ICU Management & Practice, Volume 24 - Issue 4, 2024
Early mobilisation in critical care significantly improves outcomes in critically ill patients. Overcoming boundaries requires a proactive approach, training, research and multidisciplinary collaboration.
Introduction
Early mobilisation in the critically ill patient is essential to mitigate the adverse consequences of bed rest and improve outcomes and cost reduction. The absence of muscle contraction results in loss of muscle strength and mass, leading to reduced muscle cross-sectional area, increased production of pro-inflammatory cytokines, proteolysis and muscle catabolism, leading to the development of more complications resulting in more days on mechanical ventilation, more difficult weaning, prolonged ICU stays or hospital days and even increased morbidity and mortality rates. This review provides evidence-based statements about the benefit of early mobilisation in critical care, which is a mainstay in intensive care units.
Importance for the Critically Ill Patient
One of the main problems in intensive care units where there are patients with limited mobility as a result of their underlying pathology, their clinical condition, or as a direct consequence of the necessary treatments, such as the requirement for invasive mechanical ventilation, deep sedation, malnutrition or the use of neuromuscular blockers, involves the risk of developing ICU-acquired weakness; a condition characterised by a decrease in muscle strength, generally associated with atrophy, of acute, diffuse, symmetrical and generalised onset, which develops after the onset of critical illness (Diaz et al. 2017).
Weakness acquired in the ICU does not only affect the muscles of the extremities; on the contrary, atrophy can even affect the diaphragmatic musculature after 18 hours from the start of mechanical ventilation and 96 hours in the skeletal muscles of the extremities, so that the longer the days of ventilation, the greater the muscular and systemic damage (Diaz et al. 2017).
The participation of professionals from various branches of healthcare (medicine, nursing, physiotherapy, respiratory therapy, among others) in the assessment of the patient and consensus decision-making regarding their clinical condition allows a wide range of perspectives to be considered in their management and guarantees that the decisions taken lead to the patient's recovery due to their holistic nature and are backed by an informed consensus based on scientific evidence (Hiser et al. 2023).
Benefits and Barriers in the ICU
The catabolic state during critical illness causes a change in the role of muscle. Per day in the intensive care unit (ICU), there is a 2% loss of muscle mass, and during the first week of hospital stay, there is a 12.5 % loss of muscle cross-sectional area in the presence of mechanical ventilation. The lower limbs, particularly the hip flexors, are susceptible to atrophy (Hiser et al. 2023):
Benefits of early rehabilitation
- Improvement in the level of mobility.
- Preservation of muscle mass.
- Decreased incidence of delirium.
- Reduction of intensive care stay.
- Reduction of days of mechanical ventilation.
- Reduction of morbidity and mortality.
A study in New Zealand found that only 8% of mechanically ventilated patients were mobilised out of bed (Grimm 2019). ICU patients undergo a significant percentage of deep sedation and mechanical ventilation, and haemodynamic support, and therefore, these patients experience reduced mobility and the long-term functional impairment for ICU survivors is mainly characterised by cognitive and motor sequelae (Cuthbertson et al. 2010).

In a survey conducted in intensive care units in Jundishapur of Ahvas, it was found that the main barrier to mobilisation of ICU patients was lack of trained staff, inadequate time for this procedure, as well as deep sedation/coma, obese patients and patients with agitated pain as main patient-related barriers (Babazadeh et al. 2021).
There is a lack of standardised protocol for early mobilisation, including adequate record keeping and a checklist. Inadequate equipment for the mobilisation of mechanically ventilated patients is a limitation present in intensive care units.
A survey of ICU physicians conducted in Brazil aimed to identify attitudes and barriers to the implementation of early mobilisation of critically ill patients; availability of professionals, time to mobilise and excessive stress due to workload were the main findings (Fontela et al. 2018).
In a Canadian study conducted in 46 intensive care units, 60% of physicians stated that they did not have sufficient knowledge or skills to mobilise patients receiving multi-organ support (Koo et al. 2016).
A study in India describes a lack of protocols for patient mobilisation (Akhtar and Deshmukh 2021), similar to that described in developing countries, and sufficient equipment is a limitation (Koo et al. 2016).
Obesity becomes a major challenge in early mobilisation, adding the requirement for extracorporeal supports; they participate in a misconception of seeking lack of mobility to avoid accidental removal of endotracheal tube or vascular access or drains, thereby delaying the window of opportunity to decrease the presence of acquired weakness of the critically ill patient (Bakhru et al. 2015).
‘Early rehabilitation in critical areas could improve functional prognosis and hospital costs; persistence of heterogeneous and unsubstantiated behaviours delays progress’.
Implementation Strategies
Mobilisation of the critically ill has become an increasingly important area of interest in recent years. Although most of the literature comes from neurosciences, nursing care, paediatrics, orthopaedics and geriatrics, it is of increasing interest to rehabilitation professionals (Zang et al. 2020).
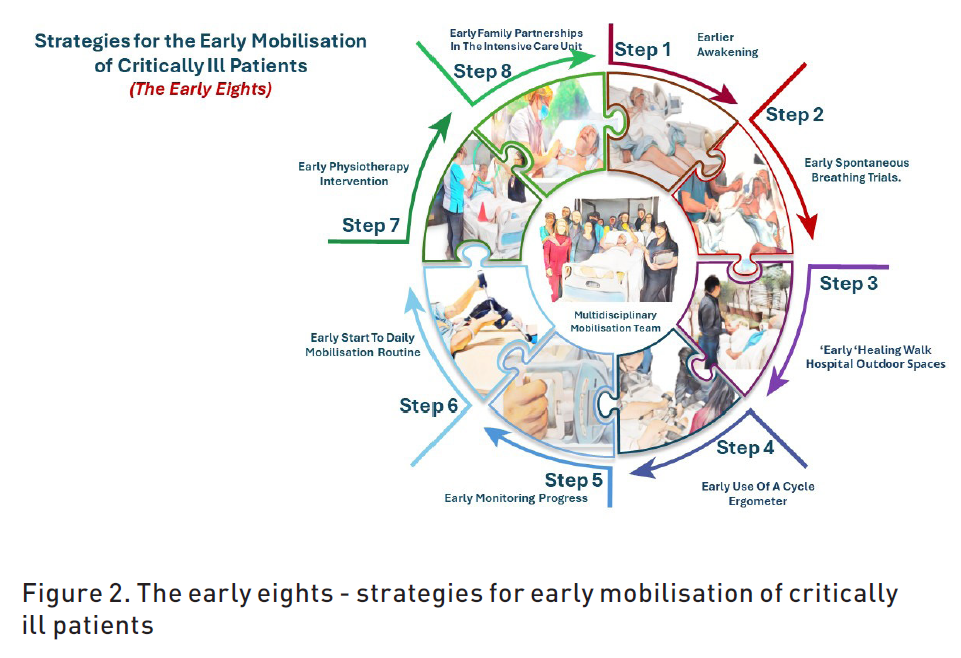
Efforts to reduce the use of sedatives and to promote early daily patient awakening and spontaneous breathing ventilation methods have become focal points of care in critical areas. This multi-centre approach to interventions that reduce ‘treatment-related immobilisation’, combined with a focus on patient management immediately after acute illness, may also improve the overall likelihood and safety of patient mobilisation after prolonged or unwarranted sedative use (Alaparthi et al. 2020; Menges et al. 2021).
The administration of unwarranted deep sedation in a human being is a practice that should be severely penalised. This intervention, lacking adequate clinical justification, not only carries inherent risks and adverse outcomes, but also entails high human and financial costs. Furthermore, it perpetuates a questionable medical tradition that compromises ethics and patient safety (Hodgson et al. 2022).
A multidisciplinary team is essential to promote early mobilisation of ICU patients. Team members set goals of care for each patient based on the patient's condition, the team's experience, and pending trials and guidelines if the patient is unable to communicate. The ICU environment and specific staff may affect how, when, where and by whom early ambulation/mobility can be initiated in individual patients (Lang et al. 2020; Smith et al. 2022).
Patient and family involvement, and support are critical to the development of a patient-centred critical illness recovery plan and the timely initiation of early mobilisation activities. Patients and their families should be educated about the implications of early mobilisation, expectations based on current condition, appreciation of their role in the early mobility process, provision of reassurance and creating a sense of achievement for the patient (Rawal and Bakhru 2023).
Early mobilisation of critically ill patients, while beneficial, remains underutilised due to concerns about patient safety and tolerance. Conflicting ethical issues may also arise, including respect for patient autonomy, beneficence to the patient, non-maleficence and justice. Dilemmas may arise because of advances in medical management, such as advances in critical care that help sustain life or modes of support that prevent the resolution of illness or disease and rehabilitation that patients may not want (Rawal and Bakhru 2023).
There is limited information on the economic consequences of implementing early mobilisation programmes. However, cost-effectiveness must be considered when allocating resources. From this perspective, it has been argued that early initiation of a progressive exercise and increased mobilisation may place substantial or excessive demands on staff, physical resources and time. Identifying the financial demand of a mobilisation programme and being able to reallocate sufficient resources after its implementation initiative is also vital for these programmes (Morris et al. 2008).
‘The prescription of unwarranted deep sedation in a human being should be criminalised, the result is an inhumane act’.
Impact on Clinical Outcomes
The outcomes of early mobilisation in critically ill patients are uncertain, although it has been associated with improved muscle strength by MRC scores and Barthel index (Schweickert et al. 2009), reduced incidence of delirium, return of baseline functional class (OR 2.7 CI 95%, 1.2-6. There is no conclusive information on survival and mortality benefits, as well as no precise definitions of early rehabilitation and no standardised algorithms for early mobilisation and rehabilitation in intensive care units.
A systematic review and meta-analysis comparing the outcomes of adult patients with early mobilisation under mechanical ventilation, defined as within three days of ICU admission, compared to the standard mobilisation group, showed no improvement in mortality at 180 days compared to the intervention group RR 1.09 CI 95% (0.69-1. 76) I2 0%, nor differences in secondary outcomes which were: days ICU stay RR -2.18 CI 95% (-3.27, -0.94) I2 93%, duration of mechanical ventilation RR -1.39 CI 95% (-2.50, -0.56) I2 82%, The analysis had severe limitations such as sample size, high heterogeneity of studies and a lack of consensus on the definition and protocols of early mobilisation (Wang et al. 2023). It is a priority to implement standardised protocols in our critical care units and to assess the risks involved in order to generate lines of research that will strengthen our clinical practice.
A comparative line of research on the effects of mobilisation 72 hours after admission to the intensive care unit followed up six months after hospital discharge, with inconclusive results on the primary outcomes of muscle strength, cognitive function, and adverse effects of early mobilisation RR 1.3 CI 95% (0.49-2.62) I2 47% (Matsukoa et al. 2023). No mortality benefit was observed in the intervention group RR 1.15 CI 95% (0.83-1.60) I2=0%. The results contrasted in lines of research by (Paton et al. 2022), where the probability of a higher survival rate in the early mobilisation group is observed. The lack of results against continuing strategies of early mobilisation protocols leaves a field of opportunity for new generations and intensive care teams that can add to the results observed in our unit in the southeast Mexican.

Conclusion
Active identification of early mobilisation barriers and implementation of a protocol should be part of the mandatory model of care for all intensive care units. Data supporting favourable outcomes of early mobilisation in intensive care unit patients is a growing line of research, and understanding the real short- and long-term impact on critically ill patients requires standardisation of rehabilitation protocols and unification of definitions of early rehabilitation.
Acknowledgement
The families involved in the process and the team that integrates the intensive care unit of ISSSTE Veracruz (nurses, physiotherapists, nutritionists, orderlies, doctors and residents) who make it possible to continue the implementation of evidence-based medicine for the good of our patients.
Conflict of Interest
None.
References:
Alaparthi GK, Gatty A, Samuel SR, Amaravadi SK (2020) Effectiveness, safety, and barriers to early mobilization in the intensive care unit. Critical Care Research and Practice. (1):7840743.
Babazadeh M, Jahani S, Poursangbor T, Cheraghian B (2021) Perceived barriers to early mobilization of intensive care unit patients by nurses in hospitals affiliated to Jundishapur University of Medical Sciences of Ahvaz in 2019. J Med Life. 14(1):100-104.
Bakhru RN, Wiebe DJ, McWilliams DJ et al. (2015) An environmental scan for early mobilization practices in US ICUs. Critical care medicine. 43(11):2360-9.
Cuthbertson BH, Roughton S, Jenkinson D et al. (2010) Quality of life in the five years after intensive care: a cohort study. Crit Care. 14:R6.
Diaz Ballve LP, Dargains N, Urrutia Inchaustegui JG et al. (2017) Weakness acquired in the intensive care unit. Incidence, risk factors and their association with inspiratory weakness. Observational cohort study. Rev Bras Ter Intensiva. 29(4):466-475.
Fontela PC, Forgiarini LA Jr, Friedman G (2018) Clinical attitudes and perceived barriers to early mobilization of critically ill patients in adult intensive care units. Rev Bras Ter Intensiva. 30(2):187-194.
Grimm J, Silvestri-Elmore A, Grimm E et al. (2019) Perceived barriers to early progressive mobilization in the ICU: Multidisciplinary perspectives in an underserved population. Journal of Nursing Education and Practice. 9(4):5.
Hiser SL, Fatima A, Ali M, Needham DM (2023) Post-intensive care syndrome (PICS): recent updates. J Intensive Care. 11(1):23.
Koo KK, Choong K, Cook DJ et al. (2016) Canadian Critical Care Trials Group. Early mobilization of critically ill adults: a survey of knowledge, perceptions and practices of Canadian physicians and physiotherapists. CMAJ Open. 4(3):E448-E454.
Lang JK, Paykel MS, Haines KJ, Hodgson CL (2020) Clinical Practice Guidelines for Early Mobilization in the ICU: A Systematic Review. Crit Care Med. 48(11):e1121-e1128.
Matsuoka A, Yoshihiro S, Shida H et al. (2023) Effects of Mobilization within 72 h of ICU Admission in Critically Ill Patients: An Updated Systematic Review and Meta-Analysis of Randomized Controlled Trials. J Clin Med. 12(18):5888.
Menges D, Seiler B, Tomonaga Y et al. (2021) Systematic early versus late mobilization or standard early mobilization in mechanically ventilated adult ICU patients: systematic review and meta-analysis. Critical Care. 25:1-24.
Morris PE, Goad A, Thompson C et al. (2008) Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 36(8):2238-43.
Patel BK, Wolfe KS, Patel SB et al. (2023) Effect of early mobilisation on long-term cognitive impairment in critical illness in the USA: a randomised controlled trial. Lancet Respir Med. 11(6):563-572.
Paton M, Chan S, Tipping CJ et al. (2023) The Effect of Mobilization at 6 Months after Critical Illness - Meta-Analysis. NEJM Evid. 2(2):EVIDoa2200234.
Rawal H, Bakhru RN (2024) Early mobilization in the ICU. CHEST Critical Care. 2(1): 100038.
Schweickert WD, Pohlman MC, Pohlman AS et al. (2009) Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 373(9678):1874-82.
Smith HAB, Besunder JB, Betters KA et al. (2022) 2022 Society of Critical Care Medicine Clinical Practice Guidelines on Prevention and Management of Pain, Agitation, Neuromuscular Blockade, and Delirium in Critically Ill Pediatric Patients With Consideration of the ICU Environment and Early Mobility. Pediatr Crit Care Med. 23(2):e74-e110.
TEAM Study Investigators and the ANZICS Clinical Trials Group; Hodgson CL, Bailey M et al. (2022) Early Active Mobilization during Mechanical Ventilation in the ICU. N Engl J Med. 387(19):1747-1758.
Wang L, Hua Y, Wang L et al. (2023) The effects of early mobilization in mechanically ventilated adult ICU patients: systematic review and meta-analysis. Front Med (Lausanne). 10:1202754.
Zang K, Chen B, Wang M et al. (2020) The effect of early mobilization in critically ill patients: a meta‐analysis. Nursing in critical care. 25(6):360-7.












