HealthManagement, Volume 19 - Issue 4, 2019
Summary: Differences in sex and gender may account for gaps in treatment and prevention of cardiovascular disease, but at the same time, it also gives the opportunity for personalised sex and gender-specific medicine.
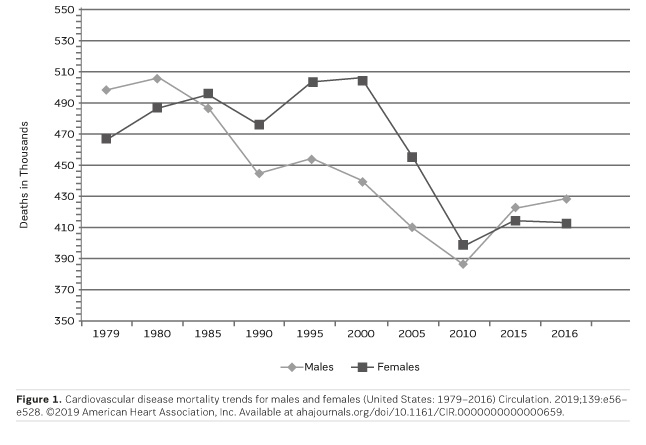
Typical presentations in medicine are defined in ways that health care professionals can draw on past experiences and education to adequately diagnose, treat, and heal. Yet, when it comes to cardiovascular disease (CVD), a “typical presentation” may not be accurate for half of the population. CVD is the leading cause of death in the United States of both men and women according to the Center for Disease Control (CDC), yet the typical risks factors and presentation for the disease differ in clinically important ways. The impact of sex and gender in health and disease is especially illustrated with CVD as the “typical” criteria for presentation chest pain, diaphoresis, nausea, radiating pain to the left shoulder and jaw, were developed from research on men.
You might also like: Personalised medicine and cardiovascular disease
Sex and Gender Impacts on Quality of Care
When CVD risks are not recognised, women are also less likely to be given aggressive treatment for the prevention of CVD such as lipid-lowering therapy, aspirin, and therapeutic lifestyle changes even when they present with the same risk for atherosclerotic CVD (Abuful et al. 2005). Abuful also noted that physicians suspected chest pain as having an actual cardiac origin more often in men than in women. Physician gender bias in prevention and treatment strategies can lead to serious consequences. While differences in sex and gender may account for gaps in treatment and prevention of cardiovascular disease, it also gives the opportunity for personalised sex and gender-specific medicine.
Risk Factors for Cardiovascular Disease: Traditional and Non-Traditional
Non-traditional risk factors for CVD are associated with the ability of women to bear children, associated with higher oestrogen levels in women, and associated with social and economic stressors. These include gestational hypertensive disorders, preeclampsia, gestational diabetes, autoimmune disorders, depression, and declining oestrogen levels (Saeed et al. 2017). Having increased blood pressure in pregnancy not only contributes to a greater risk for mortality in both the mother and baby, but also puts the mother at risk later on in life for developing high blood pressure and cardiovascular related disease (Ferranti et al. 2016). As women reach menopause, their oestrogen levels decline. Oestrogen protects and enhances the survival of cardiomyocytes within a woman’s heart when placed under stress (Kim et al. 2006). These risks support the notion that a typical presentation of CVD must be further defined to include the sex that it describes.
Risk for heart disease for both men and women:
- Smoking
- Diabetes
- High Cholesterol (high HDL and/or low HDL
- High Blood Pressure
- Obesity
- Sedentary Lifestyle
For women only
- Menopause
- Birth Control Pills in conjunction with smoking
Ischaemia in the setting of no obstructive coronary artery disease (INOCA) is associated with coronary microvascular dysfunction and adverse cardiac outcomes. More common in women, INOCA may explain the difference in heart attack symptoms and complicates the diagnosis and treatment of CVD. For example, if a cardiac catheterisation is the gold standard for diagnosis of CVD, but women have INOCA then some may be wrongly categorised as having no significant disease. Without using criteria that accounts for the impact of sex and gender, blood tests such as troponin may lead to patients wrongly “ruled out” from having CVD.
While both men and women may have chest pain when having a myocardial infarction, women are more likely to have ischaemia without “typical” chest pain symptoms and are more likely to face mortality without this traditional presentation (Canto et al. 2012). We need to reclassify “typical and atypical” presentations of CVD as this terminology contributes to bias that may lead to incorrect diagnoses. Instead, the development of guidelines and criteria that are sex and gender-specific will improve diagnosis and treatment options, and with increased recognition, we can decrease the mortality from CVD in women.
Stress and CVD Risk
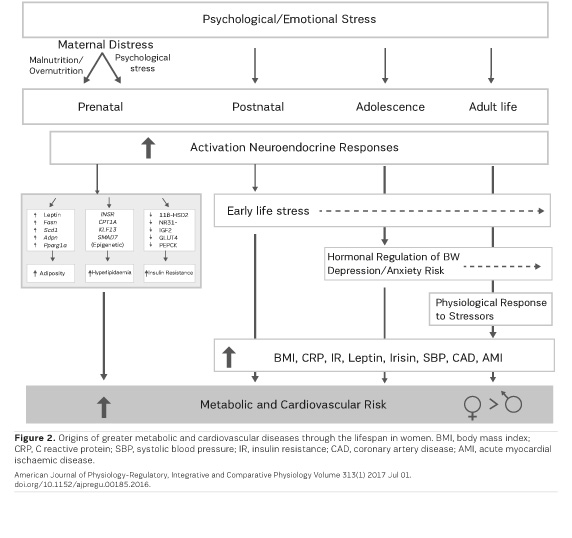
Mental and physical stress, whether experienced early or later in life, is increasingly recognised as significantly influencing the development of chronic diseases. Studies available show that the correlation between stress and CVD risk do not treat the sexes equally. Investigating the effect of socioeconomic status in puberty, a sub-study of the Ovarian Aging Study found that lower socioeconomic status for women in puberty correlated with lower levels of sex hormone-binding globulin (SHBG). SHBG is derived from an index of bioavailable testosterone, and is related to CVD associated hormone profiles (Bleil et al. 2015). Therefore, women that experienced lower socioeconomic status (SES), and the stressors that come with it, have a greater risk for CVD as they age from pubescence into adulthood. In a model by Miller, stress associated with lower SES early on in life heightens the response of macrophages and monocytes, creating a state of chronic inflammation. This inflammation, along with genetic susceptibility, can lead to chronic diseases such as chronic heart disease (Miller et al. 2011). In a study of the prevalence of Adverse Childhood Events (ACEs) over 23 states between 2011-2014, the mean score of ACEs was higher for women than in men, and was higher for multiracial communities than other races (Merrick et al. 2018). Women report experiencing adverse events in childhood more than men and these adverse events and stressors can lead to higher risks for CVD as they reach adulthood. These additional risk factors for women should heighten our awareness of the potential for CVD. Limited studies have purposefully looked into sex-related correlations on stress and cardiovascular risk, further qualifying the need for such research (Murphy & Loria 2017).
In a perspective from Murphy, there is substantial evidence pointing to several psychosocial disadvantages impacting young women, and this condition will most likely affect the metabolic and CVD risk in the next generation (Murphy & Loria 2017).
Conclusion
Key points
- When it comes to CVD, a typical presentation may not be accurate for half of the population
- In CVD, sex and gender differences contribute to a lower perceived risk of morbidity in women than in men
- A typical presentation of CVD must be further defined to include the sex that it describes
- We need to reclassify typical and atypical presentations of CVD as this terminology contributes to bias that may lead to incorrect diagnoses
References:
Abuful A, Gidron Y, Henkin Y (2005) Physicians' attitudes toward preventive therapy for coronary artery disease: is there a gender bias? Clin Cardiol, 28(8):389-393.
Bleil ME, Appelhans BM, Latham MD, Irving MA, Gregorich SE, Adler NE, Cedars MI (2015) Neighborhood socioeconomic status during childhood versus puberty in relation to endogenous sex hormone levels in adult women. Nurs Res, 64(3):211-220.
Canto JG, Rogers WJ, Goldberg RJ, Peterson ED, Wenger NK, Vaccarino V, Kiefe CI, Frederick PD, Sopko G, Zheng ZJ; NRMI Investigators (2012) Association of age and sex with myocardial infarction symptom presentation and in-hospital mortality. JAMA, 307(8):813-822.
Ferranti EP, Jones EJ, Hernandez TL (2016) Pregnancy Reveals Evolving Risk for Cardiometabolic Disease in Women. J Obstet Gynecol Neonatal Nurs, 45(3):413-425.
Garcia M, Mulvagh SL, Merz CN, Buring JE, Manson JE (2016) Cardiovascular Disease in Women: Clinical Perspectives. Circ Res, 118(8):1273-1293.
Kim JK, Pedram A, Razandi M, Levin ER (2006) Estrogen prevents cardiomyocyte apoptosis through inhibition of reactive oxygen species and differential regulation of p38 kinase isoforms. J Biol Chem, 281(10):6760-6767.
Merrick MT, Ford DC, Ports KA, Guinn AS (2018) Prevalence of Adverse Childhood Experiences From the 2011-2014 Behavioral Risk Factor Surveillance System in 23 States. JAMA Pediatr, 172(11):1038-1044.
Miller GE, Chen E, Parker KJ (2011) Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychol Bull, 137(6): 959-997.
Murphy MO, Loria AS (2017) Sex-specific effects of stress on metabolic and cardiovascular disease: are women at higher risk? Am J Physiol Regul Integr Comp Physiol, 313(1), R1-R9.
Saeed A, Kampangkaew J, Nambi V (2017) Prevention of Cardiovascular Disease in Women. Methodist Debakey Cardiovasc J, 13(4):185-192.


![Tuberculosis Diagnostics: The Promise of [18F]FDT PET Imaging Tuberculosis Diagnostics: The Promise of [18F]FDT PET Imaging](https://res.cloudinary.com/healthmanagement-org/image/upload/c_thumb,f_auto,fl_lossy,h_184,q_90,w_500/v1721132076/cw/00127782_cw_image_wi_88cc5f34b1423cec414436d2748b40ce.webp)





