Use of imaging referral guidelines has been shown to improve appropriateness of imaging, reducing numbers of examinations typically by 20%. In the UK, the relatively low per caput dose (<20% versus 48% in the U.S.) is attributed largely through the appropriate use of clinical radiology.
Imaging referral guidelines with dose information are required to be available under the European Medical Directive 2013/59 Euratom and the UK Ionising Radiology (Medical Exposures) Regulations 2000 (IRMER). The Royal College of Radiologists (RCR) has published referral guidelines for over 20 years principally to guide general practitioners (GPs) and non-specialist clinicians. Although not every guideline can be implemented immediately on publication, mechanisms should be in place to ensure that practice is reviewed against the guideline recommendations and the reasons for any differences assessed and, where appropriate, addressed.
IRMER impose a responsibility on imaging departments to ensure that all exposures to ionising radiation are justified. Guidelines assist ICRP (International Commission on Radiological Protection) level 2 justification when ionising radiation examinations are used, and especially, for high-dose procedures such as CT. Vetting of MRI examinations is equally important to ensure good medical practice and cost effectiveness. The need for clinical audit to monitor justification has been set out in the Euratom Directive and highlighted in the International Basic Safety Standards.
This study aims to audit the availability of imaging referral guidelines; vetting by radiologists of GP-initiated CT and MRI requests; and the achievement of appropriate imaging using retrospective assessment as a surrogate.
Materials and methods
The standards adopted for this audit are based partly on legislation and partly on expert consensus by the RCR Clinical Radiology Audit Committee (CRAC). Three standards based on the audit principles of structure, process, and outcome were used: (1) imaging referral guidelines with dose information should be available to all justifying practitioners (radiologists and radiographers to whom the task of justification has been delegated). As this is a mandatory duty under IRMER, the target is 100%; (2) all requests for CT and MRI from GPs should be vetted individually or through an agreed protocol. To take into account emergency referrals, the target is 95%; (3) compliance with guidelines, where applicable, should be demonstrated for GP-requested CT and MRI examinations (excluding subsequent investigations, usually for problem-solving, initiated at the recommendation of a radiologist). To take into account individual patient needs and contraindications (eg, pacemakers) the target is set at 90%.
A web-based questionnaire requesting anonymised data was devised by the RCR CRAC and distributed to imaging departments in the UK to determine the following: awareness of guideline availability; the percentage of consecutive general practitioner (GP)-requested computed tomography (CT) and magnetic resonance imaging (MRI) investigations that showed evidence of vetting; and the percentage of procedures where retrospective assessment showed the investigation to be appropriate according to imaging referral guidelines.
Results
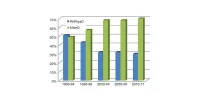
Replies were received from 88 departments covering 1,700 of 2,700 (63%) consultant radiologists practising in the UK. Regarding the availability of guidelines, approximately a third of respondents were not aware of guidelines being available to all radiologists and radiographers. The 68% level of availability (58/88 departments) is well below the standard of 100%.
In keeping with the target of 95%, vetting of CT requests was shown in 1815/1890 (96%) and MRI in 1181/1250 (95%). The majority of departments are within the upper and lower control limits indicating common cause for variation (ie, approaching normal distribution) with few low outliers.
Appropriateness of CT examinations was shown in 1746/1870 (93%) and MRI in 1154/1215 (95%), well above the target of 90%. Analysis of the 7-8% inappropriate investigations showed that CT was often not the best investigation. The most common reason for an inappropriate investigation for both MRI and CT was the inability to affect patient management.
Discussion And Conclusion
Lack of awareness of guideline availability may not be the same as non-availability of guidelines. Possible reasons for failure to reach the 100% standard of guideline availability include the fact that only 58/88 (66%) of departments have online access. Half of all departments still use paper copy. Since this audit was performed, the shortfall in online access has been addressed.
Limitations of the present study include the narrow focus on GP-requested CT and MRI. Although extrapolation to other referrers seems logical, requests from GPs have particular challenges different to those from hospital doctors. Strategies for improvement in appropriate imaging will differ according to the referrer, their availability for discussion, and feedback. Future studies including other imaging techniques, especially ultrasound, would provide a more representative view.
In conclusion, although awareness of referral guidelines availability was limited at 68%, well below the 100% standard, the meticulous vetting of requests (shown in 95ñ96%) with the amendment or return of inappropriate requests (9-12%) enables a high level of appropriate imaging (93-95%) for GP-requested CT and MRI, thus making the best use of clinical radiology.
Reference:
Remedios D, Drinkwater K, Warwick R (2014) On behalf of the Clinical Radiology Audit Committee (CRAC), The Royal College of Radiologists, London. National audit of appropriate imaging. Clinical Radiology, available online 16 July 2014, DOI: 10.1016/j.crad.2014.05.109.
Image credit: Freeimages.com
Imaging referral guidelines with dose information are required to be available under the European Medical Directive 2013/59 Euratom and the UK Ionising Radiology (Medical Exposures) Regulations 2000 (IRMER). The Royal College of Radiologists (RCR) has published referral guidelines for over 20 years principally to guide general practitioners (GPs) and non-specialist clinicians. Although not every guideline can be implemented immediately on publication, mechanisms should be in place to ensure that practice is reviewed against the guideline recommendations and the reasons for any differences assessed and, where appropriate, addressed.
IRMER impose a responsibility on imaging departments to ensure that all exposures to ionising radiation are justified. Guidelines assist ICRP (International Commission on Radiological Protection) level 2 justification when ionising radiation examinations are used, and especially, for high-dose procedures such as CT. Vetting of MRI examinations is equally important to ensure good medical practice and cost effectiveness. The need for clinical audit to monitor justification has been set out in the Euratom Directive and highlighted in the International Basic Safety Standards.
This study aims to audit the availability of imaging referral guidelines; vetting by radiologists of GP-initiated CT and MRI requests; and the achievement of appropriate imaging using retrospective assessment as a surrogate.
Materials and methods
The standards adopted for this audit are based partly on legislation and partly on expert consensus by the RCR Clinical Radiology Audit Committee (CRAC). Three standards based on the audit principles of structure, process, and outcome were used: (1) imaging referral guidelines with dose information should be available to all justifying practitioners (radiologists and radiographers to whom the task of justification has been delegated). As this is a mandatory duty under IRMER, the target is 100%; (2) all requests for CT and MRI from GPs should be vetted individually or through an agreed protocol. To take into account emergency referrals, the target is 95%; (3) compliance with guidelines, where applicable, should be demonstrated for GP-requested CT and MRI examinations (excluding subsequent investigations, usually for problem-solving, initiated at the recommendation of a radiologist). To take into account individual patient needs and contraindications (eg, pacemakers) the target is set at 90%.
A web-based questionnaire requesting anonymised data was devised by the RCR CRAC and distributed to imaging departments in the UK to determine the following: awareness of guideline availability; the percentage of consecutive general practitioner (GP)-requested computed tomography (CT) and magnetic resonance imaging (MRI) investigations that showed evidence of vetting; and the percentage of procedures where retrospective assessment showed the investigation to be appropriate according to imaging referral guidelines.
Results
Replies were received from 88 departments covering 1,700 of 2,700 (63%) consultant radiologists practising in the UK. Regarding the availability of guidelines, approximately a third of respondents were not aware of guidelines being available to all radiologists and radiographers. The 68% level of availability (58/88 departments) is well below the standard of 100%.
In keeping with the target of 95%, vetting of CT requests was shown in 1815/1890 (96%) and MRI in 1181/1250 (95%). The majority of departments are within the upper and lower control limits indicating common cause for variation (ie, approaching normal distribution) with few low outliers.
Appropriateness of CT examinations was shown in 1746/1870 (93%) and MRI in 1154/1215 (95%), well above the target of 90%. Analysis of the 7-8% inappropriate investigations showed that CT was often not the best investigation. The most common reason for an inappropriate investigation for both MRI and CT was the inability to affect patient management.
Discussion And Conclusion
Lack of awareness of guideline availability may not be the same as non-availability of guidelines. Possible reasons for failure to reach the 100% standard of guideline availability include the fact that only 58/88 (66%) of departments have online access. Half of all departments still use paper copy. Since this audit was performed, the shortfall in online access has been addressed.
Limitations of the present study include the narrow focus on GP-requested CT and MRI. Although extrapolation to other referrers seems logical, requests from GPs have particular challenges different to those from hospital doctors. Strategies for improvement in appropriate imaging will differ according to the referrer, their availability for discussion, and feedback. Future studies including other imaging techniques, especially ultrasound, would provide a more representative view.
In conclusion, although awareness of referral guidelines availability was limited at 68%, well below the 100% standard, the meticulous vetting of requests (shown in 95ñ96%) with the amendment or return of inappropriate requests (9-12%) enables a high level of appropriate imaging (93-95%) for GP-requested CT and MRI, thus making the best use of clinical radiology.
Reference:
Remedios D, Drinkwater K, Warwick R (2014) On behalf of the Clinical Radiology Audit Committee (CRAC), The Royal College of Radiologists, London. National audit of appropriate imaging. Clinical Radiology, available online 16 July 2014, DOI: 10.1016/j.crad.2014.05.109.
Image credit: Freeimages.com
Latest Articles
Imaging, Guidelines, Radiology, Quality
Use of imaging referral guidelines has been shown to improve appropriateness of imaging, reducing numbers of examinations typically by 20%. In the UK, the...