ICU Management & Practice, Volume 23 - Issue 4, 2023
Mechanical power is an easy bedside tool to guide lung protective ventilation, as it is an index of the energy load applied to the lung during mechanical ventilation and expresses in one formula all the main determinants of ventilator-induced lung injury. Although a threshold value has not already been defined, a mechanical power greater than 17 J/min has been demonstrated to be associated with the risk of death.
Approximately 35% of critically ill patients admitted to an intensive care unit required mechanical ventilation (Bellani et al. 2016). Irrespective of the underlying disease, mechanical ventilation is instituted to ensure adequate gas exchange and reduce the work of breathing and ventilator-induced lung injury (VILI) (Fan et al. 2018).
According to the motion equation, the pressure developed inside the respiratory system is used to generate an inspiratory flow and a change in tidal volume (Gattinoni et al. 2016). For a given flow and tidal volume, the generated airway pressure into the respiratory system can be different according to the elastic and resistive load of the lungs and chest wall. In passive conditions, the possible development of lung injury during mechanical ventilation thus arises from the interaction between the ventilator and the characteristics of the respiratory system.
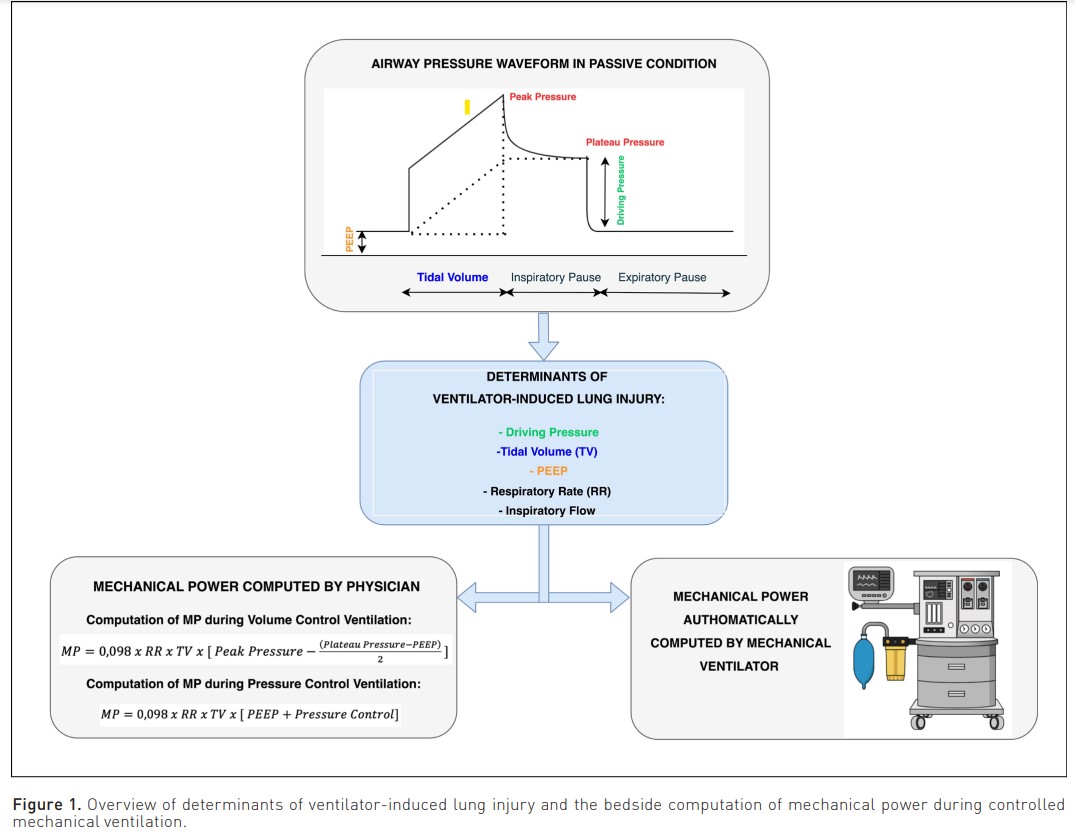
In daily clinical practice, the tidal volume and the driving pressure are usually considered the main determinants of the VILI, although the respiratory rate and the level of positive end-expiratory pressure (PEEP) could also play a role, albeit to a lesser extent (Fan et al. 2017; Sahetya et al. 2017).
In order to unify all these variables, in 2016 our group proposed mechanical power as an index of the energy load applied during mechanical ventilation, which could be related to the risk of the VILI (Cressoni et al. 2016; Gattinoni et al. 2016). Initially, it was computed including tidal volume, respiratory rate, compliance, resistance and inspiratory flow in the formula. Subsequently, a more simplified formula based only on the inspiratory plateau pressure, applied PEEP, and tidal volume has been proposed (Chiumello et al. 2020; Giosa et al. 2019). However, this more simplified formula can be used only during volume control ventilation with a constant inspiratory flow (Gattinoni et al. 2016). On the contrary, during pressure control ventilation, in which the flow is decelerated, another specific algebraic formula should be applied (Chiumello et al. 2020). Both these surrogate algebraic formulae (i.e. for volume and pressure control ventilation), based on variables commonly provided by the mechanical ventilator (Chiumello et al. 2020), showed an acceptable accuracy compared to the more sophisticated comprehensive formula.
Furthermore, the new generation of mechanical ventilators can both continuously and automatically show mechanical power at the bedside with good accuracy (Chiumello et al. 2022) (Figure 1).
A post hoc analysis of a large randomised clinical trial comparing the application of a low versus a high tidal volume (6 ml/kg vs 10 ml/kg of predicted body weight) in healthy patients during general anaesthesia for major surgery, demonstrated that the mechanical power was associated with an increased risk of postoperative pulmonary complications and acute respiratory failure [OR, 1.34 (95% CI, 1.17 to 1.52), P <0.001; OR, 1.40 (95% CI, 1.21 to 1.61), P <0.001] in the first seven postoperative days (Karalapillai et al. 2022). A subsequent retrospective cohort study which analysed data of patients who underwent general anaesthesia between 2008 and 2018, found that the median intraoperative mechanical power was higher in patients with postoperative respiratory failure than in patients without (7.67 vs 6.62 J/min; P <0.001) (Santer et al. 2022). In particular, a higher mechanical power was associated with a greater risk of postoperative reintubation: for each 5 J/min increase in mechanical power, the adjusted risk of reintubation was 31% higher (Santer et al. 2022).
In critically ill mechanically ventilated patients admitted to the emergency department without acute respiratory distress syndrome (ARDS), 8.9% developed ARDS during the intensive care stay (Fuller et al. 2018). Compared to patients without ARDS, those who developed ARDS presented a significantly higher mechanical power at admission (17.5 vs 15.7 J/min, respectively). Interestingly, the incidence of ARDS was significantly higher for mechanical power values greater than 12 J/min.
Analysing critically ill patients admitted to intensive care who were mechanically ventilated for at least 48 hours, the mechanical power after the first 24 hours of ventilation was significantly associated with higher intensive care and 30-day mortality (Serpa Neto et al. 2018). There was a consistent increase in the risk of death for mechanical power values greater than 17 J/min, and these mechanical power values remained associated with higher mortality even in the presence of low tidal volume or driving pressure.
Considering patients with sustained ARDS, mechanical power values greater than 22 J/min were associated with higher hospital mortality and lower survival at three years (Parhar et al. 2019).
However, a similar mechanical power could result in different degrees of possible lung injury according to the lung and chest wall elastance characteristics. The real distending force of the lung is not the airway pressure but the transpulmonary, computed as the difference between the airway and pleural pressure (i.e. commonly as the oesophageal pressure); consequently, especially in the presence of chest wall impairment, the transpulmonary mechanical power should better reflect the possible lung injury. In addition, ARDS patients are characterised by a huge variability in the lung size (i.e. baby lung), which mainly depends on the severity of respiratory failure. In fact, the possible lung injury could also be related to the amount of aerated tissue and size of the baby lung: a less injured lung could tolerate a higher mechanical power compared to a sicker lung. In other words, a similar mechanical power could be more harmful in severe ARDS compared to moderate ARDS. When the mechanical power was normalised to the aerated lung, it was associated with intensive care mortality (Coppola et al. 2020). In addition, among the different ventilator parameters such as tidal volume, respiratory rate, PEEP, and driving pressure, the mechanical power normalised to compliance had the highest predictive discrimination for the patient outcome (Zhang et al. 2019).
At the present time, according to the available data and based on the pathophysiology of the VILI, the mechanical power, which can be easily computed by physicians at the bedside or displayed in the modern ventilators, should be included in the daily clinical monitoring as an easy tool to guide a lung protective strategy.
Conflict of Interest
None.









