End-of-life (EoL) care focuses on symptom relief and addressing the emotional, psychological, and spiritual needs of patients and their families. These decisions are influenced by ethical, legal, cultural, and resource-related factors, and practices vary globally. In some countries, life-supporting treatment (LST) decisions are shared with families, while in others, clinicians decide alone.
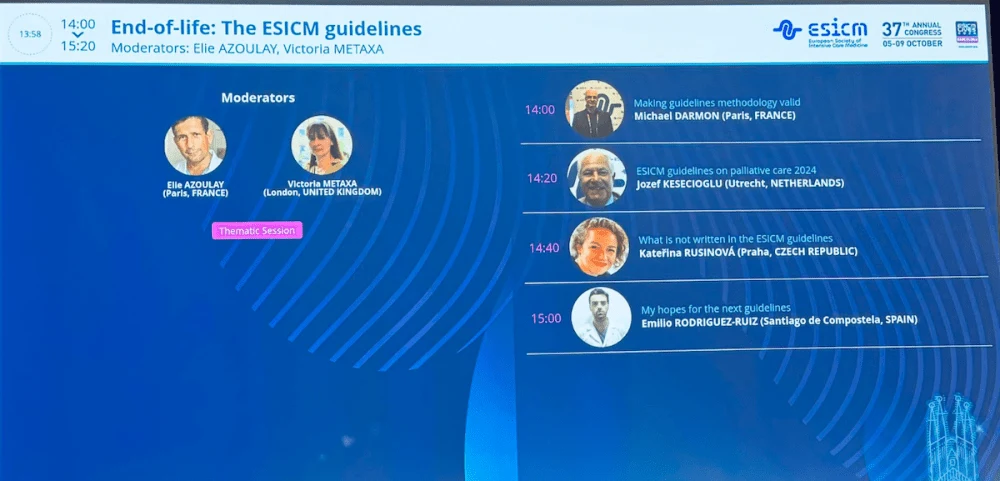
The guidelines for end-of-life (EoL) care in the ICU were created by an international expert panel on behalf of the European Society for Intensive Care Medicine (ESICM). The panel divided the guidelines into seven pre-defined domains, each overseen by a domain chair, with a methodologist ensuring the transparency and reproducibility of the process. These guidelines offer eight evidence-based recommendations—six with a low level of evidence and two with a high level of evidence—along with 19 expert opinions.
Having national regulations on EoL care, which permit the withholding or withdrawing of LSTs, can enhance EoL care, improve patient and family satisfaction, and promote patient autonomy. Countries lacking such regulations are encouraged to create legal frameworks to facilitate LST limitations, with support from intensive care clinicians, professional societies, lawmakers, and other leaders.
While these recommendations are based on expert opinion, there is insufficient evidence to warrant formal recommendations. Experts also suggest that these regulations should include provisions for patients' preferences, such as advance directives, living wills, and powers of attorney, in the EoL decision-making process, although, again, there is not enough evidence for a formal recommendation.
Approaches to EoL care for critically ill patients vary between low- and middle-income countries (LMICs) or resource-constrained environments and high-income countries (HICs) across different domains. However, there is insufficient evidence to support a formal recommendation regarding these differences.
Family members must have a clear understanding of the patient's condition to effectively clarify the goals of care. Additionally, the guidelines suggest assessing how patients and their families cope with the ICU environment to identify specific needs for optimal communication and personalised discussions about care goals. However, there is insufficient evidence to support formal recommendations for these practices.
For adult critically ill patients where LST is considered non-beneficial, implementing structured EoL decision-making strategies may help surrogates understand the care provided, clarify their preferred roles in the decision-making process, and define patient-centred goals of care. Additionally, structured support and communication can be offered to family members after the decision to forgo ICU treatment for adult critically ill patients, as this may help reduce complicated grief, anxiety, and PTSD symptoms. However, this recommendation is based on a low level of evidence.
The guidelines also recommend employing a structured EoL decision-making strategy for critically ill patients when LST is considered inappropriate. This approach may enhance staff satisfaction and reduce mental health symptoms among healthcare professionals. However, there is insufficient evidence to support formal recommendations for this strategy.
Early palliative care, including consultations with palliative care specialists for ICU patients at high risk of morbidity and mortality, could improve quality of life and better align care with patient goals. However, there is insufficient evidence to support formal recommendations for this practice.
Experts suggest that validated instruments for assessing symptoms should be utilised in ICU patients with advanced illness to enhance symptom detection and treatment. This recommendation is based on a low level of evidence.
Relatives of dying ICU patients may benefit from structured support, including family conferences held before and after the patient's death. However, there is insufficient evidence to support formal recommendations for this practice.
Regularly re-evaluating the proportionality of LSTs in the ICU, involving patients, family members, and multidisciplinary teams, may help reduce unnecessary procedures and decrease the length of stay in the ICU and hospital. However, there is insufficient evidence to support formal recommendations for this practice.
Experts suggest that structured training programmes should be implemented for ICU healthcare professionals to improve their competencies in EoL communication. This recommendation is based on a low level of evidence. They also recommend implementing enhanced written communication tools, such as brochures, pamphlets, or leaflets, for the families of ICU patients to complement standard oral communication. This recommendation is supported by a high level of evidence.
Experts suggest that communication with the families of critically ill patients dying in the ICU should be managed by an intensivist team with palliative care training. This recommendation is based on a low level of evidence.
Palliative care interventions may be beneficial for patients with poor prognosis, even when receiving optimal intensive care, as they could enhance satisfaction with care for both patients and family members. However, there is insufficient evidence to support a formal recommendation for this practice.
Experts recommend implementing flexible visiting policies to help reduce family anxiety and enhance satisfaction. However, there is insufficient evidence to support formal recommendations for this practice. They also recommend providing bereavement brochures or leaflets along with structured family conferences before a patient's death to support families at the end of life, supported by a high level of evidence. Additionally, they suggest that condolence letters written by the ICU team should not be routinely sent to bereaved family members, although this recommendation is based on a low level of evidence.
Encouraging family-led care in EoL situations may be acceptable to family members and could lead to better outcomes for caregivers. However, there is insufficient evidence to support a formal recommendation for this practice.
EoL care should be customised to accommodate the cultural needs of patients and their families whenever possible. However, there is insufficient evidence to support a formal recommendation for this practice. Implementing a protocol to prevent and address conflict situations among healthcare professionals or with family members. However, there is insufficient evidence to support a formal recommendation for this practice.
Promoting multidisciplinary communication in EoL situations by discussing care goals among all parties involved—patients, family members, and professionals. The guidelines also suggest implementing strategies to prevent mental distress, including ethical discussions in the ICU. However, there is insufficient evidence to support a formal recommendation for these practices.
These guidelines are designed to assist ICU healthcare professionals in addressing the significant challenges associated with EoL care. The lack of data and the considerable variability in practices and outcomes across ICUs and countries highlight the need for more legislative and research efforts.
The guidelines establish a research agenda that summarises literature from recent decades and provides evidence-based recommendations and expert opinions on EoL and palliative care for critically ill adults, benefiting patients, families, and healthcare professionals. However, the guidelines are limited by the absence of high-quality studies, particularly RCTs, which restricts the ability to make strong evidence-based recommendations.
Effective communication within the ICU team and with patients and their families is crucial. While structured programmes aimed at improving EoL communication for ICU healthcare professionals have shown promise, their long-term effects need further evaluation, particularly regarding documentation of patient preferences, quality of dying, ICU length of stay, mental health symptoms in relatives, and the well-being of healthcare professionals. Challenges related to cultural, religious, and racial diversity in communication require special attention. Additionally, research is needed to understand how legislation regarding EoL practices and patient and family rights may impact communication and well-being.
The use of treatment limitation tools (TLTs) and other strategies to reach a consensus between the ICU team, patients, and families can help protect healthcare professionals from moral distress and prevent unnecessary suffering for patients. Evaluating visiting policies, collecting memory-making materials before death, and providing follow-up bereavement support are potential ways to improve outcomes for relatives that warrant high-quality studies. Furthermore, personal-care programmes for ICU healthcare professionals and monitoring staff well-being by ICU leaders should also be explored.
Source: LIVES2024; Intensive Care Medicine
Image Credit: #LIVES2024