ICU Management & Practice, Volume 16 - Issue 3, 2016
Brazil is the largest country in South America, and ranks fifth in the list of the most populous countries, with a population of approximately 209 million people (84% urban). It is a large country with many challenges that affect the healthcare sector, such as economic inequalities, and the demographic transition with an ageing population (>10% older than 60%), the result of diminishing birth rates and an increased life expectancy of 74 years (World Health Organization 2015). Despite the existence of universal coverage, 25% of the population is covered by private insurance.
ICU Beds Capacity and Distribution
There are significant disparities when it comes to hospitals and intensive care unit (ICU) beds. Brazil has approximately 6400 hospitals, 69% of which are private. Only 35% of hospital beds are public, although the public sector also has access to a substantial number of private beds through contracts (Paim et al 2011; Cadastro Nacional de Estabelecimentos de Saude 2016; Instituto Brasileiro de Geografia e Estatística 2016).
There are approximately 36,000 ICU beds in Brazil. Although this is one of the largest number of ICU beds in the world per population, its distribution in geographic terms or by public or private hospital is heterogeneous. There are 25 ICU beds per 100,000 inhabitants and 7.6 public ICU beds per 100,000 inhabitants, rates that on average are close to most European countries (Rhodes et al 2012; Instituto Brasileiro de Geografia e Estatística 2016). However, distribution ranges from fewer than 3 beds per 100,000 inhabitants in some states in the Northern region to more than 20 beds per 100,000 inhabitants in the Southeast states (Rhodes et al 2012, IBGE 2016).
Brazilian
Critical Care Society
The Brazilian Critical Care Society (Associação de Medicina Intensiva Brasileira - AMIB amib.org.br) plays a major role in the specialty. Founded in 1980, it is the sole provider of board examinations for specialists. There are currently 5,797 physicians that specialise in adult critical care and 1,539 in paediatric critical care. There are currently 44 active centres running critical care residency programmes (38 adult, 5 paediatric) and in 2016 there are 234 physicians training in these centres. The society’s educational arm is a rich source of information and training through its website as well as through local events. It provides hundreds of courses per year and holds an annual congress with 5,000 attendees. Among books, consensus and other publications, a highlight is the Brazilian Journal of Intensive Care (rbti.org.br), a Pubmed/Medline indexed medical journal published jointly with the Portuguese Society of Critical Care in English, Portuguese and Spanish.
Quality of Care
The National Health Surveillance Agency (ANVISA) is responsible for regulatory rules for ICU care organisation. The Health Ministry defines the public policy and ANVISA is responsible for surveillance, inspection and control of quality of care and organisational aspects throughout the country. The rules and criteria for opening an ICU and to classify its ability to care for patients presenting different severity levels (from I to III) are published in a document known as RDC No. 07 (National Health Surveillance Agency, Ministry of Health 2010), which determines the minimal requisites for ICU functioning, including the requirements for healthcare services inside the ICU and inside the hospital structure, equipment, monitoring tools and quantitative and qualitative composition of the medical and healthcare allied professional teams. All ICUs require full presence of medical staff 24/7. A boardcertified intensivist should be the responsible ICU physician, and at least one board-certified physician should be in charge of patient care during the day. Night shifts can be covered by non-board certified professionals. Reimbursement is affected by classification based on this document, and level III units receive higher values than level I and II.
See Also: Study: Brazil QI Intervention Did Not Reduce Mortality
Despite these requirements,
unfortunately some units outside the main cities in the South and Southeast
regions still lack board-certified professionals, and in these settings
telemedicine regulation could be an important measure to improve quality of
care.
Recent data from the
Organizational Characteristics in Critical Care (ORCHESTRA) study (Soares et al.
2015) showed that only 21% of units had the presence of a board-certified intensivist
24/7, although this factor was not associated with better outcomes. In this
study, better nurse-patient ratio was associated with increased ICU
efficiency. The only organisational characteristic associated with better outcomes
was the number of care protocols.

The effects of protocols were consistent across subgroups including surgical and medical patients as well as different severity levels. In addition, results suggest that collaborative multidisciplinary work among ICU care providers impacts favourably on the patients’ outcomes, since hospital mortality was lower in ICUs where protocols were jointly managed by different care providers.
Another relevant aspect of ICU regulation in Brazil, is the need to collect and report quality indicators to ANVISA on a regular basis. Use of severity-of-illness assessment tools (e.g. Acute Physiology and Chronic Health Evaluation [APACHE-II] or Simplified Acute Physiology [SAPS 3], the latter recommended by AMIB), standardised mortality rate, occupancy rate, central line-associated bacteraemia, or ventilator-associated pneumonia are examples of obligatory variables. AMIB has developed a project (UTIs Brasileiras – utisbrasileiras.com/en) in partnership with EPIMED® to provide access to an online performance monitoring tool in which this information can be collected and assessed for performance evaluation and benchmarking among different ICUs throughout the country. EPIMED® Monitor System is a Brazilian commercial cloud-based registry for quality improvement (epimedsolutions.com/en), performance evaluation, and benchmarking purposes that has more than 1,000,000 Brazilian patients included. This is a big data opportunity to generate knowledge and better understand critical care in Brazil.
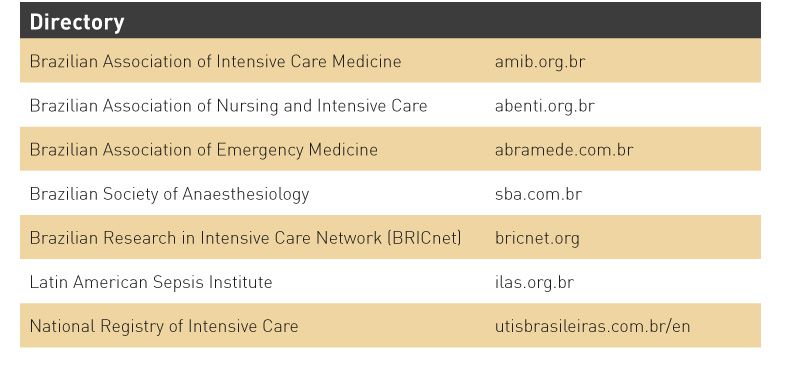
Research Networks
The critical care scenario is changing quickly in Brazil and new challenges are arising, including translating investments in structure, education and research into better healthcare and reducing the mortality that is still unacceptably high for many types of severe acute illnesses in our country (BRICNet (Brazilian Research in Intensive Care Network) 2014). To respond to these demands, it is crucial to organise regional research networks assessing these critical issues in the care of critically ill patients. Brazil hosts initiatives on research, such as the Latin American Sepsis Institute (ILAS- ilas.org.br), the Brazilian Research in Intensive Care Network (BRICNet – bricnet.org/english) and AMIB-Net (Comitê Científico da BRICNet 2014).
AMIB-Net is a network, run by the Brazilian Critical Care Society (AMIB) since 2009, that supports and runs observational studies focusing on education and professional development. It reaches almost every ICU professional throughout the country and has developed several surveys and identified areas of interest and geographical particularities for future projects in Brazil.
The Brazilian Research in Intensive Care Network (BRICNet) is an active and independent organisation. Collaboration with international research networks is intense and has allowed many studies to enrol a large number of ICU and patients in Brazil. Since 2007 BRICNet has been able to endorse and run several multicentre observational studies as well as support local and international studies and investigators. Their results have helped us to improve current knowledge on the epidemiology and organisation of critical care in Brazil. Recent initiatives resulting in studies most relevant to Brazil include the Checklist- Trial (Writing Group for the CHECKLIST-ICU Investigators and the Brazilian Research in Intensive Care Network (BRICNet) 2016) and the ORCHESTRA Study (Soares et al 2015), amongst several others supported by this network.
The Latin America Sepsis Institute (ilas.org.br) is a reference in Brazil for clinical studies, continuous medical and allied healthcare professions education, and quality improvement initiatives implementation in sepsis. This network has included more than 40,000 septic patients since 2004 and its projects aim to improve quality of care and knowledge on sepsis in Brazil and Latin America.
Challenges and
Opportunities
There are of course many
challenges and opportunities in the field of critical care medicine in Brazil.
These challenges represent enormous opportunities for improvement in the
delivery of care, and present an enormous task that can only be successful if
all stakeholders, policy makers and society acknowledge them and work on
sustainable actions and long-term plans.
The first challenge is to provide universal and timely access to critical care. This is especially important to care not only for the daily challenges such as sepsis, trauma and respiratory failure, but also for emerging threats that include Zika and Dengue (Bozza and Salluh 2010; Bozza and Grinsztejn 2016).
Austin et al. (2014) evaluated acute care services supply in seven cities of diverse economic background, including a city in Brazil (Recife). This demonstrated that urban acute care services vary substantially across economic regions and economic differences play only a partial role. Thus, in some cities, despite adequate provision of ICU beds, there was substantial difference in mortality rates (Austin et al 2014). Certainly, several aspects seem to play a role in the gap observed in mortality rates in sepsis (Kaukonen et al. 2014; Conde et al. 2013; Machado et al. 2013)and acute respiratory failure (Azevedo et al. 2013) between low and middle-income countries as compared to high-income countries. One is the incomplete translation of evidence to practice as observed by the relatively low adherence to best practices such as low tidal volume (Azevedo et al. 2013) and light sedation (Writing Group for the CHECKLIST-ICU Investigators and the Brazilian Research in Intensive Care Network (BRICNet) 2016). However, a recent Brazilian study made clear that when protocols and other feasible organisational factors are in place, outcomes are improved (Soares et al 2015). Another study showed that checklists may improve adherence to some of the best practices and improve the safety climate and teamwork (Writing Group for the CHECKLIST-ICU Investigators and the Brazilian Research in Intensive Care Network (BRICNet) 2016). Last, but not least, adequate staffing patterns are to be established with two main special focuses. The first is to make specialists available for rural areas. Whilst this is hard to achieve even in high-income countries with continental dimensions technology can help decrease the gaps with the use of telemedicine and the availability of specialists for remote consultation. The second is to increase the nurse to bed ratio as well as the number of specialised nurses, as they play a key role in the implementation of protocols and infection control measures.
Conclusion
Critical care is a fast-evolving medical field in Brazil that carries opportunities and challenges as big as the continental dimensions of the country. To address these challenges involvement of the main stakeholders is crucial and increased data on epidemiology as well as clinical studies that tackle the aspects of translating evidence to practice are urgently needed.
Conflict of Interest
Jorge Salluh is founder and shareholder of Epimed Solutions. Thiago Lisboa declares that he has no conflict of interest.
References:
Azevedo LC, Park M, Salluh JI et al. (2013) Clinical outcomes of patients requiring ventilatory support in Brazilian intensive care units: a multicenter, prospective, cohort study. Crit Care, 17(2): R63.
PubMed ↗
BRICNet (Brazilian Research in Intensive Care Network) (2014)
Research networks and clinical trials in critical care in Brazil: current status and future perspectives. Rev Bras Ter Intensiva, 26(2):79-80.
Cadastro Nacional de Estabelecimentos de Saude (2016) [Accessed: 20 Jul 2016] Available from http://cnes.datasus.gov.br
Conde KA, Silva E, Silva CO et al. (2013) Differences in sepsis treatment and outcomes between public and private hospitals in Brazil: a multicenter observational study PLoS One, 8(6): e64790.
PubMed ↗
Instituto Brasileiro de Geografia e Estatística (n.d.) Observatorio das cidades. [Accessed: 20 July 2016] Available from cidades.ibge.gov.br/xtras/fontes.php
Kaukonen KM, Bailey M, Suzuki S et al. (2014) Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000-12. JAMA, 311(13): 1308-16.
PubMed ↗
Machado FR, Salomão R, Rigato O et al. (2013) Late recognition and illness severity are determinants of early death in severe septic patients. Clinics (Sao Paulo), 68(5): 586-91.
PubMed ↗
Paim J, Travassos C, Almeida C et al. (2011) The Brazilian health system: history, advances, and challenges. Lancet, 377(9779): 1778-97.
PubMed ↗
Rhodes A , Moreno RP (2012) Intensive care provision: a global problem.Rev Bras Ter Intensiva, 24(4): 322-5.
PubMed ↗
Soares M, Bozza FA, Angus DC et al. (2015) Organizational characteristics, outcomes, and resource use in 78 Brazilian intensive care units: the ORCHESTRA study. Intensive Care Med, 41(12): 2149-60.
PubMed ↗
Writing Group for the CHECKLIST-ICU Investigators and the Brazilian Research in Intensive Care Network (BRICNet) (2016) Effect of a quality improvement intervention with daily round checklists, goal setting, and clinician prompting on mortality of critically ill patients: a randomized clinical trial. JAMA, 315(14): 1480-90.
PubMed ↗
Bozza FA, Salluh J. (2010) An urban perspective on sepsis in developing countries.
Lancet Infect Dis, 10(5): 290-1.
PubMed ↗
Bozza FA, Grinsztejn B (2016) Key points on Zika infection for the intensivist.
Intensive Care Med,42(9): 1490-2.
PubMed ↗
Austin S, Murthy S, Wunsch H et al. (2014) Access to urban acute care services in high- vs. middle-income countries: an analysis of seven cities. Intensive Care Med, 40(3): 342-52.
PubMed ↗
National Health Surveillance Agency, Ministry of Health. (2010) Resolução-RDC Nº 7, de 24 de Fevereiro de 2010. [Accessed: 8 September 2016] Available from www20.anvisa.gov.br/segurancadopaciente/index.php/legislacao/item/rdc-7-de-24-de-fevereiro-de-2010
World Health Organization (2015) Brazil: WHO statistical profile. [Accessed: 8 September 2016] Available from http://www.who.int/gho/countries/bra.pdf?ua=1








