Switzerland is a country of 8.2 million
inhabitants, who mostly live outside one of
the six major cities: Zurich (384,786 inhabitants),
Geneva (191,557), Basel (174,491),
Lausanne (132,626), Berne (128,848) and
Winterthur (105,676) (Bundesamt für Statistik
2015). Switzerland is composed of 26 cantons
that enjoy a great deal of independence from the
federation. The jurisdiction of the emergency
service and hospital structure mainly lies with
these cantons (Wyss and Lorenz 2000), although
smaller cantons collaborate on many aspects.
For example, Basel University Hospital (its official
name translates as “University Hospital of
both Basels”) is a joint undertaking of the two
cantons Basel City and Basel Country.
Healthcare System
Every Swiss inhabitant, regardless of nationality,
is obliged to obtain healthcare insurance that in
its base tariff covers the costs of healthcare and
medication listed in a legal document. Insurance
for accidents, both during work or leisure,
is further provided through employers, who
insure their employees, usually with one of the
few major companies that provide this type of
coverage. The government subsidises insurance
fees for the needy.
The Swiss healthcare system is among the most
expensive in the world. In a 2006 comparison
of the costs of healthcare in OECD member
countries, Switzerland came second after the
United States, with average expenditure of 11.1%
of GDP on healthcare (OECD 2010). However,
in the most recent comparison of the quality
and performance of healthcare systems among
the 197 member states of WHO, Switzerland
was rated second in the overall quality of its
system (“attainment of WHO-goals”) and 20th
in performance (where quality is compared to
costs) (WHO 2000).
Emergency Medicine
As in most western countries, major emergency
rooms are usually part of a university hospital,
of which there are five in Switzerland: Basel,
Berne, Geneva, Lausanne and Zurich. In 2006
there were 138 hospital-based emergency rooms
in Switzerland, of which 21 (including the
five affiliated to a university) provide care to
more than 20,000 patients per year (Sanchez
et al. 2006).
As pre-hospital emergency services are largely
regulated (and often provided or commissioned)
by cantons, there is a great diversity of modes
of service. This article therefore focuses on the
situation and numbers from Berne.
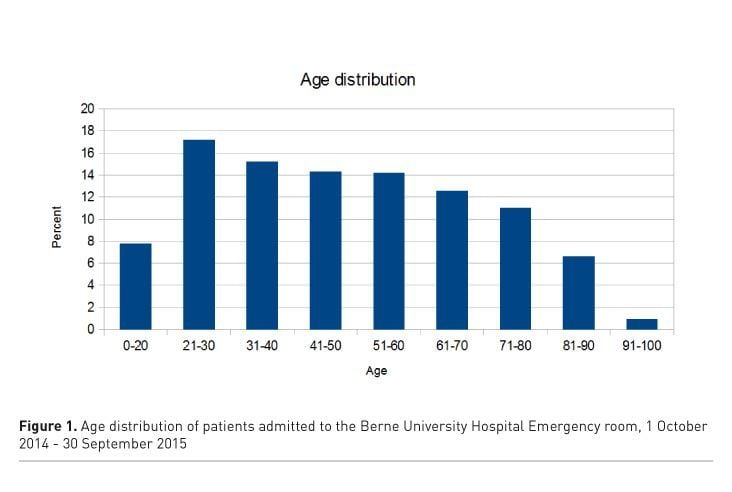
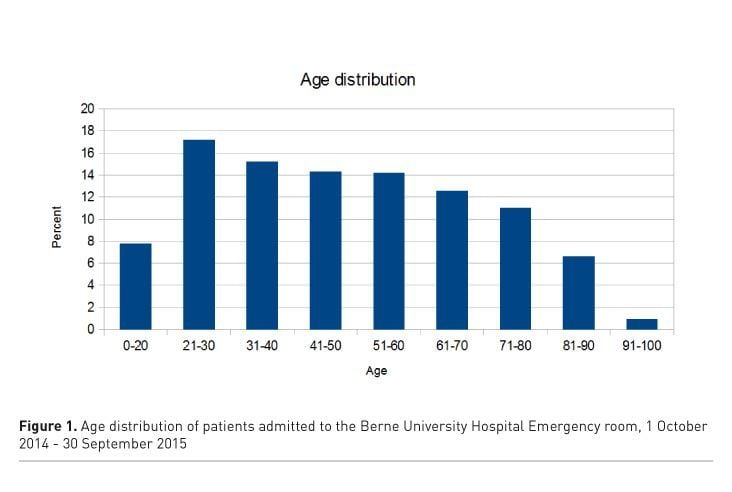
As the canton of Berne covers a large alpine
area and its
university hospital is the closest by
air to most of the Swiss Alps, patients injured
when farming the steep slopes or during sport
make up a comparatively large portion of emergency
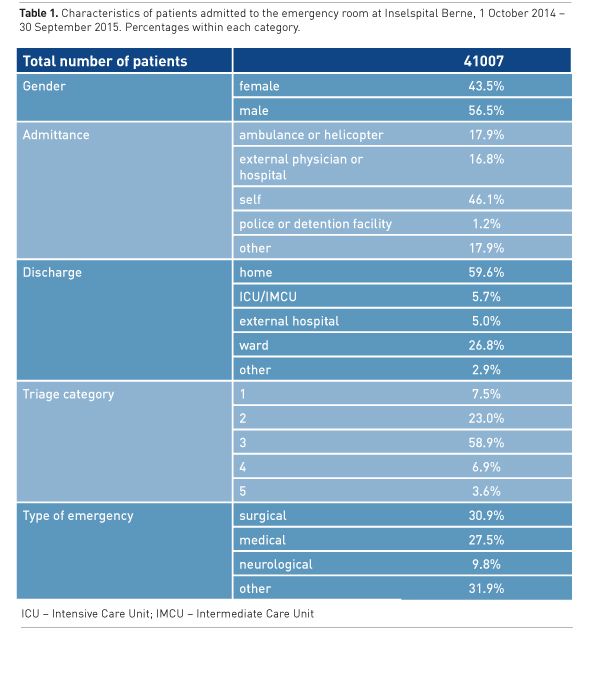
patients here (see Table 1), leading to a
relatively young population of patients (see
figure 1). This may further explain why caring
for hypothermic patients is comparatively common
in the Berne University emergency room.
Pre-hospital emergency service in the canton
of Berne is mainly provided by Rega and Air
Glacier (both providing a physician-staffed helicopter
rescue service) and the ‘Sanitätspolizei’
(translated as ‘rescue police’) on the ground.
The Sanitätspolizei staffs one car with an emergency
physician around the clock that can meet
the emergency medical service at the scene if needed, but paramedics in the usual rescue operation are fairly well
trained and are competent to provide a number of medical procedures
and treatments, including administering selected medications
or providing advanced airway management.
Once on their way to an emergency room, more seriously ill patients
are typically transported to one of the larger hospitals by the Sanitätspolizei.
Most patients in Swiss emergency departments, however,
are walk-in patients who present themselves (and most of the time
are treated and discharged: see Table 1). Around 60% of all patients
presenting to the emergency room in Berne are discharged home. Only
around 5.7% are admitted to the intensive or immediate care unit.
Intensive care specialists can typically expect a complete diagnostic
workup of patients transferred to the ICU, including collection of
microbial samples, calculated antibiotics, lumbar puncture and the
collection of procedural statements from all relevant disciplines. In
Berne, almost the only measure we omit in the emergency room is
inserting a central venous line into patients before admitting them
to the ICU, because doing so could limit the ICU's options for extended
haemodynamic monitoring, with either PICO catheters or a
pulmonary artery catheter, which is usually inserted together with
a central venous line.
Emergency Rooms
Most hospitals throughout Switzerland now operate as interdisciplinary
units, but there are still some older systems, in which patients are
separated along the lines of surgical care or internal medicine (Sanchez
et al. 2006). The emergency room at Berne University Hospital is an
interdisciplinary unit within the department of emergency medicine,
intensive care and anaesthesiology and sees all adult patients with an
interdisciplinary team. As in most other emergency rooms throughout
the country, patients are classified according to the urgency of their
treatment by specially trained nurses using a standardised triage model
(Hallas 2006; Hollimann et al. 2011). Urgent treatment (for around
7.5% of our patients) is usually provided within one of the three
shock rooms, while patients with minor complaints can be referred
to an integrated ‘fast lane’, staffed with one general practitioner from
8am to 10pm every day. Discharged patients can also be scheduled
to revisit within this fast lane concept.
Aside from patients who walk in or who are brought in through
an emergency service, the emergency room at Inselspital Berne sees
all non-planned patients referred to any of the specialities at the
University Hospital from an outside clinic. In total, we see more than
40,000 patients a year, with numbers continually rising for the last
five years. Around 18% of these patients are brought in by ambulance
or helicopter, slightly below half (46%) present themselves and the
remainder are referred to us from various sources, including external
hospitals, general practitioners, the police, psychiatric institutes or prisons (see Table 1). Those patients presented
by the police or referred from prisons are a
special feature of Berne, as the university hospital
here is the only one in Switzerland that
runs a specialised ward for detainees with all
medical care available.
Physician Education and Training
Current undergraduate teaching of emergency
medicine is rather sparse in Europe (Smith et
al. 2007). Education of physicians working in
emergency medicine in Switzerland is regulated
through the Swiss Society of Emergency and
Rescue Medicine (SSERM). It offers two types of
degrees, termed 'certificates of ability': one for
preclinical and one for clinical emergency medicine.
Both curricula are available online (sgnor.
ch/faehigkeitsausweise). While the certificate for
preclinical medicine is available to every physician
who has completed the three year curriculum,
the certificate for clinical emergency medicine
is only available once candidates have completed
residency and have obtained a degree in internal
medicine, surgery, anaesthesiology, intensive care,
orthopaedic surgery, traumatology or cardiology.
To obtain the certificate, one further needs to
participate in various courses (including Focused
Assessment with Sonography in Trauma (FAST),
Advanced Trauma Life Support® (ATLS) facs.
org/quality%20programs/trauma/atls and Advanced
Cardiovascular Life Support (ACLS)) and
complete an 18-month rotation in an accredited
emergency room. The curriculum is based on
the curriculum of the European Society of Emergency
Medicine (EUSEM), and the catalogue of
learning objectives is an adaptation of the English
Emergency Medicine specific learning objectives.
The degrees in clinical or preclinical emergency
medicine further require that the student passes a
final assessment. However, emergency medicine
is currently not available as a separate residency
training in Switzerland (Osterwalder 1998), and
the two certificates of ability do not substitute for
a residency programme, but may be completed
as part of a residency training. Maintenance of
certification requires physicians in Switzerland
to obtain a predefined number of credits for
continuous education activities, but currently
does not involve reassessments.
Acknowledgements
The authors would like to thank Meret Ricklin,
PhD and Sabina Uttiger, both from the Department
of Emergency Medicine at Inselspital Berne,
for providing data for this article.
See Also:
Critical Care in the Emergency Department
Bundesamt für Statistik (2015) Aktuellste provisorische
Monats- und Quartalsdaten. Bevölkerungsstand und -struktur – Indikatoren. [Accessed: 30 October 2015] Available from
bfs.admin.ch/bfs/portal/de/index/themen/01/02/blank/key/bevoelkerungsstand/01.html
Hallas P (2006) The effect of specialist treatment in
emergency medicine. A survey of current experiences. Scand J Trauma Resusc
Emerg Med, 14: 5–8.
Holliman CJ, Mulligan TM, Suter RE et al. (2011) The
efficacy and value of emergency medicine: a supportive literature review. Int J
Emerg Med, 4: 44.
OECD (2010) OECD
Gesundheitsdaten 2010. [Accessed: 28 August 2015] Available from
oecd.org/health/healthdata/
Osterwalder JJ (1998) Emergency Medicine in Switzerland. Ann
Emerg Med, 32(2): 243–7.
Sanchez B, Hirzel AH, Bingisser R et al. (2006) State of emergency medicine in Switzerland: a
national profile of emergency departments in 2006. Int J Emerg Med, 6(1): 23.
Smith CM, Perkins GD, Bullock I et al. (2007) Undergraduate
training in the care of the acutely ill patient: a literature review. Intensive
Care Med, 33(5): 901–7.
WHO (2010) The world health report 2000 - Health systems:
improving performance. [Accessed: 30 October 2015] Available from
who.int/whr/2000/en/
Wyss K, Lorenz N (2010) Decentralization and central and
regional coordination of health services: the case of Switzerland. Int J Health
Plann Manag, 15(2): 103–14.