (2016) Extreme dysbiosis of the microbiome in critical illness. mSphere, 1(4). pii: e00199-16. doi: 10.1128/mSphere.00199-16.
Moromizato T, Litonjua AA, Braun AB et al. (2014) Association of low serum 25-hydroxyvitamin D levels and sepsis in the critically ill. Crit Care Med, 42: 97-107.
Needham DM, Feldman DR, Kho ME (2011) The functional costs of ICU survivorship. Collaborating to improve post-ICU disability. Am J Respir Crit Care Med, 183: 962-4.
Peterson SJ, Tsai AA, Scala CM et al. (2010) Adequacy of oral intake in critically ill patients 1 week after extubation. J Am Diet Assoc, 110: 427-33.
Philipson TJ, Snider JT, Lakdawalla DN et al. (2013) Impact of oral nutritional supplementation on hospital outcomes. Am J Manag Care, 19: 121-8.
Stanojcic M, Finnerty CC, Jeschke MG (2016) Anabolic and anticatabolic agents in critical care. Curr Opin Crit Care, 22: 325-31.
Stratton R, Green C, Elia M (2003) Disease-related malnutrition: an evidence-based approach to treatment. Wallingford, UK: CABI Publishing.
Stratton RJ, Hébuterne X, Elia M (2013) A systematic review and meta-analysis of the impact of oral nutritional supplements on hospital readmissions. Ageing Res Rev, 12: 884-97.
Uehara M, Plank LD, Hill GL (1999) Components of energy expenditure in patients with severe sepsis and major trauma: a basis for clinical care. Crit Care Med, 27: 1295-302.
Weycker D, Akhras KS, Edelsberg J et al. (2003) Long-term mortality and medical care charges in patients with severe sepsis. Crit Care Med, 31: 2316-23.
Wischmeyer PE (2016) Are we creating survivors...or victims in critical care? Delivering targeted nutrition to improve outcomes. Curr Opin Crit Care, 22: 279-84.
Wischmeyer PE, McDonald D, Knight R (2016) Role of the microbiome, probiotics, and 'dysbiosis therapy' in critical illness. Curr Opin Crit Care, 22: 347-53.
Wischmeyer PE, San-Millan I (2015) Winning the war against ICU-acquired weakness: new innovations in nutrition and exercise physiology. Crit Care, 19 Suppl 3: S6.







