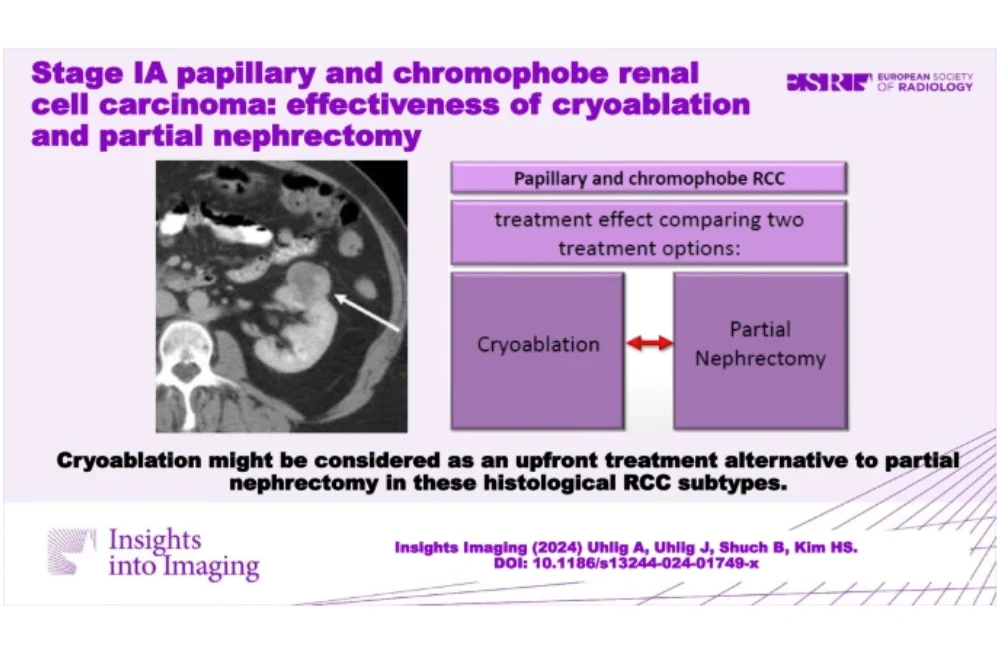
Renal cancer, the most prevalent malignancy of the kidneys, accounted for 431,288 cases and 179,368 deaths worldwide in 2020. Over recent decades, the incidence of renal cancer has surged, partly due to advancements in radiological imaging, enabling earlier detection of localised tumours. Renal cell carcinoma (RCC), comprising about 90-95% of renal cancers, includes subtypes such as clear cell RCC (ccRCC), papillary RCC (pRCC), and chromophobe RCC (chRCC). Treatment often involves surgical resection or thermal ablation, but the effectiveness of these treatments, particularly cryoablation (CRA), varies by RCC subtype. A recent study published in Insights into Imaging examines the comparative effectiveness of CRA versus partial nephrectomy (PN) in treating pRCC and chRCC.
Advances in RCC Detection and Treatment
The increase in renal cancer detection can be attributed to technological advancements and the widespread use of radiological cross-sectional imaging. Typically, these tumours are detected at a smaller diameter and are often localised to the kidney, classified as T1a (≤4 cm) or T1b (≤7 cm) without nodal or distant metastases (AJCC stage I A/B). Early detection has allowed for more effective treatment interventions, with surgical resection through partial nephrectomy remaining the standard treatment for early-stage RCC. However, CRA has emerged as a viable alternative, especially for smaller tumours or patients with comorbidities. CRA uses freezing and thaw cycles to induce tumour cell death, boasting a high technical success rate and a low complication profile.
Comparative Effectiveness of CRA and PN
Historically, studies comparing PN to CRA have primarily focused on ccRCC, leaving a gap in understanding regarding the effectiveness of CRA for less common subtypes like pRCC and chRCC. Recent analyses from the National Cancer Database (NCDB) indicate that the overall survival (OS) for patients with these subtypes may not significantly differ between CRA and PN treatments. For instance, in a study involving 11,122 stage I RCC patients, the OS rates between CRA and PN were comparable for pRCC and chRCC after adjusting for confounders. This suggests that CRA could be a suitable alternative to PN, especially for patients with smaller tumours or those unsuitable for surgery due to other health conditions.
Factors Influencing Treatment Outcomes
Several factors influence the outcomes of CRA and PN in RCC treatment. The cellular origins and prognostic profiles of RCC subtypes play a crucial role. For example, pRCC and chRCC have lower risks of local recurrence and metastasis compared to ccRCC, which may contribute to the comparable OS rates observed. Furthermore, technical aspects of CRA, such as the tumour's location within the kidney and the procedure's specifics (e.g., number of probes, freeze-thaw cycles), also impact effectiveness. Studies have shown that tumours with lower microvessel density, typically seen in pRCC and chRCC, respond better to CRA due to reduced "cold-sink" effects, where nearby blood vessels dissipate the cold, reducing ablation efficacy.
Clinical Implications and the Way Forward
This study highlights that CRA and PN offer similar overall survival outcomes for patients with stage IA pRCC and chRCC. These findings support the notion that CRA is a viable treatment alternative to PN, especially for patients who are frail or have comorbidities that make surgery risky. The favourable complication profile of CRA further reinforces its potential as a primary treatment option. However, further prospective studies are necessary to validate these findings and explore additional outcomes such as recurrence-free survival and cancer-specific survival. As the ability to identify RCC subtypes before treatment improves, personalised treatment strategies will become increasingly critical in optimising patient outcomes.
In conclusion, CRA provides a promising alternative to PN for treating certain RCC subtypes, with comparable effectiveness and a better complication profile. This approach aligns with the trend towards personalised medicine, ensuring that treatment plans are tailored to the individual characteristics of each patient's cancer. Future research should focus on confirming these results in controlled settings and expanding the understanding of CRA's effectiveness across different RCC subtypes and patient populations.
Source & Image Credit: Insights into Imaging