ICU Management & Practice, Volume 24 - Issue 4, 2024
Early mobilisation within 72 hours of ICU admission mitigates risks including reduced functionality and cognitive decline in critically ill patients, improving outcomes such as mobility and quality of life. Overcoming barriers through flexible staffing, protocols, and personalised care strategies is essential to humanising critical care in daily practice. We apply this evidence-based approach to Mr Smith.
Critically ill patients treated in intensive care units (ICU) have an increased risk of developing several sequelae, including reduced functionality and muscle strength, ICU-acquired weakness (ICU-AW), cognitive decline, delirium, and others (Fazzini et al. 2023; Renner et al. 2023). Most of these risks can be mitigated by early physical activity and mobilisation, which is defined as mobilisation starting within 72 hours of ICU admission ICU (Schaller et al. 2024). Early mobilisation has shown to positively influence mobility, functional independence, incidence and days in delirium, days on mechanical ventilation, ICU and hospital length of stay, discharge home, long-term cognitive function, and quality of life (Okada et al. 2019; Wang et al. 2020; Zang et al. 2020). Similarly, complications such as ventilator-associated pneumonia, pressure sores, or deep venous thromboses can be reduced (Daum et al. 2024; Jiroutková et al. 2024; Wang et al. 2020).
Forms of Mobilisation
Early mobilisation includes measures on patients that initiate or support passive or active movement exercises and aim to promote or maintain the ability to move. This includes passive range of motion exercises or cycling, active exercises in bed (active range of motion, sitting up in bed), and out-of-bed activities (sitting on the edge of bed, standing, active/passive transfer to chair, walking). Particularly early on during critical illness, neuromuscular electrical stimulation, assist devices, and robotics can be a useful supplement to facilitate mobilisation therapy (Clarissa et al. 2019; Grunow et al. 2022; Lorenz et al. 2024). Considering inclusion and exclusion criteria and appropriate clinical assessment, these activities are feasible and safe, even with patients on mechanical ventilation, vasopressor therapy, and extracorporeal membrane oxygenation (Schaller et al. 2024).
Protocols
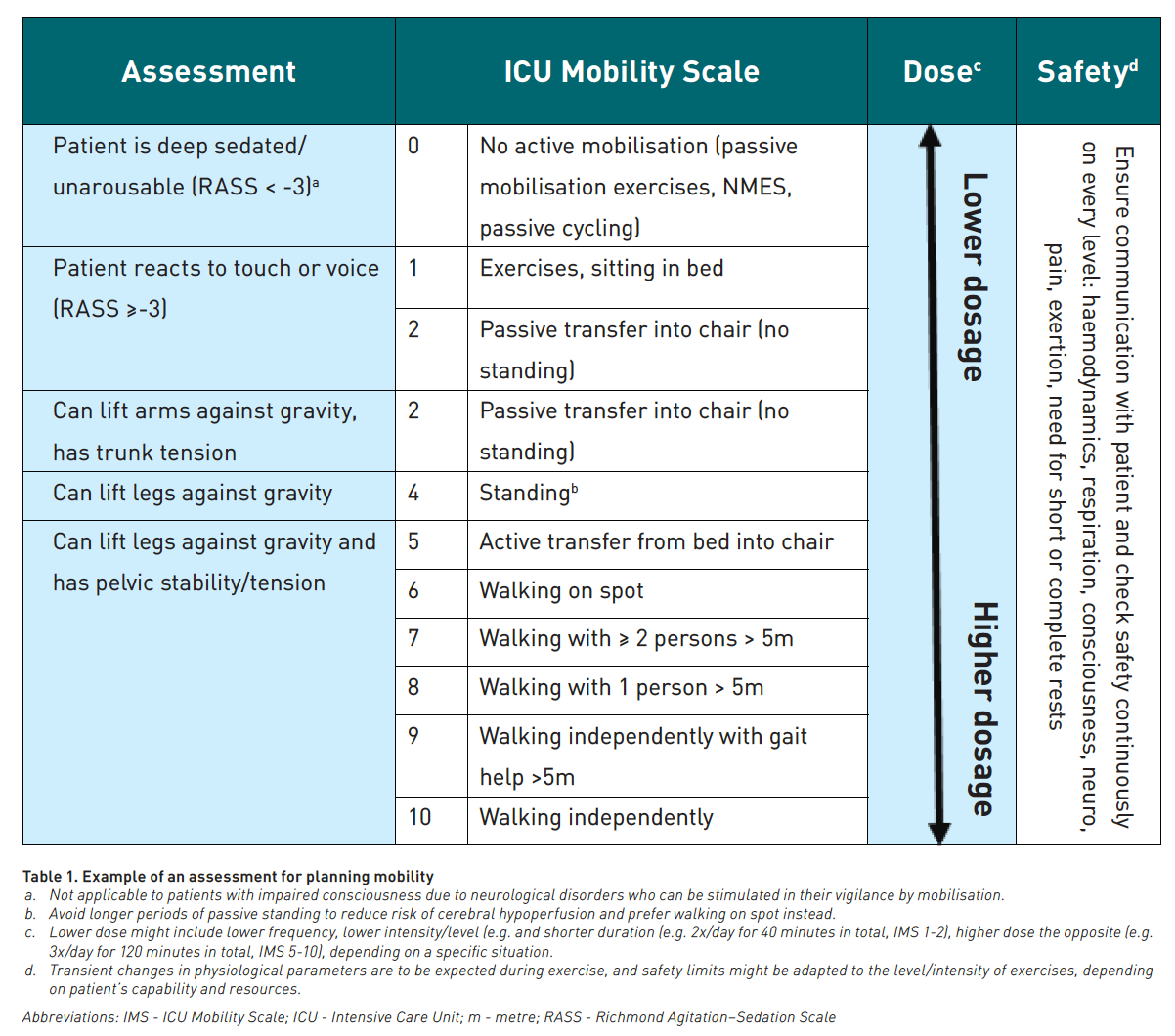
In daily clinical practice, early mobilisation is delivered in an interprofessional team approach and can be guided by protocols such as the ABCDEF bundle, which includes interventions for analgesia and sedation, delirium, spontaneous breathing trials, mobilisation and family integration by the whole interprofessional critical care team (Marra et al. 2017; Pun et al. 2019). For implementing early mobilisation into daily practice, the use of interprofessional protocols is recommended as they facilitate conducting early mobilisation in the ICU (Schaller et al. 2024). Protocols should include a) initiation criteria for mobilisation of patients in- and outside the bed, e.g. by a traffic light system; b) assessment of consciousness and function; c) scales such as the ICU mobility scale for planning, performing, and documenting mobility; d) safety criteria for discontinuing a mobilisation session; e) checklists for devices (Eggmann et al. 2024; Parry et al. 2018; Schaller et al. 2016) (Table 1). As such, mobilisation should be an integral component of daily ICU rounds together with sedation, ventilation, haemodynamics, nutrition etc.
Question of the Right Dose
While it is recognised that mobilisation and physical activity improve patient outcomes, there is growing evidence that different variables should be considered when correctly quantifying and applying mobilisation. This includes not only the intensity (most often level) but also the frequency and duration of mobilisation. Accordingly, mobilisation protocols have used a daily frequency of mobilisation (Morris et al. 2016; Schaller et al. 2016) with a proposed number of daily mobilisation sessions. Other mobilisation protocols recommend a duration of physical activity of up to 60-90 minutes per day (Hodgson et al. 2016; Wright et al. 2018). Furthermore, scores to combine the level and duration of activity have been developed (Scheffenbichler et al. 2021; Watanabe et al. 2021). This synergy of characteristics of physical activity positively influences patient-centred outcomes. Yet the optimal dose of mobilisation needs to be adapted to each individual patient based on individual clinical assessment and comorbidities. Receiving the maximum possible activity intensity increased 180-day mortality risk in patients with diabetes mellitus in a secondary analysis of the TEAM trial (Investigators et al. 2022; Serpa Neto et al. 2024). Similarly, very early and longer mobilisation sessions increased mortality in stroke patients treated in stroke units (Bernhardt et al. 2016; Bernhardt et al. 2015). In general, the dose of mobilisation in its level/intensity, frequency, and duration should be adapted to patients' individual capability and tolerance, with higher dose in patients with higher physiological reserves.
Barriers and Implementation
Patient-specific barriers (haemodynamic instability, endotracheal tubes and other lines, delirium and agitation, etc.), structural barriers (time constraints, staff shortage, lack of protocols or equipment, and others) and missing education, knowledge, and culture often prevent early mobilisation from being performed at all or according to the standards proposed in validated mobilisation protocols (Dubb et al. 2016). These barriers can be overcome by several strategies in an interprofessional implementation process, including baseline assessment of mobilisation, identification of local barriers, use of appropriate strategies, implementation, re-assessment of the mobility rates, reflection, and feedback to the team (Barr et al. 2021). The hospital and ICU management should provide the resources to address barriers and implement early mobilisation in the ICU (Schaller et al. 2024).
With regard to the implementation of scientific findings on early mobilisation with better results for patients and cost savings for hospitals, the management levels should also support these practical topics with their own ideas at an early stage (Azuh et al. 2016; Lord et al. 2013; Unoki et al. 2024). The planning of additional mobility teams to ensure early mobilisation is certainly helpful, but in times of staff shortages, it is quite a challenge. Here, flexible working time models and financial incentives could ensure that employees who work part-time, among others, would be willing to increase their working hours for special activities to be additionally available for early mobilisation. In addition to human resources, technical support through mobility aids or robotics may also become increasingly important, but empirical data on the use of robotics to support specialist staff in intensive care units are limited (Lorenz et al. 2024; Mehler-Klamt et al. 2023; Warmbein et al. 2024). Before investments in robotics are made, the minimum requirement for robotics is to demonstrate (1) a benefit for the patients and (2) an actual reduction in the workload of healthcare staff. The authors also argue that such investments must be carefully weighed against additional investment in the recruitment and retention of healthcare professionals until it is also demonstrated that robotic mobilisation adds value to conventional mobilisation.
When Evidence Comes to Mr Smith
Especially in critically ill patients, who often suffer from impaired consciousness, pain, or fatigue, it is essential to adapt the standardised mobilisation to an individual goal setting (Nydahl et al. 2024a). Therapy goals should follow the SMART rule, making them Specific, Measurable, Achievable, Reasonable and Time-bound. A differentiation between long and short-term goals is sensible. To improve patient adherence and clinical outcomes, a shared decision-making (SDM) approach should be used to set goals, which might also prevent wrong expectations (More and Kaplan 2018).
Let us assume that Mr Smith is a patient in our ICU, suffering from sepsis, ICU-AW, delirium, and is still on mechanical ventilation (MV). He is physically weak and mentally fatigued, wondering how fast this all could happen. We approach him with a motivating dialogue and involve his family to get to know his personal interests and short- and long-term goals so that we can motivate him for rehabilitation. His family personalises the room with photos of him with his family, in the garden, with grandchildren, or with his dog. Patient Smith becomes Mr Smith. The family writes notes on his "get-to-know-me" board with personal information, helping us to tailor activities to his interests and daily habits. Meeting the family is important for him, and being outside, so we mobilise him into a wheelchair and arrange a tour for him to the hospital’s garden where he can meet his family and dog, even with mechanical ventilation and a few standing exercises in the garden. He comes back with bright eyes and smiles, and the whole team is proud of him and his excellent care. The nurse reports in his ICU diary: “Today, you reached a milestone!” and adds a photo of him being in the sunshine with his family. Only in an ideal world? No, in a lot of ICUs, early mobilisation became routine; studies have shown an overall mobilisation rate ranging from 10% to 73%, the rate for patients with MV being lower with a range of 7% to 33% (Nydahl et al. 2024b). So even though barriers still exist, and the mobilisation rate could still be increased, this could be a real-world case.
Conclusion
In conclusion, early rehabilitation improves patient outcomes when it is appropriately dosed. This individualised approach to early rehabilitation has not yet been sufficiently studied, since early rehabilitation in critical care is a complex intervention comprising multiple interconnected components. As in other areas of medicine, we need to consider the individuality of patients, including their capabilities, needs, experiences, values, and personal contexts, thereby humanising critical care (Heras La Calle et al. 2017). Humanising critical care involves a multi-professional, multi-disciplinary approach that includes elements such as effective communication, patient well-being, flexible visiting hours, the involvement and participation of relatives, the prevention and treatment of Post-Intensive Care Syndrome, humanised architecture and infrastructure, and appropriate end-of-life care (Nin Vaeza et al. 2020). This will be the future of critical care.
Conflict of Interest
None.
References:
Azuh O, Gammon H, Burmeister C et al. (2016) Benefits of early active mobility in the medical intensive care unit: A pilot study. Am J Med. 129(8):866-871.e1.
Barr J, Paulson SS, Kamdar B et al. (2021) The coming of age of implementation science and research in critical care medicine. Crit Care Med. 49(8):1254-1275.
Bernhardt J, Churilov L, Ellery F et al. (2016) Prespecified dose-response analysis for A Very Early Rehabilitation Trial (AVERT). Neurology. 86(23):2138-2145.
Bernhardt J, Churilov L, Ellery F et al. (2015) Efficacy and safety of very early mobilisation within 24 h of stroke onset (AVERT): a randomised controlled trial. Lancet. 386(9988):46-55.
Clarissa C, Salisbury L, Rodgers S, Kean S (2019) Early mobilisation in mechanically ventilated patients: a systematic integrative review of definitions and activities. J Intensive Care. 7:3.
Daum N, Drewniok N, Bald A et al. (2024) Early mobilisation within 72 hours after admission of critically ill patients in the intensive care unit: A systematic review with network meta-analysis. Intensive Crit Care Nurs. 80:103573.
Dubb R, Nydahl P, Hermes C et al. (2016) Barriers and strategies for early mobilization of patients in intensive care units. Ann Am Thorac Soc. 13(5):724-730.
Eggmann S, Nydahl P, Gosselink R, Bissett B (2024) We need to talk about adverse events during physical rehabilitation in critical care trials. eClinicalMedicine. 68:102439.
Fazzini B, Märkl T, Costas C et al. (2023) The rate and assessment of muscle wasting during critical illness: a systematic review and meta-analysis. Crit Care. 27(1):2.
Grunow JJ, Nydahl P, Schaller SJ (2022) Mobilisation of intensive care unit patients: How can the ICU rooms and modern medical equipment help? Anasthesiol Intensivmed Notfallmed Schmerzther. 57(1):41-51.
Heras La Calle G, Oviés Á, Tello VG (2017) A plan for improving the humanisation of intensive care units. Intensive Care Med. 43(4):547-549.
Hodgson CL, Bailey M, Bellomo R et al. (2016) A binational multicenter pilot feasibility randomized controlled trial of early goal-directed mobilization in the ICU. Crit Care Med. 44(6):1145-1152.
Investigators TS, Hodgson CL, Bailey M et al. (2022) Early active mobilization during mechanical ventilation in the ICU. N Engl J Med. 387(19):1747-1758.
Jiroutková K, Duška F, Waldauf P (2024) Should new data on rehabilitation interventions in critically ill patients change clinical practice? Updated meta-analysis of randomized controlled trials. Crit Care Med.
Lord RK, Mayhew CR, Korupolu R et al. (2013) ICU early physical rehabilitation programs: financial modeling of cost savings. Crit Care Med. 41(3):717-724.
Lorenz M, Baum F, Kloss P et al. (2024) Robotic-Assisted In-Bed Mobilization in Ventilated ICU Patients With COVID-19: An Interventional, Randomized, Controlled Pilot Study (ROBEM II Study). Crit Care Med. 52(5):683-693.
Marra A, Ely EW, Pandharipande PP, Patel MB (2017) The ABCDEF bundle in critical care. Crit Care Clin. 33(2):225-243.
Mehler-Klamt AC, Huber J, Schmidbauer L et al. (2023) The use of robotic and technical systems for early mobilization of intensive care patients: A scoping review. Pflege. 36(3):156-167.
Morris PE, Berry MJ, Files DC et al. (2016) Standardized rehabilitation and hospital length of stay among patients with acute respiratory failure: A randomized clinical trial. JAMA. 315(24):2694-2702.
Nin Vaeza N, Martin Delgado MC, Heras La Calle G (2020) Humanizing intensive care: Toward a human-centered care ICU model. Crit Care Med. 48(3):385-390.
Nydahl P, Heras-La Calle G, McWilliams D (2024a) Personalized rehabilitation: A step towards humanizing critical care. Intensive Crit Care Nurs. 82:103634.
Nydahl P, Fick LS, Eggmann S (2024b) Break down barriers - Can point prevalence studies change mobilization practice in the intensive care unit? Intensive Crit Care Nurs. 80:103537.
Okada Y, Unoki T, Matsuishi Y et al. (2019) Early versus delayed mobilization for in-hospital mortality and health-related quality of life among critically ill patients: a systematic review and meta-analysis. J Intensive Care. 7:57.
Parry SM, Nydahl P, Needham DM (2018) Implementing early physical rehabilitation and mobilisation in the ICU: institutional, clinician, and patient considerations. Intensive Care Med. 44(4):470-473.
Pun BT, Balas MC, Barnes-Daly MA et al. (2019) Caring for critically ill patients with the ABCDEF bundle: Results of the ICU Liberation Collaborative in over 15,000 adults. Crit Care Med. 47(1):3-14.
Renner C, Jeitziner MM, Albert M et al. (2023) Guideline on multimodal rehabilitation for patients with post-intensive care syndrome. Crit Care. 27(1):301.
Schaller SJ, Anstey M, Blobner M et al. (2016) Early, goal-directed mobilisation in the surgical intensive care unit: a randomised controlled trial. Lancet. 388(10052):1377-1388.
Schaller SJ, Scheffenbichler F, Bein T et al. (2024) Guideline on positioning and early mobilisation in the critically ill by an expert panel. Intensive Care Med. 50(8):1211-1227.
Scheffenbichler FT, Teja B, Wongtangman K et al. (2021) Effects of the level and duration of mobilization therapy in the ICU on neuromuscular function and outcomes: A systematic review and meta-analysis. Crit Care Med. 49(9):1561-1573.
Serpa Neto A, Bailey M, Seller D et al. (2024) Impact of high dose early mobilization on outcomes for patients with diabetes: A secondary analysis of the TEAM trial. Am J Respir Crit Care Med.
Unoki Y, Ono S, Sasabuchi Y et al. (2024) Exploring the influence of a financial incentive scheme on early mobilization and rehabilitation in ICU patients: an interrupted time-series analysis. BMC Health Serv Res. 24(1):242.
Wang J, Ren D, Liu Y et al. (2020) Effects of early mobilization on the prognosis of critically ill patients: A systematic review and meta-analysis. Int J Nurs Stud. 110:103708.
Warmbein A, Hübner L, Rathgeber I et al. (2024) Robot-assisted early mobilization for intensive care unit patients: Feasibility and first-time clinical use. Int J Nurs Stud. 152, 104702.
Watanabe S, Morita Y, Suzuki S et al. (2021) Effects of the intensity and activity time of early rehabilitation on activities of daily living dependence in mechanically ventilated patients. Prog Rehabil Med. 6:20210054.
Wright SE, Thomas K, Watson G et al. (2018) Intensive versus standard physical rehabilitation therapy in the critically ill (EPICC): a multicentre, parallel group, randomised controlled trial. Thorax. 73(3):213-221.
Zang K, Chen B, Wang M et al. (2020) The effect of early mobilization in critically ill patients: A meta-analysis. Nurs Crit Care. 25(6):360-367.











