Sepsis is defined as a “life-threatening organ dysfunction caused by a dysregulated host response to infection” (Singer et al. 2016) and is estimated by the UK Sepsis Trust to cause the deaths of at least 44,000 people in the UK annually.
Scaling the findings of a large meta-analysis (Fleischmann et al. 2016) for relative population size gives an incidence in Wales of between 8000-13,000 cases of sepsis per annum with an associated mortality of between 2200-2300.
These estimates accord with both extrapolation from an inspection of UK critical care data (Daniels 2011a) and a retrospective review of mortality within one Welsh hospital (Robinson 2013). The latter study estimated sepsis to be responsible for approximately 15% of hospital deaths.
The size of sepsis in Wales study (Szakmany et al. 2016) found a prevalence of sepsis and severe sepsis in Welsh acute hospitals of 5.5% with associated mortality at 90 days of 31%.
In NHS Wales the aim to reduce avoidable harm and mortality caused by sepsis has been a tier one Welsh Government target since 2013, and all Health Boards and Trusts have participated in the national Rapid Response to Acute Illness (RRAILS) programme since 2011.
During the time that this programme has enabled clinicians to identify and treat sepsis more quickly there has been a reduction in the numbers of deaths associated with two sepsis ICD10 codes. NHS Wales was the winner of a Global Sepsis Award in 2015 (Hancock and Watkins 2017).
An important component in this achievement has been enabling clinicians to rapidly recognise sepsis and treat using the ‘Sepsis 6’ care bundle.
The Sepsis 6 bundle
The original Surviving Sepsis Campaign Guidelines (Dellinger 2008) and subsequent revisions have focused on the delivery of evidence-based, time-limited ‘care bundles’ at various points in the patient pathway, including within 1-, 3-, 6- and 24-hour time frames.
UK healthcare has generally chosen to adopt the ‘Sepsis 6’ care bundle, which was first devised by Ron Daniels of the UK Sepsis Trust and the delivery of which, within a one-hour timeframe, has been shown to be associated with improved patient outcomes (Daniels et al. 2011b; NCEPOD 2015)
The six elements of the bundle are:
- Give O2 to keep sats above 94%
- Take blood cultures
- Give IV antibiotics
- Give a fluid challenge
- Measure lactate
- Measure urine output
In NHS Wales the Sepsis 6 bundle, delivered within one hour of sepsis recognition, has been the accepted and standard treatment for sepsis in all acute hospital settings since 2013. Percentage compliance with delivery of the bundle is measured within all Health Boards as a key quality improvement metric.
An important function of the RRAILS programme has been to support clinicians in testing various methods for increasing the speed and effectiveness of Sepsis 6 bundle delivery. These have included the sepsis bag, sepsis box and sepsis trolley.
Description and evaluation of such tools is not well developed in the literature. One large-scale literature review of the crash cart /resuscitation trolley reported little information or uniformity in the range of equipment, instructions for use or evaluation of effectiveness (Jacquet et al 2018).
Kafle and Nath (2014) report improvements in outcomes for patients treated with a range of sepsis interventions including a sepsis box but in the context of a small sample size (n=30).
The sepsis bag
Working with 1000 Lives Improvement Service, the Critical Care Outreach Team (CCOT) at the Royal Glamorgan Hospital, Cwm Taf University Health Board, introduced a sepsis response bag in 2012. The bag contained the six elements of the Sepsis 6 care bundle with the exception of antibiotics.
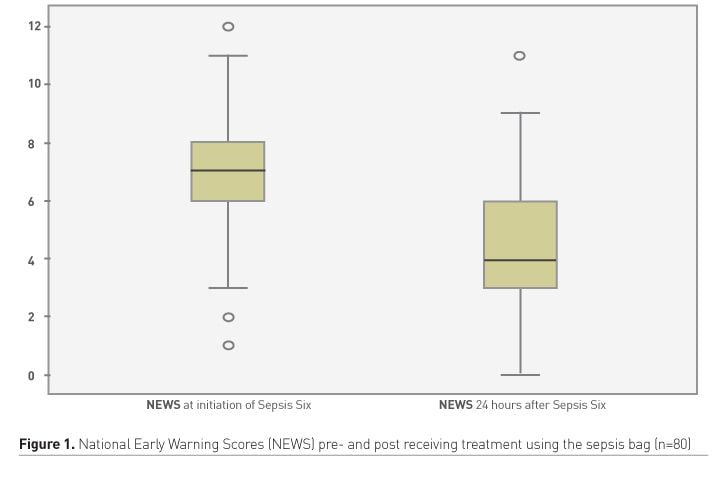
The bag was evaluated by analysis of the National Early Warning Scores (NEWS) of eighty patients pre- and post receiving treatment using the bag. This analysis showed a statistically significant reduction of NEWS at 24 hours of treatment using the sepsis bag with the largest reduction being -8 (Figure 1).
The sepsis response bags were found to be favourably associated with the delivery of the Sepsis 6 and the reduction in NEWS was accepted as inferring a better patient outcome.
However, evaluation of the sepsis bags highlighted several difficulties:
- Infection prevention and control advice in the Welsh Government was that the bags would be impossible to clean effectively between patients.
- The bags were not sealed and equipment could be and was removed. This obviously had serious implications for completeness of the kit when the bag came to be used again.
- Once the bag had been used it was difficult to get it replenished immediately.
- The majority of the bags had been used by the CCOT and not by medical or nursing staff in the ward areas, potentially resulting in a delay in delivery of the Sepsis 6 bundle.
In order to address these issues whilst maintaining the concept of the single adjunct for delivery of treatment the 1000 Lives Improvement Service and Cwm Taf University Health Board approached an industry partner to collaborate in developing and testing a solution.
The sepsis box study
The disposable single-use box that was collaboratively developed as a result contained all the elements to deliver the Sepsis 6 apart from antibiotics. Each element was contained within a separate, sealed compartment with a perforated cardboard ‘door’ modelled on the idea of the advent calendar.
The box also contained all the documentation necessary for recording delivery of the Sepsis 6 bundle as well as a copy of the Health Board antibiotic formulary.
The study took place between May 2016 and April 2017 with a box being placed in all clinical areas, excluding the intensive care unit (ICU) and emergency department (ED), at two district general hospitals within Cwm Taf University Health Board. As boxes were used they were replaced by the Critical Care Outreach Team who also performed the role of data collectors. A data entry clerk transferred data to a purpose-built database and the results were analysed by both the 1000 Lives Improvement Service and Cwm Taf University Health Board.
In addition to the outcomes associated with use of the sepsis bag this study also had the aims to:
- Improve Sepsis 6 bundle compliance
- Engage ward staff to initiate the Sepsis 6 care bundle
- Prevent admissions to critical care.
A staff survey was carried out concurrently to evaluate attitudes to use of the sepsis box.
Results
Data was recorded for 114 patients who had been treated using the sepsis box. Members of the Critical Care Outreach Team (CCOT), partly due to an issue with the distribution of blood culture bottles to wards during the trial period, initiated the majority of boxes.
The staff survey revealed that the single-use sepsis box was generally positively regarded and was favourably associated with the delivery of the Sepsis 6 care bundle by ward staff.
Outcomes
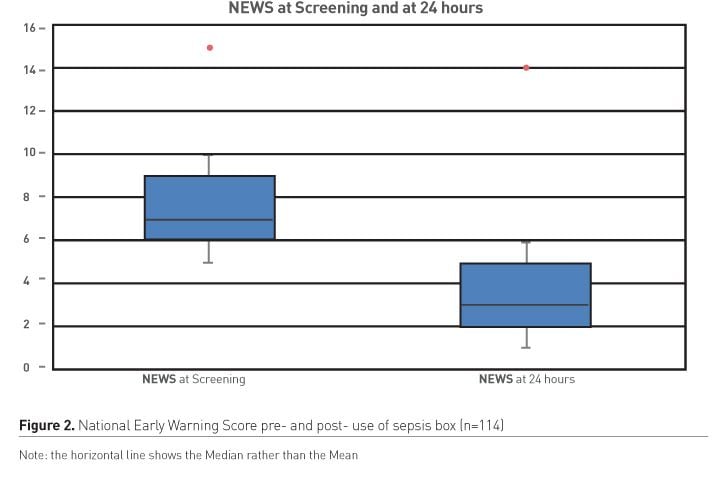
Quantitatively, positive patient outcomes were associated with use of the single-use sepsis box. The results from the trial indicated a significant drop in average NEWS score at 24 hours and an inferred better patient outcome from use of the box (Figure 2). Of the 114 patients, the mean NEWS score at the point of Sepsis recognition was 7.66 indicating a high acuity and a strong mortality prediction whilst the mean NEWS score at 24 hours post treatment was 3.89.
Of the 114 patients who received treatment in total with the box, at 24 hours:
- 10 (9%) patients were admitted to Critical Care, of which
- 1 (1%) patient died
- 104 (91%) remained on the ward and improved.
Use of the box by ward nursing staff
During the trial, ward staff rather than the CCOT initiated treatment using the sepsis box on 28 (25%) occasions and of these 1 patient was transferred to critical care with a NEWS of 12, and survived. Of these 28 patients treated:
- 1 patient had a NEWS of 12
- 2 patients had a NEWS of 11; and
- 25 patients had a NEWS of 9.
Discussion
The trial showed that initiation of the Sepsis 6 care bundle through use of the single-use Sepsis Box was linked to a significant drop in average NEWS at 24 hours, and with significantly fewer patients being referred to critical care than would normally be expected with such high NEWS scores.
The 25% of patients whose treatment was initiated by ward nursing staff were all very sick with a NEWS of 9 or greater, which would ordinarily be associated with an admission to critical care. Only one of these patients was admitted to critical care and survived.
As the trial was not randomised, compared to a control group, and had a small sample size, it is not possible to infer whether the positive outcomes are directly attributable to the unique features of the single use sepsis box, or are simply associated with the utilisation of any tool that drives the delivery of sepsis treatment in the clinical area.
If the latter then it is possible that the use of a bag, box or trolley influences a number of factors including reliability, error proofing, decision support and ‘nudging’ behavioural change.
Reliability
Reliability of healthcare delivery is poor. McGlynn et al. (2003) found the ‘defect rate’ in the delivery of healthcare to be 45% whilst Burnett et al. (2012) demonstrated reliability of care delivery at 80-90%, noting that these rates would not be tolerated by any other industry.
In promoting the idea of ‘Safety 2’ Hollnagel et al (2015) state that:
“Safety management should .... move from ensuring that ‘as few things as possible go wrong’ to ensuring that ‘as many things as possible go right’”
In seeking to ensure that as many things as possible do go right, in recent years clinicians have sought to learn lessons from other ‘safety critical’ high-reliability organisations (HROs) (Weick and Sutcliffe 2007; Health Foundation 2011).
An important lesson is how to mitigate for human error, by utilising a range of human factors principles, including ‘error proofing’ the system. Error proofing, or Poka Yoke as developed by the Toyota Production System, is intended to make it more difficult and to require more effort to do the ‘wrong’ thing and easier to do the correct action.
The sepsis box, containing all required items and instructions to perform the task, fulfils these criteria well. However, we should also be aware of the dangers of confirmation bias and potential for inappropriate overtreatment with unnecessary antibiotics in patients who do not have sepsis.
Decision support
The first consensus statement on medical emergency teams (METs) (Devita et al. 2006) identifies the afferent and efferent arms of the rapid response system. The afferent part consists of the recognition of acute deterioration and a trigger to action whilst the efferent part consists of the response, usually by a team or individual with critical care expertise.
This binary approach continues to be used to describe the rapid response system and is undoubtedly useful. However, it is possible that it may be too simple a model to use when describing the actions around the treatment of an acutely, although not critically ill person, such as some with sepsis.
The National Confidential Enquiry into Patient Outcome and Death (NCEPOD) report Time to Intervene (2012) identifies system failures not only in the recognition and response to the sick patient but also in the escalation process of their care. The UK Department of Health publication Competencies for Recognising and Responding to Acutely Ill Patients in Hospital (2009) identifies six possible roles in the recognition, escalation and response process, only the last of which necessitates the possession of critical care skills on the part of the responder.
The recent publication of a competency framework for caring for Level 1 patients (National Outreach Forum and Critical Care Networks 2018) is an acknowledgement of the fact that the hospital does not contain only the relatively well and those in need of a critical care response but that the landscape of patient acuity is more nuanced.
In short, it is apparent that there is a considerable amount of decision-making taking place between the points of recognition and response to sepsis and that this process involves achieving reliable communication of a shared mental model and establishing situational awareness amongst teams of nursing and medical staff in the acute setting.
It was evident during the study that the use of the sepsis box, alongside a standardised care bundle and screening tool, enhanced decision-making and promoted escalation of care to appropriate levels. This can be seen from the large number of patients with a NEWS that would normally indicate an ICU admission, remaining on the ward with a lower NEWS at 24 hours.
Behavioural change
The Health Foundation paper Behavioural Insights in Healthcare (Perry et al. 2015) identifies the provision of prompts and cues as well as using default options such as care bundles, as important tools in delivering behaviour change. The Behavioural Insights team (BIT) (Service et al. 2014) identify the acronym EAST™ (Easy Attractive, Social and Timely) as descriptive of successful behavioural change. The use of a focused prompt such as the sepsis box or trolley within the context of a rapid response system satisfies the requirements for an easy, attractive, social and timely approach to behaviour change.
Conclusion
Whilst limited in both sample size and evaluative rigour this study does, nevertheless, appear to indicate that the use of a piece of equipment to focus delivery of sepsis treatment can have positive outcomes for patients for a number of reasons. These may include design, effect on improving reliability, error proofing of the system, supporting decision-making in the sub-critical patient and in nudging a change in clinical behaviour.
Since the completion of the sepsis box study, the decision has been made by the commercial company on economic grounds, to cease production. Whilst this is disappointing it is nevertheless worth noting that a by-product of the trial and the interest shown in it is that all hospitals in Wales now aspire to situate a sepsis bag, box or trolley in all clinical areas.
Acknowledgements
We would like to acknowledge the hard work, ingenuity and perseverance of Anne Evans and her colleagues at Rocialle and the dedication of the CCOT teams and clinicians in Cwm Taf University Health Board.
Conflict of interest
Chris Hancock declares that he has no conflict of interest. Andrew Hermon declares that he has no conflict of interest.