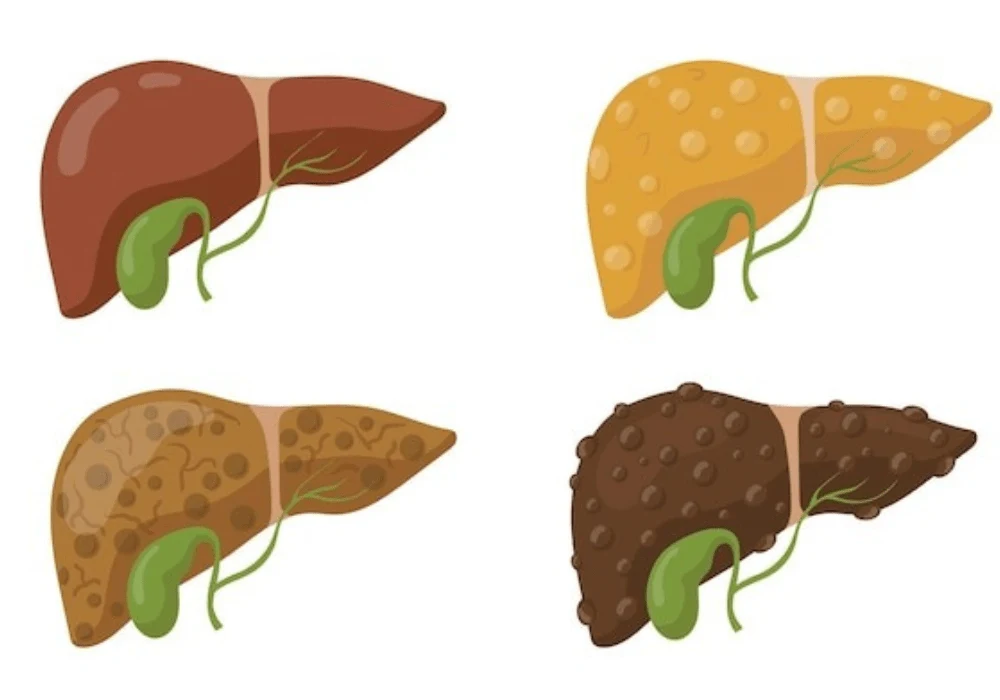
Metabolic dysfunction-associated steatotic liver disease (MASLD) has emerged as a prevalent and pressing global health concern, driven largely by rising rates of obesity and metabolic syndrome. Characterised by the accumulation of fat in hepatocytes, MASLD can progress to more severe conditions, including steatohepatitis, fibrosis and even liver failure or cancer.
Accurate grading of hepatic steatosis is essential for effective management and intervention. While liver biopsy remains the diagnostic gold standard, its invasive nature limits broad applicability. Consequently, non-invasive imaging modalities—particularly magnetic resonance imaging proton density fat fraction (MRI-PDFF), controlled attenuation parameter (CAP) and attenuation coefficient (AC)—have been extensively studied as alternatives. A recent meta-analysis consolidates data from 38 studies, involving over 5000 patients, to assess the performance of these techniques against biopsy-verified diagnoses.
Diagnostic Performance of MRI-PDFF, CAP and AC
The study assessed the diagnostic accuracy of MRI-PDFF, CAP and AC across various steatosis grades—mild (≥S1), moderate (≥S2) and severe (≥S3). MRI-PDFF showed the highest diagnostic performance, with area under the curve (AUC) values of 0.99 for ≥S1, 0.89 for ≥S2 and 0.90 for ≥S3. CAP demonstrated slightly lower performance, particularly in diagnosing moderate and severe steatosis, with AUCs of 0.95, 0.84 and 0.77 for ≥S1, ≥S2 and ≥S3, respectively. AC provided competitive results, showing AUCs of 0.97, 0.90 and 0.89 for the respective grades.
Pooled sensitivity and specificity analyses revealed similar patterns. MRI-PDFF maintained high sensitivity and specificity, particularly for ≥S1 (95% and 98%, respectively). CAP achieved good sensitivity for all grades but lagged in specificity for ≥S2 (70%) and ≥S3 (65%). AC consistently delivered strong sensitivity and specificity across all grades, indicating its potential reliability.
Comparative analysis revealed that CAP underperformed in detecting ≥S2 and ≥S3 when compared to MRI-PDFF and AC, with statistically significant differences. This discrepancy highlights the limitation of CAP in stratifying steatosis severity, particularly in clinical populations where higher grades are more prevalent.
Influence of Patient Demographics on Diagnostic Accuracy
The meta-analysis further explored the influence of variables such as age, body mass index (BMI) and geographical region. Subgroup analyses identified that MRI-PDFF and CAP had greater accuracy in younger individuals (under 51 years) and those with a BMI ≤30 kg/m². Among Asian populations, CAP and MRI-PDFF demonstrated improved diagnostic performance in identifying both moderate and severe steatosis.
Age and BMI had a noticeable impact on sensitivity and specificity across modalities. MRI-PDFF yielded better sensitivity in patients younger than 51, while specificity was higher among those older than 51 for diagnosing ≥S3. CAP's performance decreased in patients with higher BMI, likely due to limitations in signal penetration and increased variability in measurements. Similarly, CAP was more accurate in populations with lower BMI, particularly in Asia, where individuals tend to have less subcutaneous fat, allowing clearer imaging.
Must Read: Assessing Steatosis via Photon-counting CT
For AC, the influence of demographic variables was less pronounced, with consistent performance across subgroups. The lack of heterogeneity in AC’s diagnostic performance suggests it may be more robust across diverse populations. However, variability between ultrasound systems used to derive AC could affect broader adoption until standardisation is achieved.
Clinical Recommendations and Utility
The findings support integrating AC into routine clinical practice, especially during ultrasound examinations for patients at risk of MASLD. MRI-PDFF, although highly accurate, remains costly and less accessible, limiting its routine use. CAP, while commonly used, is best suited for detecting mild steatosis and may be more appropriate for assessing liver fibrosis rather than steatosis stratification.
The Fagan nomogram analysis underscored the clinical relevance of each method. MRI-PDFF offered the highest post-test probability (95%) for positive results and the lowest for negative (2%). AC followed closely, with a 91% positive and 7% negative post-test probability, while CAP showed 80% and 6%, respectively. These metrics affirm the strong diagnostic power of MRI-PDFF and AC, with AC offering a practical balance between accuracy and accessibility.
Despite the advantages of AC, current limitations include variation in measurements across different ultrasound systems, necessitating cautious interpretation until standardisation is achieved. The study recommends adopting AC broadly in ultrasound screening while reserving MRI-PDFF for settings that require high diagnostic precision or serve as clinical reference standards. CAP’s role, though limited in steatosis grading, remains valid in fibrosis detection.
This comprehensive analysis of non-invasive imaging techniques for hepatic steatosis underscores the superior accuracy of MRI-PDFF and AC, particularly in identifying moderate and severe disease stages. MRI-PDFF stands out as a non-invasive reference standard, though its use is constrained by availability and cost. AC, on the other hand, offers an effective and accessible alternative that enhances routine ultrasound screening. CAP, while less effective for detailed steatosis grading, still serves a valuable role in broader liver assessments. Incorporating AC into standard diagnostic protocols presents a practical path forward in the early detection and management of MASLD. As future studies refine these approaches and address current limitations, the diagnostic landscape for hepatic steatosis is set to become both more accurate and more inclusive.
Source: Academic Radiology
Image Credit: Freepik