ICU Management & Practice, Volume 22 - Issue 2, 2022
Sepsis and septic shock have been defined in 2016 (Singer et al. 2016) and the management of patients is framed by the Surviving Sepsis Campaign guidelines with its renewed version in 2021 (Evans et al. 2021). Using PubMed, around 15,000 hits respond to the word “sepsis” and “septic shock”, the best match being a review published by Angus and van der Poll in the New England Journal of Medicine in 2013.
As clinicians, we face sepsis and septic shock every day in our intensive care units (ICU). Despite our efforts, the 90-day mortality rate of these patients remains up to 40% in septic shock. We have to fight this high mortality with only antibiotics, one or two vasopressors and a few other drugs that the usefulness of which is still under debate. Each of us has probably their own view of sepsis, depending on several variables.
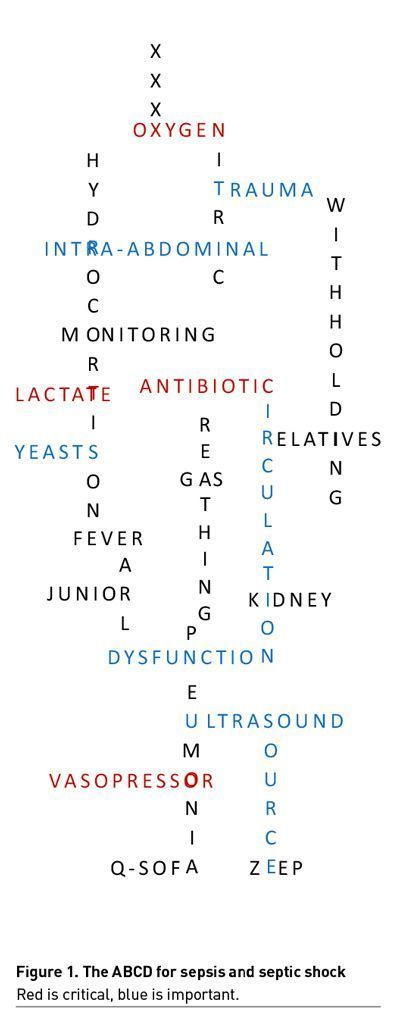
I provide, thereafter, my alphabet of sepsis and septic shock, based on personal choice. Some of my comments are not evidence-based but reflect my own clinical experience. This is a subjective approach, which does not rely on consensual process, Delphi rounds, or literature-based research.
The Sepsis Alphabet
A – Antibiotics are the key drugs in sepsis, regardless of the lack of randomised controlled trials on their use. They are used either as empirical treatment or as guided treatment, depending on the availability of the microbiological results. In septic shock, they should be administered as soon as possible after diagnosis and sampling (Evans et al. 2021). There is still a debate in sepsis in which few studies suggested an association between early administration and good outcomes (Rüddel et al. 2022), while others showed that a short delay - 4 to 6 hours - may be acceptable (Nauclér et al 2021). The balance between an overuse leading to resistance emergence and a strategy of large coverage for patients with suspected sepsis is a daily challenge in the ICU.
Others: albumin; antifungals.
B – Breathing is disturbed in most septic episodes. Increased respiratory rate is a clinical marker of sepsis in several scoring systems, including the concept of systemic inflammatory response syndrome and the quick sequential organ failure assessment (q-SOFA) score. This symptom should be regarded with attention for the diagnosis of sepsis, and one should keep in mind that it does not always refer to pneumonia.
Others: base excess; beta-lactams; biomarkers; bundle.
C – Circulation is the cornerstone differentiating sepsis and septic shock. The definition of septic shock is a sepsis associated with a vascular failure requiring the introduction of vasopressors and an increased plasma concentration of lactate (Singer et al. 2016). It is a circulatory shock inducing a vasoplegia. However, microcirculation may be impaired in a relative proportion of patients with sepsis (Joffre et al. 2020).
Others: carbapenems; cardiac; catecholamines; coagulopathy; confusion; crystalloids; colloids.
D – Dysfunction of organ(s) defines the sepsis, based on an increase in the SOFA score (Singer et al. 2016). This score reflects the degree of injury of organs, facilitating the decision-making for clinicians. At the bedside, the number of organs with dysfunction is probably one of the most relevant predictors of outcomes. However, the “multiple organ dysfunction syndrome” should not be used as cause of death, because this syndrome just reflects another initial injury that has to be clearly identified.
Others: de-escalation; delivery; dobutamine.
E – Early identification of sepsis is a critical step to improve the outcomes of patient. A large literature supports that early identification of sepsis, early source control and early antibiotic treatment are critical to save lives of patients with sepsis and septic shock (Evans et al. 2021). Different scores like the q-SOFA or strategies, including the use of point-of-care-ultrasound (Zieleskiewicz et al. 2021), may facilitate an early diagnosis. However, while guidelines look for providing specific timing for each step of the management, the word “early” should rather reflect “as soon as possible”.
Others: echocardiography; ECMO; epinephrine; examination.
F – Fever is found in most - but not all - patients with sepsis. Fever is one of the variables defining inflammation syndrome (Walter et al. 2016). However, not all patients with sepsis develop fever and those with hypothermia may have worse outcomes. In addition, not all patients with fever have sepsis – a large number have inflammation, cancer-related fever, drug-induced fever, etc. Finally, the fever control in sepsis is an unresolved issue, but a bunch of experimental literature suggest against treating it in these patients. Fever is a critical symptom, but this sign can lead to treatments in excess.
Others: fibrillation; fludrocortisone; fluid; fluoroquinolone.
G – Gas exchanges are impaired in patients with septic shock mainly due to metabolic acidosis. It is critical in a patient developing sepsis to pay attention to gas exchange by sampling arterial blood. A fine knowledge of gas exchange is a mandatory step to manage the patients with sepsis and septic shock.
Others: gender; glycopeptides; gram.
H – Hydrocortisone may be used to compensate a relative deficit in steroid production in patients with sepsis. This drug is recommended in patients with a severe vascular failure not responding to first-line vasopressors (Evans et al. 2021). However, despite 20 years of intense research, there is still no consensus on its use in septic shock, with positive randomised controlled trials contradicting negative ones. However, low-doses of hydrocortisone are largely used in patients with septic shock (Téblick et al. 2019).
Others: heat shock protein; hypotension; hypothermia; hypoxia.
I – Intra-abdominal infection is often identified as the second or third source of infection (Martin-Loeches et al. 2019). This source of infection should be evoked for each patient who develops sepsis without evident site of infection. A delay in diagnosis may lead to delayed source control, resulting in worsened outcome. Of note, intra-abdominal infection is often diagnosed in patients with acute respiratory failure with bilateral basal images on chest x-ray, and then, the wrong diagnosis of pneumonia may cause a fatal delay for the source control.
Others: insulin; interleukin(s).
J – Juniors should be the target to increase awareness about sepsis in the medical community. We need to sensitise these young doctors to recognise and manage patients with sepsis, which remains an under-known and under-diagnosed syndrome. Education of junior doctors is probably a step to improve patient outcomes in sepsis.
K- Kidney function is impaired in a large number of patients with sepsis (Pickkers et al. 2021). It should be determined by using the adequate method. In ICU, the different calculated formula should not be used to assess the creatinine clearance. Creatinine clearance should be measured on the urine collected during 8 to 24 hours using the formula "urine creatinine/plasma creatinine x volume of urine). Acute kidney failure is a strong predictor of long-term outcomes (Al-Dorzi et al. 2021).
Others: kaliaemia.
L – Lactate is the most useful biomarker in sepsis and septic shock (Evans et al. 2021). A serum concentration above 2.0 mmol/L is a variable included in the definition of septic shock (Singer et al. 2016). The increase is due to an imbalance between the needs and the inputs of oxygen to cells, resulting in an anaerobic pathway. However, intensivists should keep in mind that serum concentration of lactate remains the product of its production and its elimination. Thus, in patients with other sources of production, such as muscles (due to epinephrine infusion) (Levy et al. 2015), or those with a decreased elimination, such as those with liver disease, the interpretation of an increased serum lactate deserves a fine analysis. Serum lactate should thus be measured if there is the slightest doubt.
Others: liver; lung.
M – Monitoring is defined as the maintenance of regular surveillance over time. The level of monitoring required in sepsis and septic shock remains conflicting. It seems safe to use continuous monitoring of arterial pressure in patients at risk of haemodynamic instability (Evans et al. 2021). The use of continuous monitoring of cardiac output is under debate, although a majority of experts would support this statement in septic shock. However, only the devices based on thermodilution seem reliable in these patients (Monnet and Teboul 2017).
Others: mediators; metabolism; microcirculation; mitochondria; mortality.
N – Nitric oxide, a free radical, is the mediator responsible for vasodilation at the level of endothelium. Its production is related to the pro-inflammatory response and activates the GMPc pathway, which results in the dephosphorylation of myosin phosphatase. Its “chemical” inhibition was assessed in a large randomised controlled trial that found an increased mortality in the group receiving the inhibitor of nitric oxide (López et al. 2004). The reasons for this failure - hypertension in the intervention group, other roles of nitric oxide, etc – are not clearly elucidated.
Others: norepinephrine.
O – Oxygen may be found abundantly in patients with septic shock, but its use is impaired at the cell level due to several mechanisms including mitochondrial and microcirculatory injuries. This results in poor utilisation of circulating oxygen, and possible high concentration of oxygen found in mixed venous blood samples or superior cava vena blood samples. The elevated values of oxygen central venous saturations have been associated with impaired outcome (Textoris et al. 2011). However, the best management of patients with elevated oxygen central venous saturations remains a matter of debate.
Others: outcome.
P – Pneumonia is the first cause of infection in the ICU and the first source of sepsis. Different types of pneumonia are defined including community-acquired and hospital-acquired that includes ventilator-associated pneumonia. The definition of pneumonia is based on an evolutive image in the context of infection (Leone et al. 2018). Its management is framed by several guidelines. However, the diagnosis of infection is challenging, which results in frequent mistakes and treatments in excess.
Others: parasites; patient; penicillin; plasmodium; procalcitonin; pyuria.
Q – Q-SOFA has been suggested to diagnose sepsis in outpatients and in-ward patients. It consists of three variables including mental status, blood pressure and respiratory rate (Seymour et al. 2016). It should serve as a red flag to identify the patients at risk of sepsis to decide both the best treatment, the source control and the admission to ICU. However, the use of this score outside the field of ICU is disappointing.
Others: quality.
R – Relatives of patients with sepsis need attention. This syndrome, despite having a high mortality rate, remains unknown by the public at large. The concept of severe infection reaching several organs and leading to organ dysfunction is difficult to understand, especially in patients with no significant prior medical history. Good communication skills are required and rely on efficient training (Davidson et al. 2017).
Others: reactive oxygen species; responders; resistance.
S – Source control, which consists of the reduction of the physical process of infection, is a critical step in the management of septic patients (Martin-Loeches et al. 2019). Any delay, if source control is feasible, is associated with impaired outcome. Mini-invasive procedures should be preferred in those patients.
Others: selective digestive decontamination; survivors; syndrome; systemic.
T – Trauma is another inflammatory state that can trigger symptoms close to those of sepsis. It is interesting to underline similarities and differences in the management of patients with trauma and sepsis. First, in the bleeding trauma patient, a systematic investigation to identify the cause of bleeding has been implemented, using whole-body computed tomography scan (Caputo et al. 2014). This strategy should be assessed in patients with sepsis, to improve the identification of the sepsis source. Second, the mortality of trauma patients who develop septic shock is lower than that of non-trauma patients who develop sepsis. The causes of this difference may be age, comorbidities, underlying disease or immune dysfunction (Medam et al. 2017).
Others: terlipressin, tumour necrosis factors.
U – Ultrasound is essential to manage patients with sepsis and septic shock. This facilitates the source identification (lungs, kidneys, abdomen), assesses the effect of infection on several organs (lung oedema), provides a close look at the cardiac function and makes it possible to perform therapeutic interventions like an abscess drainage. The benefit is to use it at the bedside or in the conventional ward patient presenting a respiratory or circulatory failure (Zieleskiewicz et al. 2021).
Others: urine output.
V – Vasopressors are the other key treatment in septic shock with antibiotics. They separate sepsis and septic shock in addition to lactate (Singer et al. 2016). They mainly include catecholamines, vasopressin, and angiotensin 2. Among catecholamines, norepinephrine should be the first choice, acting on alpha receptors (favouring vessel contraction) and, with lower effects, on beta receptors (favouring inotropism). Epinephrine tends to be abandoned as first line treatment. Vasopressin is probably the best choice as second line, but the level of evidence supporting this statement remains low. Angiotensin 2 has emerged as an efficient interventional drug, but additional evidence is needed to use it in the best indications (Meresse et al. 2020).
Others: vasopressin.
W – Withholdingand Withdrawal of life-sustained therapy is a critical issue in sepsis. Studies in the field should always report the rate of withholding and withdrawal of life-sustained therapy among the non-survivors. A multi-professional discussion and an evaluation of patient wishes are required in each case (Sprung et al. 2019). Resuscitation should not be an end in itself; quality of life after ICU discharge is an endpoint that should be constantly discussed with the patient or their relatives.
X – XXXX was a drug with anticoagulant and anti-inflammatory properties that created significant hope to improve the outcomes of patients with sepsis. A first randomised controlled trial including patients in septic shock showed a decrease in 28-day mortality rate of around 6% in absolute value (Bernard et al. 2001). Unfortunately, the following randomised controlled trials did not confirm this result, notably in patients with sepsis, which resulted in the withdrawal of the drug by the company.
Y – Yeasts are an agent of infection that can cause sepsis. Among yeasts, Candida sp. and Aspergillus sp. are the most frequently reported in ICU patients (Vincent et al. 2020). Intensivists should keep in mind the possibility of infection by yeasts, especially in frail patients including those receiving immunosuppressive drugs and those treated with antibiotics for a long duration (Bassetti et al. 2017). Early identification and specific treatments based on guidelines are critical to improve patient outcomes. Simplification is often needed for choosing the best antifungal treatment (Chatelon et al. 2019).
Z – ZeroEnd-Expiratory Pressure is never indicated in the mechanically ventilated patient with septic shock. However, the best positive end-expiratory pressure (PEEP) should be set at the bedside as a personalised intervention, balancing the positive effects on ventilation and the negative effects on haemodynamics. The first goal with the ventilator setting is not to harm the patient. To this purpose, the strategy of high PEEP versus low PEEP does not really make sense for the clinicians.
Conflict of interest
Marc Leone received fees for symposium by Amomed and Aspen and for consulting by Ambu, Gilead and LFB.
References:
Al-Dorzi HM, Alsadhan AA, Almozaini AS et al. (2021) The performance of equations that estimate glomerular filtration rate against measured urinary creatinine clearance in critically ill patients. Crit Care Res Pract. 5520653.
Bassetti M, Garnacho-Montero J, Calandra T et al. (2017) Intensive care medicine research agenda on invasive fungal infection in critically ill patients. Intensive Care Med. 43(9):1225-1238.
Bernard GR, Vincent JL, Laterre PF et al. (2001) Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med. 344(10):699-709.
Caputo ND, Stahmer C, Lim G, Shah K (2014) Whole-body computed tomographic scanning leads to better survival as opposed to selective scanning in trauma patients: a systematic review and meta-analysis. J Trauma Acute Care Surg. 77(4):534-9.
Chatelon J, Cortegiani A, Hammad E et al. (2019) Choosing the right antifungal agent in icu patients. Adv Ther. 36(12):3308-3320.
Davidson JE, Aslakson RA, Long AC et al. (2017) Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med. 45(1):103-128.
Evans L, Rhodes A, Alhazzani W et al. (2021) Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 47(11):1181-1247.
Joffre J, Hellman J, Ince C, Ait-Oufella H (2020) Endothelial Responses in Sepsis. Am J Respir Crit Care Med. 202(3):361-370.
Leone M, Bouadma L, Bouhemad B et al. (2018) Hospital-acquired pneumonia in ICU. Anaesth Crit Care Pain Med. 37(1):83-98.
Levy B, Gibot S, Franck P et al. (2005). Relation between muscle Na+K+ ATPase activity and raised lactate concentrations in septic shock: a prospective study. Lancet. 365(9462):871-5.
López A, Lorente JA, Steingrub J et al. (2004) Multiple-center, randomized, placebo-controlled, double-blind study of the nitric oxide synthase inhibitor 546C88: effect on survival in patients with septic shock. Crit Care Med. 32(1):21-30.
Martin-Loeches I, Timsit JF, Leone M et al. (2019) Clinical controversies in abdominal sepsis. Insights for critical care settings. J Crit Care. 53:53-58.
Medam S, Zieleskiewicz L, Duclos G et al. (2017) Risk factors for death in septic shock: A retrospective cohort study comparing trauma and non-trauma patients. Medicine (Baltimore). 96(50):e9241.
Meresse Z, Medam S, Mathieu C et al. (2020) Vasopressors to treat refractory septic shock. Minerva Anestesiol. 86(5):537-545.
Monnet X, Teboul JL (2017) Transpulmonary thermodilution: advantages and limits. Crit Care. 21(1):147.
Nauclér P, Huttner A, van Werkhoven CH et al. (2021) Impact of time to antibiotic therapy on clinical outcome in patients with bacterial infections in the emergency department: implications for antimicrobial stewardship. Clin Microbiol Infect. 27(2):175-181.
Pickkers P, Darmon M, Hoste E et al. (2021) Acute kidney injury in the critically ill: an updated review on pathophysiology and management. Intensive Care Med. 47(8):835-850.
Rüddel H, Thomas-Rüddel DO, Reinhart K et al. (2022) Adverse effects of delayed antimicrobial treatment and surgical source control in adults with sepsis: results of a planned secondary analysis of a cluster-randomized controlled trial. Crit Care. 28;26(1):51.
Seymour CW, Liu VX, Iwashyna TJ et al. (2016) Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 315(8):762-74.
Singer M, Deutschman CS, Seymour CW et al. (2016) The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 315(8):801-10.
Sprung CL, Ricou B, Hartog CS et al. (2019) Changes in end-of-life practices in European intensive care units from 1999 to 2016. JAMA. 322(17):1692-1704.
Téblick A, Peeters B, Langouche L, Van den Berghe G (2019) Adrenal function and dysfunction in critically ill patients. Nat Rev Endocrinol. 15(7):417-427.
Textoris J, Fouché L, Wiramus S et al. (2011) High central venous oxygen saturation in the latter stages of septic shock is associated with increased mortality. Crit Care. 15(4):R176.
Vincent JL, Sakr Y, Singer M et al. (2020) Prevalence and outcomes of infection among patients in intensive care units in 2017. JAMA. 323(15):1478-1487.
Walter EJ, Hanna-Jumma S, Carraretto M, Forni L (2016) The pathophysiological basis and consequences of fever. Crit Care. 20(1):200.
Zieleskiewicz L, Lopez A, Hraiech S et al. (2021) Bedside POCUS during ward emergencies is associated with improved diagnosis and outcome: an observational, prospective, controlled study. Crit Care. 25(1):34.







