A new magnetic resonance imaging (MRI) study published in the journal Radiology indicates that heart ages differently in men and women. Researchers from Johns Hopkins say the findings may support the development of gender-specific treatments for heart disease.
Previous studies have shown that in both sexes, the main heart chamber, the left ventricle — which fills with and then forces out blood — gets smaller with time. As a result, less blood enters the heart and less gets pumped out to the rest of the body. Many of these studies have been cross-sectional, or focused on one point in time, and based on comparisons between the young and old, which doesn't account for different lifestyles and other historical factors.
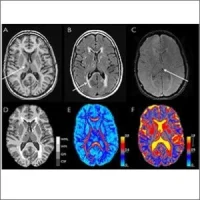
The new study is believed to be the first long-term follow-up using MRI showing how hearts change as they age. Researchers were able to assess long-term changes in the same people by acquiring a baseline cardiac MRI and then comparing it with another taken at a later date.
"We had the opportunity to re-examine the same people after 10 years so that we could see what happened to their hearts after a decade," says lead investigator John Eng, MD, from Johns Hopkins University School of Medicine in Baltimore. "This is a more reliable way to assess left ventricular changes over time."
For the study, researchers analysed MRI scans performed on nearly 3,000 older adults, ages 54 to 94, without pre-existing heart disease. Participants were followed between 2002 and 2012, at six hospitals across the U.S. where each one of them underwent MRI testing at the beginning of the study and once more after a decade.
Over a period of 10 years, left ventricular mass increased by an average of 8 grams in men and decreased by 1.6 grams in women. The heart’s filling capacity — marked by the amount of blood the left ventricle can hold between heartbeats — declined in both sexes but more precipitously so in women, by about 13 ml, compared with just under 10 ml in men. The differences in size, volume and pumping ability occurred independently of other risk factors known to affect heart muscle size and performance, including body weight, blood pressure, cholesterol levels, exercise levels and smoking.
The reasons for the differences between left ventricular mass in men and women will require more research, Dr. Eng points out. However, the findings suggest that optimum treatment for heart failure might not be the same for women and men. "We've been talking a lot lately about personalised medicine, and here's an example where perhaps men and women might have to be treated differently," according to Dr. Eng.
The study is part of an ongoing, long-term project called the Multi-Ethnic Study of Atherosclerosis (MESA), a large observational study focused on cardiovascular disease. The study was designed to enrol adults with no symptoms of heart disease to determine who develops heart disease or heart failure, what factors precipitate the disease and who is more likely to die from it.
Source: Johns Hopkins Medicine
Image credit: Flickr.com
Previous studies have shown that in both sexes, the main heart chamber, the left ventricle — which fills with and then forces out blood — gets smaller with time. As a result, less blood enters the heart and less gets pumped out to the rest of the body. Many of these studies have been cross-sectional, or focused on one point in time, and based on comparisons between the young and old, which doesn't account for different lifestyles and other historical factors.
The new study is believed to be the first long-term follow-up using MRI showing how hearts change as they age. Researchers were able to assess long-term changes in the same people by acquiring a baseline cardiac MRI and then comparing it with another taken at a later date.
"We had the opportunity to re-examine the same people after 10 years so that we could see what happened to their hearts after a decade," says lead investigator John Eng, MD, from Johns Hopkins University School of Medicine in Baltimore. "This is a more reliable way to assess left ventricular changes over time."
For the study, researchers analysed MRI scans performed on nearly 3,000 older adults, ages 54 to 94, without pre-existing heart disease. Participants were followed between 2002 and 2012, at six hospitals across the U.S. where each one of them underwent MRI testing at the beginning of the study and once more after a decade.
Over a period of 10 years, left ventricular mass increased by an average of 8 grams in men and decreased by 1.6 grams in women. The heart’s filling capacity — marked by the amount of blood the left ventricle can hold between heartbeats — declined in both sexes but more precipitously so in women, by about 13 ml, compared with just under 10 ml in men. The differences in size, volume and pumping ability occurred independently of other risk factors known to affect heart muscle size and performance, including body weight, blood pressure, cholesterol levels, exercise levels and smoking.
The reasons for the differences between left ventricular mass in men and women will require more research, Dr. Eng points out. However, the findings suggest that optimum treatment for heart failure might not be the same for women and men. "We've been talking a lot lately about personalised medicine, and here's an example where perhaps men and women might have to be treated differently," according to Dr. Eng.
The study is part of an ongoing, long-term project called the Multi-Ethnic Study of Atherosclerosis (MESA), a large observational study focused on cardiovascular disease. The study was designed to enrol adults with no symptoms of heart disease to determine who develops heart disease or heart failure, what factors precipitate the disease and who is more likely to die from it.
Source: Johns Hopkins Medicine
Image credit: Flickr.com
Latest Articles
heartmanagement, Johns Hopkins, heart disease, heart failure, MRI scans, left ventricle
A new magnetic resonance imaging (MRI) study published in the journal Radiology indicates that heart ages differently in men and women. Researchers from Johns Hopkins say the findings may support the development of gender-specific treatments for heart dis