Close collaboration between the emergency department (ED) and intensive care unit (ICU) and standardised ICU admission criteria for patients with sepsis can significantly reduce mortality rate and care costs, according to new research published in CHEST Journal.
"Although ICU level of care is costly, earlier inclusion of borderline patients may improve mortality," says lead researcher Joseph Carrington, MD, Northwest Hospital and Lifebridge Critical Care in Randallstown, Maryland. "It may also significantly decrease resource utilisation, as our study found."
For this study, Dr. Carrington and his colleague, Jaime Barnes, DO, also of Northwest Hospital, reviewed 886 medical records from patients with sepsis admitted to the ICU of a community hospital. There was collaboration between the ED and ICU in admitting traditionally “borderline” patients to the ICU, as well as utilising standardised ICU admission criteria for septic patients.
The researchers compared mortality and length of stay before and after making ICU admission criteria less stringent for patients with sepsis. They found that upon easing of ICU admission criteria, overall mortality decreased by 45.4 percent (from 14.38 percent to 7.85 percent). Although the severity of the illness did not change, ICU length of stay was 25.9 percent lower in the post-implementation cohort (3.97 days vs. 2.94 days). In addition, the number of intermediate care unit patients who were transferred to the ICU also decreased by 67.1 percent (from 3.89 percent to 1.28 percent).
"In addition to improved outcomes, annualised cost savings in our new model were $2,286,600 (based on average cost of $2,500/ICU-day)," the authors write.
The results show that developing a collaborative culture between the ED and ICU and lowering ICU admission thresholds not only provide smarter use of ICUs but may also help improve annual cost savings in hospitals, according to the authors.
Further results will be shared during CHEST Annual Meeting 2015, held in Montréal, Canada on 24-28 October.
Source: American College of Chest Physicians
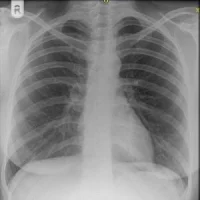
Image credit: Flickr.com
"Although ICU level of care is costly, earlier inclusion of borderline patients may improve mortality," says lead researcher Joseph Carrington, MD, Northwest Hospital and Lifebridge Critical Care in Randallstown, Maryland. "It may also significantly decrease resource utilisation, as our study found."
For this study, Dr. Carrington and his colleague, Jaime Barnes, DO, also of Northwest Hospital, reviewed 886 medical records from patients with sepsis admitted to the ICU of a community hospital. There was collaboration between the ED and ICU in admitting traditionally “borderline” patients to the ICU, as well as utilising standardised ICU admission criteria for septic patients.
The researchers compared mortality and length of stay before and after making ICU admission criteria less stringent for patients with sepsis. They found that upon easing of ICU admission criteria, overall mortality decreased by 45.4 percent (from 14.38 percent to 7.85 percent). Although the severity of the illness did not change, ICU length of stay was 25.9 percent lower in the post-implementation cohort (3.97 days vs. 2.94 days). In addition, the number of intermediate care unit patients who were transferred to the ICU also decreased by 67.1 percent (from 3.89 percent to 1.28 percent).
"In addition to improved outcomes, annualised cost savings in our new model were $2,286,600 (based on average cost of $2,500/ICU-day)," the authors write.
The results show that developing a collaborative culture between the ED and ICU and lowering ICU admission thresholds not only provide smarter use of ICUs but may also help improve annual cost savings in hospitals, according to the authors.
Further results will be shared during CHEST Annual Meeting 2015, held in Montréal, Canada on 24-28 October.
Source: American College of Chest Physicians
Image credit: Flickr.com
References:
Carrington J, Barnes J (2015) Making ICU Admissions Smarter, Not Making Them Harder: Lowering ICU Admission Thresholds Improves Outcomes and Resource Utilization. Chest. October 2015;148(4_MeetingAbstracts):246A. doi:
10.1378/chest.2270816
10.1378/chest.2270816
Latest Articles
healthmanagement, emergency department, length of stay, intensive care unit, sepsis, mortality, cost savings
Close collaboration between the emergency department (ED) and intensive care unit (ICU) and standardised ICU admission criteria for patients with sepsis can significantly reduce mortality rate and care costs, according to new research published in CHEST J