ICU Management & Practice, Volume 22 - Issue 2, 2022
Introduction
Sepsis is a dysregulated host immune response to infection resulting in acute injury to potentially multiple organs. It is a major cause for morbidity and mortality worldwide (Rhodes et al. 2017). The majority of sepsis patients are from the community but the mortality and associated cost of caring for patients (>50,000 USD) are significantly higher with nosocomial sepsis (Paoli et al. 2018; Rhee et al. 2019; Fay et al. 2020). Surprisingly, even previously healthy patients admitted with sepsis have a higher short-term mortality compared to those with comorbid conditions (adjusted OR 1.99 [95% CI 1.87-2.13]) (Alrawashdeh et al. 2022). There has been an increase in sepsis related hospitalisations in U.S. Medicare beneficiaries from 2012-2018 (Buchman et al. 2020). In that study, authors report that the long-term mortality from sepsis remains high despite advances in management over the last two decades (septic shock mortality at six months is approximately 60%) and the corresponding economic burden of skilled nursing care post discharge, increased over the six years of the study period (Buchman et al. 2020).
Bacterial infections of the lower respiratory tract are the most common cause of sepsis in ICU, although based on other risk factors, such as immunosuppression and exposure to antibiotics within 90 days, other pathogens including fungi and viruses can cause sepsis. Additional common sources of sepsis include intra-abdominal infections, blood stream infections, urinary tract infections, infected vascular access sites, and skin/soft tissue infection. Gram-negative pathogens are identified more commonly in cultures than gram-positives but over the last decade, the percentage of multidrug resistant (MDR) bacterial isolates is on the rise worldwide (Vincent et al. 2020). The most common gram-negative pathogens include Klebsiella species, E. coli, Pseudomonas species, Enterobacteriaceae, Proteus, Stenotrophomonas, Serratia and Acinetobacter species, whereas gram-positive isolates include S. aureus, S. pneumoniae, and Enterococcus, and fungal microorganisms were Candida species and Aspergillus (Vincent et al. 2020). MDR pathogens including extended spectrum beta-lactamase (ESBL) enzyme and Amp C enzyme producing E. coli, Klebsiella and carbapenem-resistant Klebsiella and Acinetobacter, and methicillin-resistant Staphylococcus aureus (MRSA) are independently associated with a higher mortality in ICU compared to infections with other organisms (Vincent et al. 2020). Risk factors for MRSA include prior history of MRSA infection or colonisation, recent IV antibiotics, history of recurrent skin infections or chronic wounds, presence of invasive devices, haemodialysis, and recent hospitalisation within 90 days. The risk of 30-day mortality is higher in patients with MDR pathogens and comorbid conditions, such as cirrhosis, immunosuppression or vascular disease but also in those who have received antibiotics, chemotherapy, wound care, dialysis, or surgery within the last 30 days prior to onset of sepsis (Fay et al. 2020). In this review, we focus on the antibacterial management of patients with sepsis admitted to ICU.
Heterogeneity of Sepsis Syndrome
Recent analysis of big data including 64,000 patients from three different clinical trials have shown that sepsis syndrome can be categorised into four different phenotypes based on demographics, laboratory values, and patterns of organ dysfunction, and this may have implications on clinical outcomes and mortality (Seymour et al. 2019). Gene expression profiling to detect the underlying molecular responses and characterising early septic patients have shown five distinct endotypes, each based on 200 unique gene expression differences and distinct pathways: neutrophilic suppressive, inflammatory, innate-host-defense, interferon, and adaptive (Baghela et al. 2022). Of these, the neutrophilic suppressive and inflammatory endotypes have a propensity to develop severe infection. In another study, investigators found significant differences in key immune and coagulation system pathways based on the source of infection but mortality differences were primarily dependent on the source of infection with abdominal and respiratory infections having slightly higher ICU mortality (Peters-Sengers et al. 2022).
Early Recognition Saves Lives
Surviving Sepsis Campaign 2016 guidelines emphasise early recognition of sepsis with a 1-hour bundle and administration of early appropriate antibiotics plus effective source control (Rhodes et al. 2017). For every hour’s delay in antimicrobial administration over the first 6-hrs since diagnosis of septic shock, there is a 7.6% increased risk of death (Kumar et al. 2006). A recent meta-analysis investigating the impact of delay in appropriate antibiotic therapy for hospitalised adult patients with bacterial infections showed significant reduction in treatment failure (OR 0.33, 95% CI 0.16-0.66), reduced mortality rates (OR 0.44, 95% CI 0.38-0.50) and mean hospital costs in those who had appropriate antibiotics (Bassetti et al. 2020). Patients, who received discordant empiric antibiotic therapy based on susceptibility to bacterial isolates had an increased risk of mortality independent of microbial resistance, sepsis or septic shock (adjusted odds ratio 1.46 [95% CI, 1.28–1.66]) (Kadri et al. 2021). The majority of discordant empirical antibiotic therapy and associated mortality were in patients with bloodstream infections caused by Staphylococcus aureus or Enterobacterales (Kadri et al. 2021). Data from a large study including 20,026 adults with suspected sepsis in 12 emergency departments showed that both delays in recognition of infection and administration of the antibiotics were associated with increased hospital mortality (Taylor et al. 2021).
The above evidence highlights the importance of rapid recognition and need for broad-spectrum empirical antimicrobial therapy in patients with suspected sepsis, preferably within 6-hours but immediately in patients with septic shock. However, rampant use of broad-spectrum antibiotics in the absence of proven infection is a risk factor for development of antibiotic resistant pathogens and excess mortality (Teshome et al. 2020). Thus, antibiotic stewardship is a key element in the management of sepsis with a commitment to narrow and stop antimicrobials based on culture data during the hospital stay (Wunderink et al. 2020). Another potential opportunity is to develop rapid and cost-effective diagnostics for early identification of the causative pathogen and resistance testing of positive blood culture using multiplex technologies (She and Bender 2019). Multiplex PCR can detect common bloodstream pathogens within a few hours compared to conventional blood cultures. Several systems including Verigene and FilmArray are commercially available as an adjunct to the conventional microbiology methods, and are used to detect microbial resistance rapidly (De Angelis et al. 2020).
Recently, next-generation sequencing using microbial cell-free DNA has been shown to have better sensitivity in detecting pathogens within hours compared to traditional blood culture in patients with a sepsis (Blauwkamp et al. 2019). Cost effectiveness models show incorporating molecular testing in emergency department in patients with sepsis and septic shock would significantly impact patients receiving inappropriate antibiotic therapy with an incremental cost-effectiveness ratio of negative $7,302/death averted (Zacharioudakis et al. 2019).
Biomarkers and Host Response Markers of Sepsis
A different tactic would be to measure the host response to infection rather than direct pathogen detection by using sepsis biomarkers to aide in the decision to start or stop antibiotics. Several markers including procalcitonin (PCT), C-reactive protein (CRP), soluble triggering receptors expressed on myeloid 1, proadrenomedullin, soluble urokinase plasminogen activator receptor and interleukin-6 have been studied in patients with sepsis (Masia et al. 2005; Kruger et al. 2008; Gunsolus et al. 2019). However, the currently available biomarkers lack discriminative diagnostic sensitivity on the decision to start empiric antibiotics in suspected sepsis and generally most societies endorse serial measurement for antibiotic stewardship efforts (Bouadma et al. 2010). In a patient-level meta-analysis, PCT guided antibiotic stewardship programme was able to significantly reduce days on antibiotics compared to controls with significant improvement in mortality (aOR 0.89, 95% CI:0.8 - 0.99; p = 0.03) (Wirz et al. 2018). Thus, checking serial biomarkers such as PCT and CRP can be of valuable assistance along with clinical judgement on decision to help decide on duration of treatment.
Despite advances in diagnostics and risk stratification, almost 47% of patients with sepsis have a negative-culture and failure to identify the causative pathogen limits opportunities for modification/narrowing of antibiotic spectrum (Gupta et al. 2016). Transcriptomics, targeting host immune gene expression (mRNA) profiling in response to infection is another emerging field with superior diagnostic and prognostic value compared to serum biomarkers in patients with early sepsis (Gunsolus et al. 2019). SeptiCyte LAB is a continuous output of a four-mRNA; CEACAM4, LAMP1, PLA2G7, and PLAC8 (Immunexpress, Seattle, WA) that has FDA clearance for detection of sepsis from systemic inflammatory response syndrome. Increasing scores from 1-10 shows a higher predilection for infectious cause independent of age, sex, race/ethnicity, clinical and other biomarkers, including PCT (Miller et al. 2018; Sweeney et al. 2016). In a study comparing 3-omics models based on host response, including Sepsis MetaScore, SeptiCyte and FAIM3:PLAC8 ratio, all three models showed good discriminative ability in distinguishing patients with sepsis (Maslove et al. 2019). Ultimately, the effectiveness of rapid diagnostics will depend on its ability to reduce days on broad-spectrum antibiotics, prevent delay of appropriate antibiotics, reduce mortality, and length of stay.
Antimicrobial Considerations
The 2021 Surviving Sepsis International guidelines recommend in adults with sepsis or septic shock at high risk of MRSA and MDR-gram negative organisms to start antibiotics with MRSA coverage and use two antimicrobials with gram-negative coverage for empiric coverage (Evans et al. 2021). However, the guidelines strongly advise against using MRSA coverage or dual gram-negative coverage in patients with low risk for both organisms and once susceptibilities have been identified (Evans et al. 2021). In a recent meta-analysis and trial sequential analysis including thirteen studies, there was no difference in mortality or other patient-related outcomes between mono- vs. combination therapy (Sjovall et al. 2017). Consideration for targeted therapy should be made after assessment of risk factors for MDR pathogens including prior colonisation in the preceding year, local prevalence, broad-spectrum antibiotic use within 90 days, use of selective digestive decontamination, type of infection – community vs. nosocomial, travel to highly endemic countries and hospitalisations abroad in the last 90 days (Evans et al. 2021).
On any given day, almost 70% of ICU patients receive empirical or targeted antimicrobial therapy (Timsit et al. 2019). The hospital antibiogram can aid in selecting empiric antibiotic treatments with a higher chance of covering pathogens based on prior local knowledge and sensitivity. However, it is not always practical in achieving 90% coverage often based on antibiograms, as it might mean using restricted antibiotics more often driving resistance in the community. Therefore, empiric antibiotic choices should include risk factors related with antibiotic resistance such as comorbid conditions, recent exposure to healthcare, immunosuppression; type of infection: community vs. nosocomial; selection pressure from prior antibiotic use; colonisation with prior drug resistant pathogens; local epidemiology and infection prevention measures (Timsit et al. 2019). Metagenomics with fast sequencing of nucleic acids of all bacterial pathogens and their resistance determinants in the future would aid with this workflow to limit duration and narrow spectrum to monotherapy.
It is imperative to not only use the appropriate antimicrobial agent but to use the appropriate dose based on the pharmacokinetic (PK)/dynamic (PD) properties, and for the optimal duration. Consideration should be given to the minimum inhibitory concentration (MIC) of the pathogen, volume of distribution (usually high in patients with sepsis), augmented renal clearance (ARC), presence of renal or liver failure altering drug metabolism, physiochemical nature of the drug like hydrophilic/lipophilic properties, use of organ support (continuous renal replacement therapy and extracorporeal membrane oxygenation) and the site of infection. Underdosing is common in sepsis due to large volume of distribution and ARC. Hence, an initial large bolus (1.5 x standard dose) loading dose is most often required in severe sepsis patients regardless of their organ function (De Backer et al. 2019). Beta-lactams work best with time-dependent killing and are usually administered in multiple daily doses or as a continuous infusion to keep the concentration above MIC, while other antibiotics such as aminoglycosides and quinolones exert their antimicrobial effects best by concentration-dependent killing and are usually administered with a single large daily dose.
Therapeutic Drug Monitoring (TDM) is another measure employed in ensuring appropriate and effective antibiotic use in severe sepsis patients due to the inherent flaws with prediction of PK/PD characteristics in this population (Timsit et al. 2020). TDM is especially beneficial for certain antibiotic classes and should be used with vancomycin and aminoglycosides; however there is lack of evidence on adoption of regular TDM with use of beta-lactams (Timsit et al. 2020). Antibiotics are also chosen based on the site of infection. Lipophilic drugs like quinolones provide high tissue concentrations but hydrophilic antibiotics such as aminoglycosides do not penetrate into tissue space and remain extravascular but often enough to exert their antimicrobial effects (De Backer et al. 2019).
Another important aspect is appropriate source control. Common scenarios include an obstructive stone in patients with sepsis related to urinary tract infection, cholecystitis with cholangitis, post pancreatitis infected phlegmon, skin and soft-tissue infections, infected intra-vascular or cardiac devices, empyema and surgical site infections. This should be followed by antimicrobial de-escalation (ADE) strategies that form the cornerstone for antibiotic stewardship programme to help reduce duration of antibiotics and emergence of MDR pathogens. ADE involves narrowing the spectrum of the initial antibiotic and/or decreasing the number of agents (Tabah et al. 2020). The majority of patients with sepsis related to pneumonia or post operative intra-abdominal infections can be treated with short course 5–7-day treatment. The Surviving Sepsis 2021 guidelines gave a conditional weak recommendation for limiting antibiotics to a short course in adults with an initial diagnosis of sepsis or septic shock and adequate source control (Evans et al. 2021). However, longer course might be needed with endocarditis and osteomyelitis, and certain MDR pathogens.
Newer Antimicrobial Agents
Over the last decade several new and combination antibiotics have been developed to treat severe sepsis patients with resistant gram positive and negative pathogens. These include fifth generation cephalosporins, cephalosporin/beta-lactam + beta-lactamase inhibitor regimens including ceftazidime-avibactam, ceftolozane-tazobactam, imipenem-relebactam, meropenem-vaborbactam, and cefiderocol (Sjovall et al. 2017). In general, ceftolozane-tazobactam, ceftazidime-avibactam and imipenem-relebactam are effective choices against highly drug resistant P. aeruginosa, whereas with carbapenem-resistant Enterobacteriaceae, ceftazidime-avibactam, imipenem-relebactam, and meropenem-vaborbactam are good options (Torres et al. 2018; Kollef et al. 2019; Torres et al. 2019). Ceftazidime-avibactam and cefiderocol are optimal choices for metallo-beta-lactamase producing pathogens (Tamma et al. 2020). Meropenem-vaborbactam has good activity against most gram-negative microorganisms, including those with extended-spectrum beta-lactamases and K. pneumoniae carbapenemases and carbapenem-resistant Enterobacteriaceae (CRE) (Wunderink et al. 2018). Imipenem-relebactam is another combination regimen effective against most gram-negative microorganisms (Titov et al. 2020). Vancomycin, oxazolidinones (linezolid), telavancin, teicoplanin and streptogramins retain good activity against MRSA infections. Ceftobiprole is a fifth-generation cephalosporin with extended spectrum activity against methicillin-sensitive S. aureus (MSSA), P. aeruginosa and Enterobacteriaceae, but limited efficacy against MRSA and ESBL producing gram negatives, and is not used in the United States (Cilloniz et al. 2019).
Antimicrobial Preferences in Pneumonia and Intra-abdominal Infections
Lower respiratory tract infections, both community-acquired pneumonia (CAP) and nosocomial (hospital acquired pneumonia - HAP) and ventilator associated pneumonia (VAP) along with intra-abdominal infections form the bulk of sepsis in the ICU. The guidelines for CAP and nosocomial pneumonias were recently updated and they emphasise initial empiric antimicrobial therapy based on risk factors for MDR pathogens and local resistance patterns.
The 2019 American Thoracic Society/Infectious Diseases Society of America (ATS/IDSA) consensus CAP guidelines recommend that patients with severe pneumonia requiring ICU admission, with no risk factors for MRSA or P. aeruginosa, be started on either a beta-lactam plus a macrolide or beta -lactam plus a respiratory fluoroquinolone (Metlay et al. 2019). Prior studies have shown a possible survival advantage in severe CAP patients with regimens containing a macrolide with its potential anti-inflammatory effects (Rodriguez et al. 2007; Sligl et al. 2014). However, a more recent systematic review found no difference in outcomes between either a beta-lactam plus macrolide or a beta-lactam plus fluoroquinolone (Vardakas et al. 2017). In general, monotherapy is avoided in severe CAP in the ICU as appropriate dosing and safety of any single agent has not been established. The 2019 ATS/IDSA guidelines recommend empiric MRSA and/or Pseudomonal coverage for CAP patients with risk factors for these pathogens, followed by de-escalation of therapy, if cultures return without growth of these organisms (Metlay et al. 2019). MRSA and Pseudomonas risks as described above are prior positive culture, recent hospitalisations and antibiotic exposure within 90 days. In patients suspected of having P. aeruginosa, a two-drug regimen, using an anti-pseudomonal beta-lactam (cefepime, imipenem, meropenem, piperacillin/tazobactam) plus ciprofloxacin or levofloxacin is generally recommended. Another potential combination therapy will be with a three-drug regimen combining an anti-Pseudomonal beta-lactam plus an aminoglycoside plus either an intravenous anti-pneumococcal quinolone (moxifloxacin or levofloxacin) or a macrolide (Mandell et al. 2007). In patients with suspected MRSA, either vancomycin or linezolid is preferred.
Similarly, the 2016 ATS/IDSA HAP-VAP guidelines also recommend empiric coverage based on MDR risk factors and local antibiogram (Kalil et al. 2016). The majority of patients should receive an initial empiric regimen that includes coverage for methicillin-sensitive S. aureus and gram negatives (e.g., piperacillin/tazobactam, cefepime, imipenem, meropenem, ceftolozane/tazobactam). Additional consideration for antibiotics is based on MDR risk factors that include use of IV antibiotics within 90 days, septic shock at the time of VAP, ARDS preceding VAP, at least five days of hospitalisation in the past 90 days, and requirement of acute renal replacement therapy prior to VAP onset. Two anti-Pseudomonal agents from different classes are recommended for VAP patients with at least one risk factor for resistant organisms and where the local prevalence of gram-negative resistance to a single anti-pseudomonal agent is not known or is >10% of gram-negative isolates (Kalil et al. 2016). Empiric therapy includes an aminoglycoside or an anti-Pseudomonal quinolone (high-dose ciprofloxacin or levofloxacin) and an anti-pseudomonal β-lactam such as cefepime, ceftazidime, ceftolozane/tazobactam, imipenem, meropenem, ceftazidime/avibactam, imipenem/relebactam, or piperacillin/tazobactam. Newer combination antibiotics are effective with MDR pathogens. Ceftazidime-avibactam and ceftolozane-tazobactam are effective against most MDR gram-negatives (Torres et al. 2018; Kollef et al. 2019; Torres et al. 2019). Meropenem-vaborbactam has good activity against most gram-negative microorganisms, including those with extended-spectrum beta-lactamases and K. pneumoniae carbapenemases and carbapenem-resistant Enterobacteriaceae (Wunderink et al. 2018). Imipenem-relebactam is effective against most gram-negative microorganisms with a survival advantage in VAP patients (Titov et al. 2020). MRSA coverage should be included with at least one of these risk factors for antimicrobial resistance and where local prevalence of MRSA is not known, or is >10-20% of S. aureus isolates. In those patients a third agent is added using either linezolid or vancomycin.
After culture results become available and with clinical stability, de-escalation to a more narrow spectrum agent, reducing the number of antibiotics, stopping therapy altogether in patients not likely to have infection, and making efforts to reduce duration of therapy is recommended, and this has been shown to improve mortality and reduce the chance of secondary infection and antimicrobial resistance (Niederman 2006). The majority of VAP patients can be treated with a short course of antibiotics up to eight days (Chastre et al. 2003). In patients with non-responding pneumonia, inhaled colistin or aminoglycosides in addition to IV antibiotics can be used as an adjunct treatment with documented success (Kalil et al. 2016). HAP treatment guidelines are the same as for VAP, with the exception that MDR risk factors in HAP are prior intravenous antibiotic use within 90 days, or high risk for mortality.
Patients with complicated intra-abdominal infection with sepsis and shock can be challenging since most infections are polymicrobial, with both aerobic and anaerobic pathogens. Empirical therapy should include gram-negative with additional anaerobic coverage, using a beta-lactam/beta-lactamase inhibitor combination or a carbapenem (Martin-Loeches et al. 2019). However, Enterococcus is a common pathogen in abdominal infections and is sometimes resistant to beta-lactams. In those patients, treatment is modified to include glycopeptides, oxazolidinones or carbapenems. Another consideration in ICU patients with complicated intra-abdominal infection is fungal infection with candidiasis and empirical antifungal therapy with azoles or echinocandins is generally initiated for severely ill patients (Martin-Loeches et al. 2019). Appropriate source control with percutaneous drainage or open drainage should not be delayed.
Conclusion
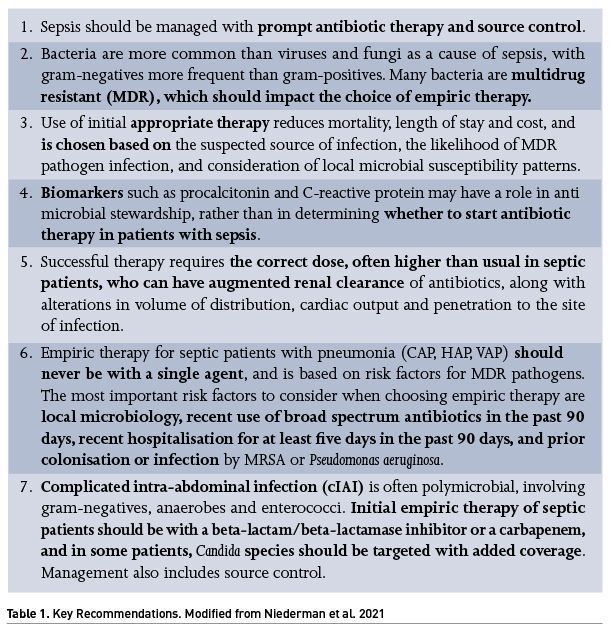
Sepsis is a common, heterogeneous, and life-threatening condition. Successful treatment includes identification of high-risk patients and prompt use of empiric antimicrobial agents directed towards the likely site of infection and the common pathogens, with a clear understanding of underlying risk factors for MDR pathogens. This should be followed by a timely de-escalation strategy once further culture data and clinical stability are achieved, to promote responsible antimicrobial stewardship. Further advances in rapid diagnostics and -omics technology will likely usher a personalised treatment option for sepsis based on endo/phenotypes. Key management principles are summarised in Table 1.
Conflict of Interest
None.
References:
Alrawashdeh M, Klompas M et al. (2022) Prevalence and Outcomes of Previously Healthy Adults Among Patients Hospitalized with Community-Onset Sepsis. Chest.
Baghela A, Pena OM et al. (2022) Predicting sepsis severity at first clinical presentation: The role of endotypes and mechanistic signatures. eBioMedicine. 75:103776.
Bassetti M, Rello J et al. (2020) Systematic review of the impact of appropriate versus inappropriate initial antibiotic therapy on outcomes of patients with severe bacterial infections. Int J Antimicrob Agents. 56(6):106184.
Blauwkamp TA, Thair S et al. (2019) Analytical and clinical validation of a microbial cell-free DNA sequencing test for infectious disease. Nat Microbiol. 4(4):663-674.
Bouadma L, Luyt CE et al. (2010) Use of procalcitonin to reduce patients' exposure to antibiotics in intensive care units (PRORATA trial): a multicentre randomised controlled trial. Lancet. 375(9713):463-474.
Buchman TG, Simpson SQ et al. (2020) Sepsis Among Medicare Beneficiaries: 1. The Burdens of Sepsis, 2012-2018. Crit Care Med. 48(3):276-288.
Chastre J, Wolff M et al. (2003) Comparison of 8 vs 15 days of antibiotic therapy for ventilator-associated pneumonia in adults: a randomized trial. JAMA. 290(19):2588-2598.
Cilloniz C, Dominedo D et al. (2019) Ceftobiprole for the treatment of pneumonia. Rev Esp Quimioter. 32 Suppl 3:17-23.
De Angelis G, Grossi A et al. (2020) Rapid molecular tests for detection of antimicrobial resistance determinants in Gram-negative organisms from positive blood cultures: a systematic review and meta-analysis. Clin Microbiol Infect. 26(3):271-280.
De Backer D, Cecconi M et al. (2019) Challenges in the management of septic shock: a narrative review. Intensive Care Med. 45(4):420-433.
Evans L, Rhodes A et al. (2021) Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 47(11):1181-1247.
Fay K, Sapiano MRP et al. (2020) Assessment of Health Care Exposures and Outcomes in Adult Patients With Sepsis and Septic Shock. JAMA Netw Open. 3(7):e206004.
Gunsolus IL, Sweeney TE et al. (2019) Diagnosing and Managing Sepsis by Probing the Host Response to Infection: Advances, Opportunities, and Challenges. J Clin Microbiol. 57(7).
Gupta S, Sakhuja A et al. (2016) Culture-Negative Severe Sepsis: Nationwide Trends and Outcomes. Chest. 150(6):1251-1259.
Kadri SS, Lai YL et al. (2021) Inappropriate empirical antibiotic therapy for bloodstream infections based on discordant in-vitro susceptibilities: a retrospective cohort analysis of prevalence, predictors, and mortality risk in US hospitals. Lancet Infect Dis. 21(2):241-251.
Kalil AC, Metersky ML et al. (2016) Executive Summary: Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 63(5):575-582.
Kollef MH, Novacek M et al. (2019) Ceftolozane-tazobactam versus meropenem for treatment of nosocomial pneumonia (ASPECT-NP): a randomised, controlled, double-blind, phase 3, non-inferiority trial. Lancet Infect Dis. 19(12):1299-1311.
Kruger S, Ewig S et al. (2008) Procalcitonin predicts patients at low risk of death from community-acquired pneumonia across all CRB-65 classes. Eur Respir J. 31(2):349-355.
Kumar A, Roberts D et al. (2006) Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 34(6):1589-1596.
Mandell LA, Wunderink RG et al. (2007) Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 44 Suppl 2:S27-72.
Martin-Loeches I, Antonelli M et al. (2019) ESICM/ESCMID task force on practical management of invasive candidiasis in critically ill patients. Intensive Care Med. 45(6):789-805.
Martin-Loeches I, Timsit JF et al. (2019) Clinical controversies in abdominal sepsis. Insights for critical care settings. J Crit Care. 53:53-58.
Masia M, Gutierrez F et al. (2005) Usefulness of procalcitonin levels in community-acquired pneumonia according to the patients outcome research team pneumonia severity index. Chest. 128(4):2223-2229.
Maslove DM, Shapira T et al. (2019) Validation of diagnostic gene sets to identify critically ill patients with sepsis. J Crit Care. 49: 92-98.
Metlay JP, Waterer GW et al. (2019) Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 200(7):e45-e67.
Miller RR, Lopansri BK et al. (2018). Validation of a Host Response Assay, SeptiCyte LAB, for Discriminating Sepsis from Systemic Inflammatory Response Syndrome in the ICU. Am J Respir Crit Care Med. 198(7):903-913.
Niederman MS, Baron RM et al. (2021) Initial antimicrobial management of sepsis. Crit Care. 25, 307.
Niederman, MS (2006) The importance of de-escalating antimicrobial therapy in patients with ventilator-associated pneumonia. Semin Respir Crit Care. Med 27(1):45-50.
Paoli CJ, Reynolds MA et al. (2018) Epidemiology and Costs of Sepsis in the United States-An Analysis Based on Timing of Diagnosis and Severity Level. Crit Care Med. 46(12):1889-1897.
Peters-Sengers H, Butler JM et al. (2022) Source-specific host response and outcomes in critically ill patients with sepsis: a prospective cohort study. Intensive Care Med. 48(1):92-102.
Rhee C, Wang R et al. (2019) Epidemiology of Hospital-Onset Versus Community-Onset Sepsis in U.S. Hospitals and Association With Mortality: A Retrospective Analysis Using Electronic Clinical Data. Crit Care Med. 47(9):1169-1176.
Rhodes A, Evans LE et al. (2017) Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Crit Care Med. 45(3):486-552.
Rodriguez A, Mendia A et al. (2007) Combination antibiotic therapy improves survival in patients with community-acquired pneumonia and shock. Crit Care Med. 35(6):1493-1498.
Seymour CW, Kennedy JN et al. (2019) Derivation, Validation, and Potential Treatment Implications of Novel Clinical Phenotypes for Sepsis. JAMA. 321(20):2003-2017.
She RC, Bender JM (2019) Advances in Rapid Molecular Blood Culture Diagnostics: Healthcare Impact, Laboratory Implications, and Multiplex Technologies. J Appl Lab Med. 3(4):617-630.
Sjovall F, Perner et al. (2017). Empirical mono- versus combination antibiotic therapy in adult intensive care patients with severe sepsis - A systematic review with meta-analysis and trial sequential analysis. J Infect. 74(4):331-344.
Sligl WI, Asadi L et al. (2014) Macrolides and mortality in critically ill patients with community-acquired pneumonia: a systematic review and meta-analysis. Crit Care Med. 42(2):420-432.
Sweeney TE, Wong HR et al. (2016) Robust classification of bacterial and viral infections via integrated host gene expression diagnostics. Sci Transl Med. 8(346):346ra391.
Tabah A, Bassetti M et al. (2020). Antimicrobial de-escalation in critically ill patients: a position statement from a task force of the European Society of Intensive Care Medicine (ESICM) and European Society of Clinical Microbiology and Infectious Diseases (ESCMID) Critically Ill Patients Study Group (ESGCIP). Intensive Care Med. 46(2):245-265.
Tamma PD, Aitken SL et al. (2020) Infectious Diseases Society of America Antimicrobial Resistant Treatment Guidance: Gram-Negative Bacterial Infections. Clin Infect Dis.
Taylor SP, Anderson WE et al. (2021) The Association Between Antibiotic Delay Intervals and Hospital Mortality Among Patients Treated in the Emergency Department for Suspected Sepsis. Crit Care Med. 49(5):741-747.
Teshome BF, Vouri SM et al. (2020) Evaluation of a ceiling effect on the association of new resistance development to antipseudomonal beta-lactam exposure in the critically ill. Infect Control Hosp Epidemiol. 41(4):484-485.
Timsit JF, Bassetti M et al. (2019) Rationalizing antimicrobial therapy in the ICU: a narrative review. Intensive Care Med 45(2):172-189.
Timsit JF, Ruppe E et al. (2020) Bloodstream infections in critically ill patients: an expert statement. Intensive Care Med. 46(2):266-284.
Titov I, Wunderink RG et al. (2020) A Randomized, Double-blind, Multicenter Trial Comparing Efficacy and Safety of Imipenem/Cilastatin/Relebactam Versus Piperacillin/Tazobactam in Adults With Hospital-acquired or Ventilator-associated Bacterial Pneumonia (RESTORE-IMI 2 Study). Clin Infect Dis.
Torres A, Rank D et al. (2019) Randomized Trial of Ceftazidime-Avibactam vs Meropenem for Treatment of Hospital-Acquired and Ventilator-Associated Bacterial Pneumonia (REPROVE): Analyses per US FDA-Specified End Points. Open Forum Infect Dis 6(4):ofz149.
Torres A, Zhong N et al. (2018) Ceftazidime-avibactam versus meropenem in nosocomial pneumonia, including ventilator-associated pneumonia (REPROVE): a randomised, double-blind, phase 3 non-inferiority trial. Lancet Infect Dis. 18(3):285-295.
Vardakas KZ, Trigkidis KK et al. (2017). Fluoroquinolones or macrolides in combination with beta-lactams in adult patients hospitalized with community acquired pneumonia: a systematic review and meta-analysis. Clin Microbiol Infect 23(4): 234-241.
Vincent JL, Sakr Y et al. (2020) Prevalence and Outcomes of Infection Among Patients in Intensive Care Units in 2017. JAMA. 323(15):1478-1487.
Wirz Y, Meier MA et al. (2018) Effect of procalcitonin-guided antibiotic treatment on clinical outcomes in intensive care unit patients with infection and sepsis patients: a patient-level meta-analysis of randomized trials. Crit Care. 22(1):191.
Wunderink RG, Giamarellos-Bourboulis EJ et al. (2018) Effect and Safety of Meropenem-Vaborbactam versus Best-Available Therapy in Patients with Carbapenem-Resistant Enterobacteriaceae Infections: The TANGO II Randomized Clinical Trial. Infect Dis Ther. 7(4):439-455.
Wunderink RG, Srinivasan A et al. (2020). Antibiotic Stewardship in the Intensive Care Unit. An Official American Thoracic Society Workshop Report in Collaboration with the AACN, CHEST, CDC, and SCCM. Ann Am Thorac Soc. 17(5):531-540.
Zacharioudakis IM, Zervou FN et al. (2019) Cost-effectiveness of molecular diagnostic assays for the therapy of severe sepsis and septic shock in the emergency department. PLoS One.14(5):e0217508.








