HealthManagement, Volume 17 - Issue 1, 2017
Healthcare service providers face significant challenges in attracting patients and retaining qualified staff. The most obvious way to outshine one’s competitors is to offer superior clinical capabilities, but such innovations can seem prohibitively expensive. Read about seven strategies that hospital systems can employ to advance their clinical capabilities, respond to the evolving challenges of healthcare today, and attract both clinicians and patients.
Invest in New Diagnostic and Therapeutic Modalities to Improve Outcomes and Expand Services
The most obvious way for service providers to augment their clinical capabilities is to offer the very latest diagnostic and therapeutic technology. For instance, innovative imaging techniques can significantly improve the speed and reliability of diagnosis, and hence of treatment success as well. They can also reduce the length of hospital stays, and as a result, the overall cost of treatment.1 Novel clinical procedures and processes can also have a positive effect on medical staff – by reducing the workload, or promoting the flow of information and knowledge sharing along the treatment chain, for example. Ultimately, no service providers want to be the last ones in their region to offer diagnostic and therapeutic capabilities that are being touted by all of their competitors. Therefore, navigating this challenge requires an outcomes-based investment strategy for acquiring the new equipment necessary to remain competitive, along with a fleet management approach to ensure that each new investment continues to provide clinical value throughout its lifetime.
Implement Patient-Centered
Process Innovations
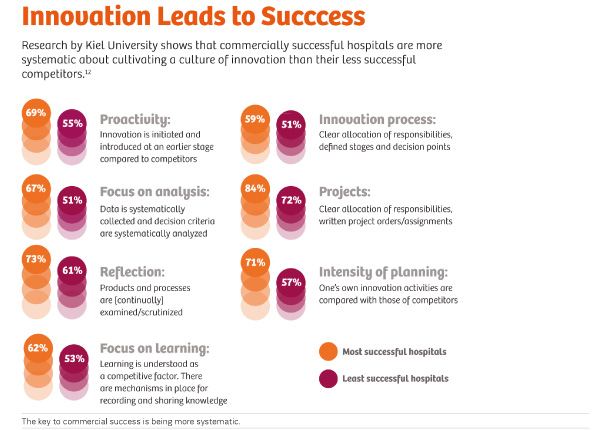
Companies that systematically focus on innovation in products, services, business models, and customer targeting grow more quickly, generate more revenue, and are more successful.2 The same goes for healthcare providers, for whom innovation has become a key success factor. So, just like companies in the business and academic sectors, hospitals benefit from participation in innovation networks as well. To be able to offer patients new treatment options, they need access to new medical procedures. A particular challenge for companies across all industries is how to create appropriate structures for innovation and develop an effective innovation culture. Healthcare providers with a strong culture of innovation that runs through all business sectors, and promotes ingenuity and knowledge sharing, are especially successful. Moreover, communication and a consistent, comprehensive implementation strategy have a strong influence on the success of an innovation.
Include Clinician Leadership in the Top Tiers of Management
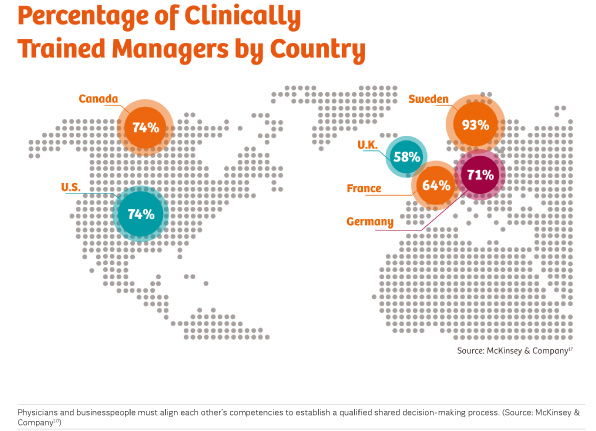
Innovations that are removed from patients, such as improved logistics and accounting processes, may represent very sound, sensible investments. However, these innovations contribute less to building a good reputation or a strong competitive position for a hospital than innovations that directly contribute to improving clinical capabilities.3 While it is increasingly being recognized that clinician leadership within hospitals is not only beneficial, but essential, to ensuring that hospitals implement the kinds of patient-centered innovations that are needed to remain competitive, increasing such leadership can remain an elusive goal. When institutions make investment decisions, the focus is often more on the purchasing costs and return on investment (ROI) rather than their impact on patient outcomes, patient safety, and employee satisfaction. In order to identify and implement promising innovations with beneficial effects on clinical capabilities, physicians and business leaders must align each other’s competencies to establish a qualified, shared decision-making process. This enables traditionally more numbers-oriented managers to develop a necessary understanding of the mindset and needs of their medical departments – and vice versa.
Pursue Innovation in eHealth
Electronic medical record digitization is transforming the flow of information and access to healthcare services – with corresponding implications for patient outcomes and treatment costs. The emerging telemedicine market provides underserved rural populations in emerging countries with access to medical expertise for the first time.4 Furthermore, telemedicine has proven to contribute to improvements in diagnosis and treatment for aging populations5 and chronically ill patients.6 Suitable partners for hospital operators can also come from other industries, such as the retail, technology, telecommunications, and consumer products sectors, and can often innovate at a faster pace than traditional healthcare companies, with lower costs.
Improve Outcomes through
Innovative Service Delivery Models
Integrated care programs have the potential to more adequately respond to the comprehensive needs of people with multi-morbidities by taking a holistic approach, while making efficient use of resources. Such programs are characterized by patient-centered, proactive, and coordinated multidisciplinary care, using new technologies to support patients’ self-management and improve collaboration between caregivers.7 The program shows that improved treatment results don’t necessarily require groundbreaking technical innovations. Instead, significant progress can often be made through targeted knowledge and information exchange as part of an organizational innovation.7
Consider Specialization Instead of Diversification
A critical mass of patient cases is a prerequisite for capability advancements in any institution. Disease-specific competency centers or service lines support hospitals in becoming established as clinical opinion leaders, recruiting highly qualified staff, and investing more successfully in technical equipment. Experience derived from managing a large number of cases can also increase clinical capabilities and thereby improve patient outcomes. One way that hospitals can effectively attract more patients and enhance their clinical experience and capabilities is to organize themselves by service lines in strategically defined clinical areas. By developing a focused service-line strategy, hospitals can also free up additional financial resources, which can then be redirected to further improve their clinical capabilities in key areas with investments in modern, patient- and user-friendly technical equipment and/or innovative services and care concepts.
Cultivate Opinion Leaders to Drive Patient
Demand, Attract Qualified Staff, and Enhance your Institution’s Reputation Opinion leaders represent an often untapped resource for hospitals to ensure that patients receive medical care based on the best evidence. They can have a significant influence on whether (and how quickly) innovations are implemented in clinical practice for the benefit of patients. As respected and well-connected sources of information, they can serve as a bridge from bench to bedside to span the knowledge-translation gap, through the early adoption of new evidence and subsequently influencing the majority of practitioners
In a Nutshell:Seven innovation
strategies to extend clinical capabilities
Invest In Clinical Technology to Improve Outcomes and Expand Services
Innovative medical technology directly influences clinical capabilities. Service providers need an outcomes-based investment strategy designed to advance their clinical capabilities, and a fleet management approach that supports stateof-the-art, outcome-based medicine.
Use Patient-Centered Process Innovations to Expand Clinical Capabilities
Process innovations that are close to the patient, and in the field of care, help increase patient and employee satisfaction as well as treatment and process quality, and hence a hospital’s reputation and market success.
Include Clinician Leadership in the Top Tiers of Management
To synchronize innovation budgets and clinical capabilities, medical and business management teams should interact as equals.
Pursue Innovation in ehealth
Electronic medical record digitization is transforming the flow of information and access to healthcare services, with corresponding implications for improving patient outcomes and reducing treatment costs.
Improve Outcomes through Innovative Service Delivery Models
Integrated care programs have the potential to more adequately respond to the comprehensive needs of people with multimorbidities by taking a holistic approach, while making efficient use of resources.
Consider Specialization Instead of Diversification
Disease-specific competency centers or service lines support hospitals in becoming established as clinical opinion leaders, recruiting highly qualified staff, and investing more successfully in technical equipment.
Cultivate Opinion Leaders
Opinion leaders represent an often untapped resource for hospitals to ensure that patients receive medical care based on the best evidence. They can have a significant influence on whether (and how quickly) innovations are implemented in clinical practice. Furthermore, they bolster a service provider’s reputation,attracting high-quality staff, as well as patients.

References:
1 Batlle, J.C., et al. (2010). Patients Imaged Early During Admission Demonstrate Reduced Length Of Hospital Stay: A Retrospective Cohort Study Of Patients Undergoing Cross-Sectional Imaging. Journal of the American College of Radiology, 7(4), pp. 269-276.
2 PwC. Unleashing the Power of Innovation. http://www.pwc.com/gx/en/innovationsurvey/files/innovation_full_report.pdf. Accessed October 2016.
3 PwC. (2015). Innovation – Deutsche Wege zum Erfolg. https://www.pwc.de/de/
publikationen/paid_pubs/pwc_innovation_-_deutsche_wege_zum_erfolg_2015.
pdf. Accessed October 2016.
4 Lewis, T., et al. (2012). E-health in Low- and Middle-Income Countries: Findings from the Center for Health Market Innovations. Bulletin of the World Health Organization. Geneva, Switzerland: (90) 5. May 2012. www.scielosp.org/scielo.php?pid=S0042-96862012000500008&script=sci_arttext. Accessed October 2016.
5 Shah, M.N., et al. (2013). High-Intensity Telemedicine-Enhanced Acute Care for
Older Adults: An Innovative Healthcare Delivery Model. Journal of the American
Geriatrics Society. Vol. 61, pp. 2000-2007.
6 Bashshur, R.L., et al. (2014). The Empirical Foundations of Telemedicine Interventions for Chronic Disease Management. Telemedicine and e-Health. 20(9), pp. 769-800.
7 Struckmann, V., et al. (2016). The Gesundes Kinzigtal Programme, Germany. Icare4EU. http://www.icare4eu.org/pdf/Gesundes_Kinzigtal.pdf. Accessed October 2016.
8 Baghai, R., et al. (2008). Service-Line Strategies for US Hospitals. The McKinsey Quarterly. http://healthcare.mckinsey.com/sites/default/files/737801_Serviceline_
strategies_for_US_hospitals__.pdf. Accessed October 2016.
9 American Hospital Association. (2016). Paving the Way for a New Era of Clinician
Leadership. AHA Solutions Insights. Vol. 2, Issue 3. http://www.aha-solutions.org/
newsletter/v2-i3/feature.shtml. Accessed October 2016.
10 McKinsey & Company. (2011). Management Matters in Healthcare. http://cep.lse.
ac.uk/textonly/_new/research/productivity/management/PDF/Management_in_
Healthcare_Presentation.pdf. Accessed October 2016.
11 Doumit, G., et al. (2007). Local Opinion Leaders: Effects on Professional Practice and Health Care Outcomes. Cochrane Database Syst. Rev. www.ncbi.nlm.nih.gov/pubmed/17253445. Accessed October 2016.


