Approximately 20 million individuals globally undergo mechanical ventilation each year, and this number is expected to increase. While lifesaving, invasive ventilation can lead to complications, with 40% of ventilated time spent on liberating patients from the ventilator. Reducing the duration of mechanical ventilation is a key research priority for better outcomes. Research supports using weaning protocols and spontaneous breathing trials (SBTs) to assess a patient's ability to breathe independently.
A meta-analysis of trials showed that protocolised weaning significantly reduces weaning time, ventilation duration, and ICU stays. However, no studies have compared the frequency of patient screening for SBTs. Common SBT techniques include pressure-supported SBT with positive end-expiratory pressure (PEEP) and T-piece SBT.
A multicentre randomised trial compared screening frequencies and SBT techniques in critically ill adults to determine their effects on time to successful extubation. The study compared the effects of two factors on the time to successful extubation in critically ill patients: (1) screening frequency, comparing once-daily screening vs more frequent screening, and (2) SBT technique, comparing pressure-supported SBT (with pressure support of >0-≤8 cm H2O and PEEP of >0-≤5 cm H2O) vs T-piece SBT.
The trial included critically ill adults on invasive mechanical ventilation for at least 24 hours. Eligible patients could initiate spontaneous breaths or trigger the ventilator and were receiving a fractional inspired oxygen concentration of 70% or less with a PEEP level of 12 cm H2O or less. The study was conducted across 23 intensive care units in North America.
Participants were enrolled early to facilitate protocolised screening, comparing more frequent vs once-daily screening, to determine the earliest time they met the criteria for a pressure-supported or T-piece SBT, which lasted between 30 to 120 minutes. "Time to successful extubation" refers to the duration from the start of the trial until the patient began unsupported, spontaneous breathing and maintained it for at least 48 hours after being extubated.
The trial included 797 patients divided into four groups based on screening frequency (once-daily or more frequent) and SBT technique (pressure-supported or T-piece). The average age was 62.4 years, and 59.2% were men. There were no statistically significant differences in time to successful extubation based on screening frequency or SBT technique. The median time to successful extubation ranged from 2.0 to 3.9 days across the groups. An unexpected interaction showed that more frequent screening with pressure-supported SBT increased the time to extubation. However, once-daily screening with pressure-supported SBT did not significantly reduce extubation time compared to T-piece SBT.
These findings show that in critically ill adults on invasive mechanical ventilation for over 24 hours, neither the screening frequency (once-daily vs more frequent) nor the SBT technique (pressure-supported vs T-piece) significantly impacted the time to successful extubation. However, an unexpected statistically significant interaction was found: more frequent screening combined with pressure-supported SBTs increased the time to the first successful extubation.
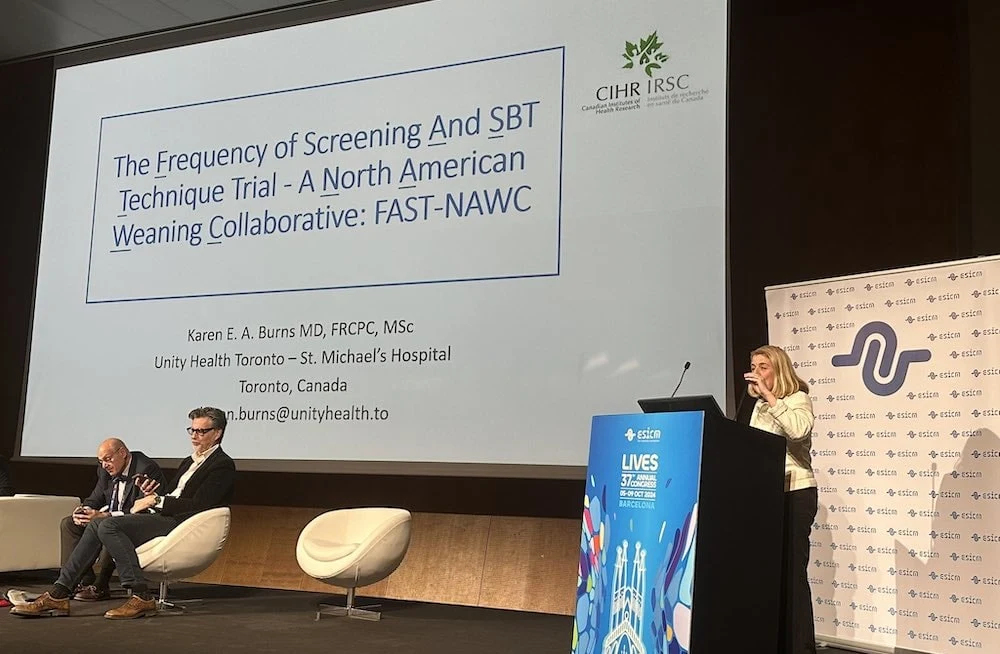
Source: JAMA, #LIVES2024
Image Credit: #LIVES2024