HealthManagement, Volume 18 - Issue 3, 2018
Primary care and wellness centres, dedicated units for sub-acute care and rehabilitation, as well as ambulatory day surgery centres, are key components of the Intercare Group’s healthcare model in South Africa.
The patient-centred organisation structures its services around the health status and needs of a patient and not merely the traditional levels of care. It represents a transition from the outdated traditional hospi- and provider-centric model, offering consumers accessibility and convenience through the location of their facilities, extended operating hours, high-quality clinical care, and reduced costs amid an escalating disease burden. The Intercare Group is an example of what is possible when one is profoundly committed to change and willing to invest, collaborate and partner to make that change a reality.
Achieving value in healthcare
When it comes to the question of value in healthcare, for us it’s about achieving the best outcomes at the lowest cost. We focus on outcomes that matter to patients, and I think our focus on integration and the consumer has assisted us in realising this vision. We combine the very best healthcare professionals with state-of-the-art facilities and equipment to deliver high-quality clinical care and maximise the experience of our patients. We have made value an overarching strategy for the Intercare Group, which informs everything we do. From its inception 16 years ago, the business has been built in a stepwise fashion, consistently building upon and expanding our services and expertise in a conscious journey towards becoming a value-based healthcare organisation.
Making healthcare accessible on a primary care level
Traditional primary care practices in South Africa are often stand-alone, with few associated services or attractions for patients. In addition, they generally only house general practitioners and a patient needs to travel to several different locations to access other healthcare services, whether this is pathology, radiology, pharmacy or other medical providers. Another characteristic is relatively limited operating hours, with practices often being closed over weekends or public holidays. This was largely symbolic of the doctor-centric nature of the healthcare system.
From the outset, we recognised that accessibility and convenience were important for patients and was something that we needed to place at the centre of our care delivery model. We achieved this in a number of ways. A report from PriceWaterhouseCoopers in 1999 highlighted that consumers want healthcare in retail spaces. We adopted this approach and our first medical centre was situated in a shopping centre, associated with a large retail pharmacy. Property owners and developers were initially resistant to the idea, because they didn’t understand the value of healthcare being based in these areas. However, creating the right partnerships helped us through this and once they understood the model, they began to actively seek out our medical centres to form anchors in their retail environment.
In addition to its physical positioning, we implemented extended operating times, including being open on weekends and public holidays. We also wanted to reduce the physical fragmentation in the location of medical services and brought a multitude of primary care services under one roof in a multi-disciplinary medical home. In our centres, patients can access general practitioners, dentists, radiology, pathology, physiotherapists, psychologists, dieticians, optometrists, audiologists and also a pharmacy.
More recently, we have made significant investments in optimising how our patients can access our services, developing online booking capabilities and setting up a call centre dedicated to making bookings and coordinating the care of our patients. Currently, telemedicine and out-of-facility care are forming major parts of our strategy.
Comprehensive, risk-based care delivery models
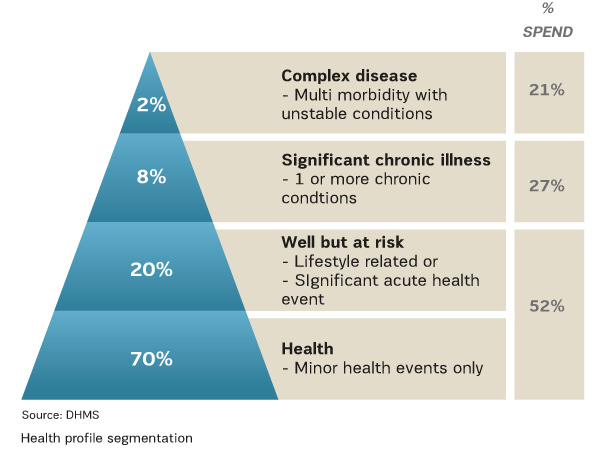
Any population can be classified into four general categories based on their health status and as such be represented on a pyramid. The majority of individuals, forming the base of the pyramid, will be healthy, with only episodic health events such as infections or injury. The next level is those who are at risk of developing chronic diseases due to certain risk factors, usually related to lifestyle. Further up the pyramid are patients who are living with one or more chronic disease, but who are relatively well. The tip of the pyramid is composed of individuals who are really struggling with their health, usually suffering from multiple illnesses and who have to interact frequently with the healthcare system due to complications of their conditions. The top two tiers in this pyramid make up only 10-15% of the population, but account for around 50% of the total healthcare spend.
Traditionally, healthcare systems and organisations structure their offering around levels of care, but the Intercare Group model is based on providing care to patients according to their health needs, in terms of where they are in the health continuum. This is why we consider our primary care and day hospitals to be on the same level, as they care for patients that are mostly well with only episodic healthcare needs. Our sub-acute and rehabilitation hospitals and primary care centres are positioned on the higher level, as they both deal with chronically ill patients with complex and ongoing medical needs.
The overall aim however, irrespective of the facility type, is to prevent individuals from moving up the pyramid, and to try and bring those more ill patients down a level.
Servicing the base of the pyramid - Wellness, primary care and day hospitals
Our primary care centres place a significant emphasis on preventative services through, for example, the promotion of appropriate vaccination programmes and the provision of lifestyle advice. They also focus a huge amount of their attention on screening and early detection, including cervical, breast and prostate cancer, HIV and diabetes, hypertension and dyslipidaemia. Indeed, Intercare outperforms the national average for almost 90% of the primary care screening and prevention metrics used in the country.
We also work very closely with Discovery Vitality, an incentive-based behaviour modification programme aimed at making people healthier. Here we partner with them to develop and operate Wellness Centres, which are able to offer comprehensive screening and prevention benefits to their members under one roof.
The ultimate aim of our work in this space is to ensure that individuals do not move up the health pyramid by addressing risk factors and preventing the development of chronic conditions.
Day hospitals represent a cost-effective alternative to surgery conducted in acute settings. The proportion of eligible surgeries performed as same-day cases in South Africa is very low, sometimes two to three times lower than in other countries. We realised early on that entering this market was aligned with our strategy of reducing costs while maintaining quality, as well as structuring our care delivery model as an out-patient based one.
Supporting patients with complex needs
The rising burden of chronic diseases together with ageing populations are resulting in a significant increase in the number of patients with multiple co-morbidities and complications. The current healthcare system with its fragmented, fee-for-service model is unable to deliver the care these patients need, in the way that they need them.
We believe that with the right approach, many of these patients can still be effectively managed at a primary care level, and we do so through several programmes with leading health insurers. I think that our success has been through our creation and use of Integrated Practice Units, which are multi-disciplinary, co-located and focused teams of healthcare professionals. In this way, we have achieved much success in reducing ER visits, unnecessary out-of-hospital specialist visits and preventable hospital admissions.

Our sub-acute and rehabilitation hospitals also focus on patients with complex medical needs. These include patients who have suffered strokes or other forms of brain injury, spinal cord injuries, severe motor vehicle accidents or require post-operative rehabilitation to help ensure maximum restoration of mobility and quality of life. In order to achieve this, we have set up multi-disciplinary teams typically composed of a general practitioner, nurse, case manager, physiotherapist, speech therapist, occupational therapist, psychologist, dietician and importantly, a social worker. These professionals come together frequently as a team to discuss each case, and also conduct meetings with the patient’s family or caregivers. They also work very closely with the health insurer and are integrated in terms of data exchange between the two. Intercare was the first group to develop a programme with Discovery Health on utilising this model of care to reduce admissions following discharge. Readmissions were reduced by 33% and preventable admissions by 50%.
Ensuring high-quality clinical care
Clinical quality and outcomes are obviously key elements of value in healthcare and it has always been important to us to ensure that these elements are of the highest possible standard. We have achieved this in several ways.
Before founding the group and opening our first medical centre in 2002, I was Chief Executive Officer of the South African Medical Association for over a decade. This gave me insight into the standards and quality of primary care in South Africa, and allowed me to select and approach the doctors that I knew were top-class. Since then we have continued to carefully select the healthcare professionals we wish to bring into our operations.
We also believe that passion and expertise are a powerful combination and usually produce the best outcomes and quality of care. As such, we invest in programmes to upskill our doctors and nurses in a field of their interest to create “primary care specialists”. Not only do we see improved outcomes with such an approach, but these practitioners usually deliver care at a lower cost, as well as with more confidence and awareness of evidence-based guidelines. They tend to order fewer tests, refer less and prescribe the optimal medical interventions the first time. We have run very successful disease management programmes on this basis, including for major depression and diabetes mellitus.
Internal peer review is also important and we are introducing such a model within the group. Each one of our medical practices has one of their own doctors trained as a peer reviewer, and they in turn work with a higher level review committee in the group to assess and improve their quality and cost profiling. The practice level peer-reviewers then take back the recommendations and actions to their fellow doctors in the practice. We also work very closely with several large health insurers in South Africa on profiling programmes and pay-for-performance remuneration structures.
You might also like: Resuscitation in Resource-Poor Settings – A Southern Africa Experience
Achieving integration
Because of the breadth of the group's service offering, including primary care centres and two types of hospitals, and the number of different types of medical services housed within them, we ran the risk of just replicating the fragmentation seen in the South African healthcare system in general. We needed to find ways of bringing them together for the benefit of our patients and the health insurers and large corporates which we serve.
In response to this, we decided to create a separate entity within the group, called Intercare Salubrity. Intercare Salubrity is a risk management company and helps to aggregate demand by insurers, wellness companies and corporates for providers, and to aggregate supply by consolidating the offerings of multiple different facilities and professionals for those requiring healthcare services. Importantly, the care delivered within this system is fully coordinated, essentially presenting a single integrated healthcare system in which patients can have their health managed.
Salubrity also helps to coordinate and integrate patient care and flow between our facilities. For example, many of the patients admitted to our sub-acute and rehabilitation facilities post stroke have uncontrolled chronic conditions such as hypertension and diabetes. Following the completion of their rehabilitation programme, these patients are discharged from the sub-acute hospital into disease management programmes operated in our primary care centres. This helps to ensure their primary conditions are better managed and helps to prevent readmissions.
Leading doctors through the turmoil
In our business review, we came across a quote from Toby Cosgrove, then CEO of Cleveland Clinic. He said: “To help physicians move beyond grief and anger about what they might be losing as the healthcare system remodels, leaders must shift the conversation to something different—something positive, noble and important” (quoted in Moriates et al. 2015).
We have found that the challenge is not to convince doctors of the principle of fixing healthcare, but rather to get them comfortable with the uncertainties in a system that is still figuring itself out. Future expectations of health insurers, patients and reimbursement generate the most concern.
It is about changing the message from one about challenges and shortcomings (poor quality and rising costs) to one of opportunities (better outcomes and reimbursement that rewards good care over volumes).
Intercare has worked hard in this space, constantly engaging with clinical leadership within the organisation and doctors on the ground and is now setting up various structures to support doctors in buying in to the required changes.
Strategic collaboration and partnerships
Strategic partnerships are very important in breaking down the siloed structure of the healthcare system sometimes characterised by defensive self-interest, mistrust and a scarcity mentality. One of the most strained relationships traditionally has been between providers and health insurers. Intercare has largely led the way in changing how healthcare providers interact and work with insurers in South Africa. Anuschka Coovadia, head of healthcare for Africa at KPMG said at Davos in 2015: “Innovative provider-payer partnerships are emerging on our healthcare landscape. These new models are built on the fundamental principles of providing the right care, at the right cost, to the right patient in the right environment.” She said an excellent example of this is the partnership between Intercare and the leading health insurer in South Africa, Discovery Health. Intercare and Discovery have co-designed, implemented and managed several successful healthcare programmes, which have benefited both provider and insurer but most importantly, the patient.
Often, strategic partnerships are also valuable in facilitating integration and aligning incentives. Intercare also works with leading providers in other areas of our healthcare industry, including pathology, imaging, pharmacy, pharmaceuticals and medical technology, to set up programmes and systems which are able to deliver true value for patients.
Future of healthcare
I think most readers will be familiar with the future trends in healthcare – consumerisation, decentralisation, digitisation, AI, and increased focus and accountability for value and so on. We believe that the future is here, but not here entirely. We are operating in an interesting and challenging, intermediary state, an ice cube that is standing in a puddle of its own water, neither completely ice nor completely water. It is a challenging time, as the demands of the new system pull at the structures and capacities of the old.
The lightbulb was an incredible technological advancement, but its impact would have been dependant on widespread electrical supply to all households. In the healthcare space artificial intelligence and various technologies will only realise their full potential when mindsets, data systems, funding models and legislation allow them too.
As a group, we are standing up and taking on the challenge of being a leader in this change, despite the difficulties that it presents and the investments which are often required.
References:
Moriates C, Arora V, Neel Shah N, eds. (2015) Understanding value-based healthcare. New York: McGraw-Hill Education.
PriceWaterhouseCoopers (1999) HealthCast 2010. Available from uemo.org/members/docs/2000/00-091/00-091.







