HealthManagement, Volume 19 - Issue 2, 2019
Critical review
A critical review of eight identified cases of muscle injuries in professional FCB players from the club’s annual muscle injury database in 2017.
Abstract
In cases of suspected muscle injury, sports medicine professionals use imaging methods such as ultrasound (US) and Magnetic Resonance Imaging (MRI) to confirm the diagnosis.
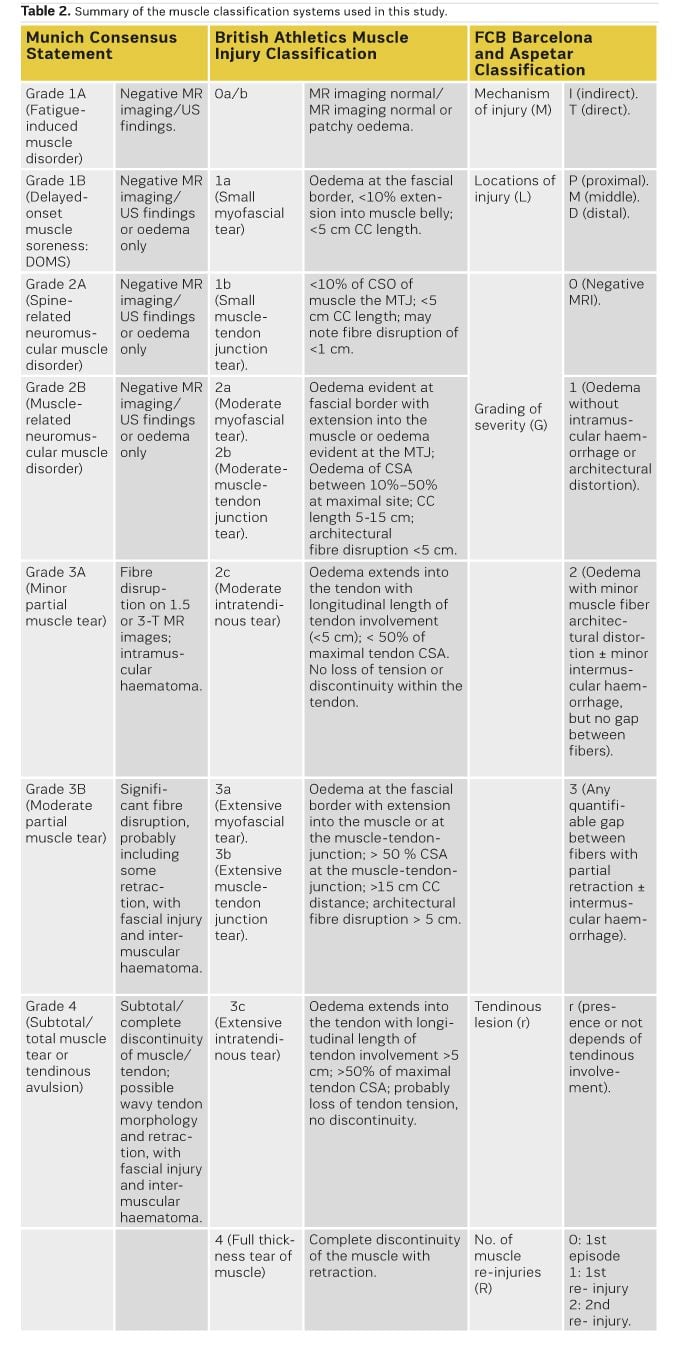
Various classification systems are available for determining the degree of severity of muscle injuries. The staging of muscle injuries depends on the qualitative and quantitative characterisation of several radiological findings by MRI. However, not all classifications use the same criteria to determine the severity of the injuries.
During the 2017-2018 seasons, the medical department of Fútbol Club Barcelona (FCB) has used these classifications to evaluate the prognosis and time to return to sport (RTS) for professional athletes following injury. However, the histological complexity and particularity of each muscle belly mean that image classifications are not infallible.
Introduction
Muscle injuries account for more than 30% of sports injuries (Ekstrand et al. 2011) and have severe implications for professional teams (Elliott et al. 2011). The most common mechanism of muscle injury in football players is muscle strain (indirect muscle injury) in the lower limbs, during eccentric contraction.
In the professional setting, player availability is paramount. When players become injured, it is important to accurately determine the severity of their injury, ie the time until they return to sport, as well as the risk of re-injury (Orchard et al. 2005; Waterworth et al. 2017). This requires an accurate diagnosis of the injury, which is particularly important for muscle injuries.
Currently, the most widely used techniques for confirming and assessing the extent of sports-related muscle injuries are ultrasound (US) and Magnetic Resonance Imaging (MRI), and the information obtained using these techniques helps to guide management, which directly affects prognosis (Blankenbaker and De Smet 2004: Fleckenstein et al. 1989).
MRI can be used to characterise the muscle injury in detail, and with high sensitivity, which allows the radiologist to categorise its severity according to various classifications. Therefore, these classifications guide the sports physician’s therapeutic approach.
You might also like: Patient safety culture
Various injury classifications have been proposed with the aim of connecting the imaging findings to the results of the clinical examination, and thereby to improve the grading of muscle injury severity and reduce the risk of re-injury. Recently, three new classifications have been proposed: the Munich Consensus Classification (Mueller-Wohlfahrt et al. 2013), the British Classification System (Pollock et al. 2014), and the FCB Barcelona and Aspetar Classification (Valle et al. 2017). These classifications focus on various factors that are key for good diagnosis and prognosis: mechanism of injury, location of the injury, presence of fibre retraction, extent of oedema (cross-sectional area), and previous injuries (re-injury).
Despite the utility of these classification systems, injury classification remains challenging due to differences in muscle architecture, injury extension, activities when the lesion occurred, the mechanism of injury, and even the player’s personality. Since each of these classifications uses different parameters to categorise muscle injuries, this can lead to conflicting treatment decisions.
The aim of this paper is to update current knowledge in sports medicine imaging by evaluating the use of these classifications, and the discrepancies that arise between them. Specifically, we demonstrate the use of these classifications for categorising muscle injuries in 8 specific cases of muscle injury in football players seen at the FCB Medical Center.
Materials and Methods
We identified eight cases of muscle injuries in professional FCB players from the club’s annual muscle injury database in 2017. We selected these cases based on several criteria:
i) The player was affiliated with the FCB professional football team at the time of the injury;
ii) The injury was located at the myoconnective junction of an important muscle for football (hamstring, rectus femoris, adductor or calf muscles);
iii) According to diagnosis, the treatment criteria were conservative (injuries requiring surgery, such as pure tendon tears, were excluded).
All injuries were evaluated during physical examination by a sports medicine physician (one of the two team doctors), after which MRI was performed in our own medical centre. All injured players underwent the same initial physiotherapy plan and re-adaptation protocol, which were managed by the same sports physiotherapist. Finally, the decision to return to sport was taken according to the criteria of FCB medical staff.
MRI studies were generally acquired within 24 hours post-injury, at the FCB Medical Center using a CANON MRI 3T VANTAGE TITAN, and were reported by an MSK radiologist sports specialist. We used a multi-purpose coil with speeder technology, which allowed us to acquire 5 sequences according to the standardised protocol for evaluating muscle injuries in the lower extremities (described in Table 1). The patients were positioned in supine decubitus, and the examination was performed on the injured limb only, and focused on an area marked with a cutaneous vitamin marker.
The MRI findings allow the follow-up US examinations to be targeted to the most relevant areas, assessed by using linear transducers (centre frequency greater than 10–17 MHz) (Allen 2007).
The MRI studies of each case were reviewed by two MSK radiologists (SM, with 10 years of experience; and JI, with 4 years of experience), who were blinded to the clinical information apart from the location of the injury. In case of discrepancies, the case was reviewed by XA, who has >25 years of experience. In parallel, a doctor of sports medicine (XY, RP or GR) reviewed the clinical history in terms of injury mechanism, and also the clinical exploration and US findings.
The radiological findings evaluated were: tendon rupture, peritendon oedema, loss of tendon tension, pennation angle, interstitial oedema of the myotendinous junction, blurring (rupture of fibres), intermuscular oedema and haematoma.
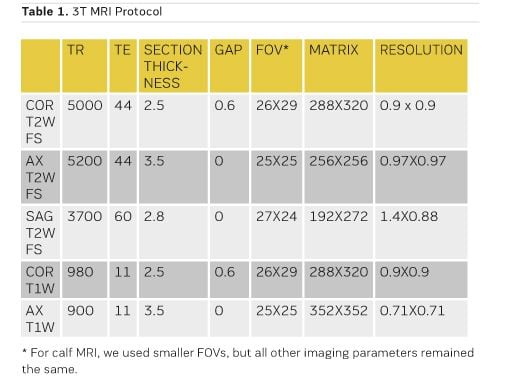
We used the magnetic resonance imaging results to categorise each case according to the classifications selected in our study. Table 2 lists the different categories according to each classification. After categorising each case, we performed an exhaustive analysis of the concordances and discrepancies.
Results
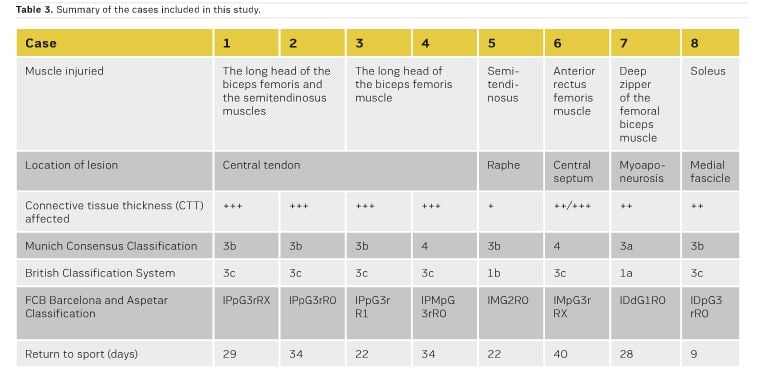
In this section, we present eight cases of muscular injury and describe our clinical approach, radiological features, therapeutic behaviour, time to return to sport, and final outcome. While the injuries studied involved different muscle groups (five long head of the biceps femoral, one semitendinosus, one rectus femoris, one soleous), all except one (myoaponeurotic junction, Case 7) are treated as lesions of the myotendinous junction (MTJ). Six lesions of the MTJ affected thick connective tissue, and one affected fine connective tissue (raphe). We observed a broad range of RTS for these injuries, varying from 9 to 40 days. Table 3 details the muscle affected, location of the injury, injury type, the thickness of the connective tissue involved, and the final categorisation of the injury in each classification system. Below, we describe each case in detail.
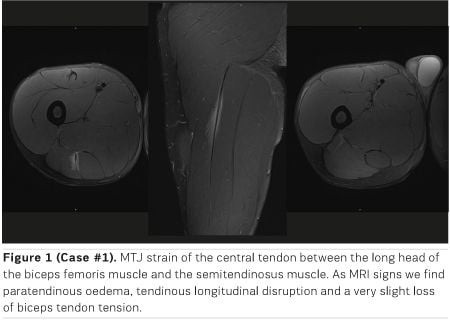
Case #1 (Figure 1)
Subject and circumstances of injury. A twenty-five-year-old professional football player who stopped playing after being referred for sudden pain in the posterior proximal third of the right thigh while sprinting and fighting for a ball during an official match. He was unable to continue playing and needed to be substituted. Palpation and stretching were painful and he was unable to do an isometric contraction.
Imaging: Diagnostic 3T MRI performed within 24 hours showed musculotendinous junction (MTJ) strain of the central tendon between the long head of the biceps femoris muscle and the semitendinosus muscle. Fat-saturated T2 weighted images demonstrated hypersignal of the central tendon with longitudinal intratendinous disruption (5.5 cm long, and 3.3 mm thick), and minimal intermuscular fluid/haemorrhage. There was surrounding oedema (CSA: 10-25% with biceps predominance). Only isolated defects in the distal fine connective tissue were seen. There was very slight loss of biceps tendon tension. As an incidental finding, cicatricial changes seemed to correspond to an old but unknown injury.
Diagnosis: Munich Consensus Classification (MCC): 3b
British Classification System (BC): 3c, FCB Barcelona and Aspetar Classification (FCB-A): IPpG3rRX
Management/outcome: Conservative treatment was proposed. MRI after fourteen days demonstrated healing with signs of partial recovery of the tendon and decreased oedema of the muscle. The player returned to play at 29 days without evidence of re-injury.
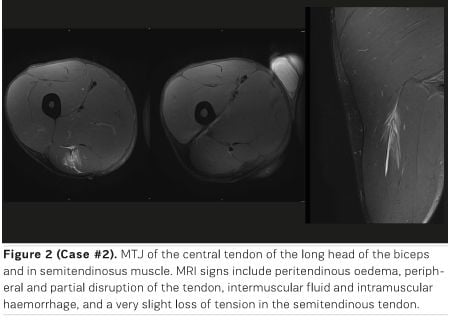
Case #2 (Figure 2)
Subject and circumstances of injury. Twenty-four-year-old professional player referred for muscle cramp in the proximal third of the right hamstring during the last 15 minutes of a football match, although he was able to finish the game. After the match, walking was limited by the pain, and stretch and palpation were also painful.
Imaging: Diagnostic 3T MRI was performed within 24 hours, and showed cicatricial changes in the free tendon of the biceps, and a variant of normality in the central tendon (thick connective tissue is found in long head of the biceps and also in semitendinosus muscle). MRI shows proximal MTJ strain of both muscles. Fat-saturated T2W images demonstrated hypersignal of the central tendon with partial and peripheral disruption, surrounding oedema (CSA: 16-31% with predominance of semitendinosus) and intermuscular fluid/haemorrhage. Only isolated defects in the distal fine connective tissue are seen. Very slight loss of semitendinosus muscle tension is observed.
Diagnosis: MCC: 3b, BC: 3c, FCB-A: IPpG3rR0
Management/outcome: Conservative treatment was proposed. MRI after fourteen days demonstrated healing with signs of partial recovery of the tendon and decreased oedema of the muscle. Return to sport at 34 days without evidence of re-injury.
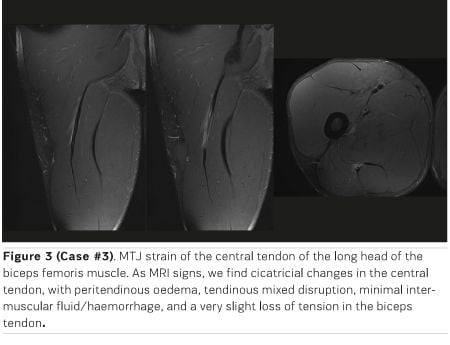
Case #3 (Figure 3)
Subject and circumstances of injury. Thirty-three-year-old football player referred with symptoms of fatigue in the posterior proximal third of the right thigh after playing two consecutive international matches with his National team. After returning to the Club, the physical exam showed painful palpation and the player had difficulty in stretching his hamstring.
Imaging: Diagnostic 3T MRI was performed more than 7 days later. MRI shows MTJ strain in the central tendon of the long head of the biceps femoris muscle. Fat-saturated T2W images demonstrated longitudinal strain of the tendon with transversal extension (3.3 mm transversal gap) and minimal intermuscular fluid/haemorrhage. There was no significant surrounding oedema (subacute lesion). We observed a very slight loss of tension in the biceps tendon. The free tendon was very thick, probably because it was a progressive injury over time (subacute), which leads to extra scar changes.
Diagnosis: MCC: 3b, BC: 3c, FCB-A: IPpG3rR1
Management/outcome: Conservative treatment was proposed. MRI after 20 days demonstrated healing with signal recovery of the tendon and closure of the tendon gap. Return to sport at 22 days without evidence of re-injury.
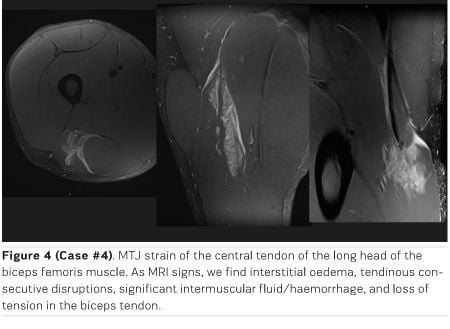
Case #4 (Figure 4)
Subject and circumstances of injury. Twenty-four-year-old football player who presented sudden acute pain in the proximal third of the right hamstring during a very high speed running action during a match, running a distance of around 20 metres. He needed to be substituted immediately. Physical exam showed considerable pain during palpation; walking was impossible, and he needed to use crutches.
Imaging: Diagnostic 3T MRI was performed within 24 hours. MRI shows a long free tendon (11 cm, tendon length from the ischial tuberosity to the origin of the central tendon of the biceps), and an early intramuscular division of the central tendon, as variants of the normality. Imaging also showed MTJ strain of the central tendon of the long head of the biceps femoris muscle. Fat-saturated T2W images demonstrated hypersignal of the tendon with multiple partial disruptions (consecutive rupture in the distal part), surrounding oedema (CSA: 36%), and significant intermuscular fluid/haemorrhage, including vascular structures. Loss of tension in the biceps tendon.
Diagnosis: MCC: 4, BC: 3c, FCB-A: IPMpG3rR0
Management/outcome: Conservative treatment was proposed. MRI after 17 days demonstrated healing with partial signal recovery of the tendon and closure of the tendon gap. Return to sport at 22 days without evidence of re-injury.
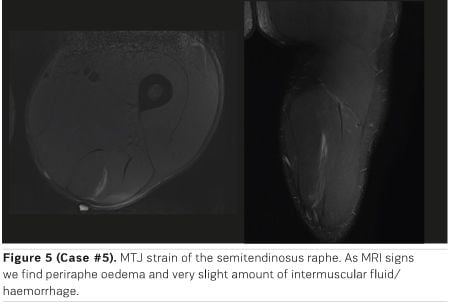
Case #5 (Figure 5)
Subject and circumstances of injury. Twenty-one-year-old player who suffered a cramp in the posterior middle third of his right thigh at the end of a football match. During physical examination palpation was tender, not painful, walking was possible, the range of motion was complete, stretching was only minimally painful, and isometric contraction was possible with only minimal pain.
Imaging: Diagnostic 3T MRI was performed after 7 days. MRI showed MTJ strain of the semitendinosus raphe. Fat-saturated T2W images demonstrated trace raphe (connective tissue of average thickness equivalent to aponeurosis) irregularity with surrounding oedema (CSA: 7.5%), and very slight intermuscular fluid/haemorrhage. No loss of tension was observed.
Diagnosis: MCC: 3b, BC: 1b, FCB-A: IMG2R0
Management/outcome: Conservative treatment was proposed. MRI after 21 days demonstrated healing with partial signs of recovery of the MTJ. Return to sport at 27 days without evidence of re-injury.
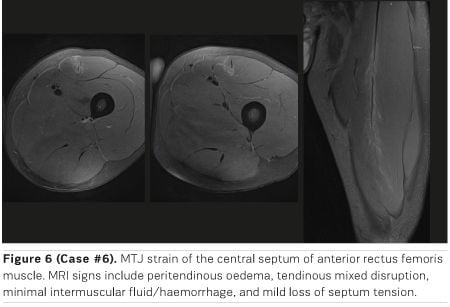
Case #6 (Figure 6)
Subject and circumstances of injury. Twenty-four-year-old professional player referred for acute moderate pain in middle third of his right quadriceps during a change of direction in a match. He chose to leave the game to avoid a more severe injury. Local palpation was clearly painful and stretching of the quadriceps was also painful.
Imaging: Diagnostic 3T MRI was performed within 24 hours, and showed MTJ strain of the central septum of the anterior rectus femoris muscle. Fat-saturated T2W images demonstrated hypersignal of the tendon with partial disruption in two areas (the proximal one showing a 2.5 mm transversal gap, and the distal one showing a 2.2 mm longitudinal gap), surrounding oedema (CSA: 19.4%) and very slight intermuscular fluid/haemorrhage. Mild loss of tendon tension. Note that the central septum showed varying thickness, suggesting cicatricial changes.
Diagnosis; MCC: 4, BC: 3c, FCB-A: IMpG3rRX
Management/outcome: Conservative treatment was proposed. Return to sport at 40 days without evidence of re-injury.
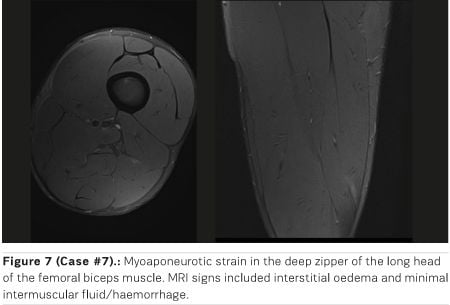
Case #7 (Figure 7)
Subject and circumstances of injury. Thirty-two-year-old professional player who suffered a cramp in the distal third of his hamstring during a side-cutting manoeuvre while running. He initially felt that he had suffered a minor injury. Palpation was slightly painful, the range of motion was complete, and concentric and eccentric muscle contraction was possible without loss of strength.
Imaging: Diagnostic 3T MRI was performed within 24 hours. MRI shows myoaponeurotic strain in the deep zipper of the long head of the femoral biceps muscle. Fat-saturated T2W images showed hypersignal at the aponeurotic border without significant fibre disruption (CSA: 10%), and very slight intermuscular fluid/haemorrhage. No loss of tendon tension was observed.
Diagnosis: MCC: 3a, BC: 1a, FCB-A: IDdG1R0
Management/outcome: Conservative treatment was proposed. MRI after 20 days demonstrated healing with signs of partial recovery of the tendon and closure of the tendon gap. Return to sport at 28 days without evidence of re-injury.
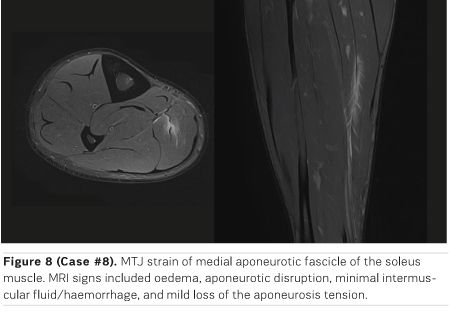
Case #8 (Figure 8)
Subject and circumstances of injury. 33-year-old player who reported feeling discomfort at the end of a football match. He had a history of muscle injury in the same leg.
Imaging: Diagnostic 3T MRI was performed two days later, and showed MTJ strain of the medial aponeurotic fascicle of the soleus muscle. Fat-saturated T2W images demonstrated hypersignal of the muscle fibres consistent with oedema (CSA: 4.9%) associated with a gap in the medial aponeurotic fascicle (about 4 mm) and moderate intermuscular fluid/haemorrhage. Mild loss of the aponeurosis tension was observed.
Diagnosis: MCC: 3b, BC: 3c, FCB-A: IDpG3rR0
Management/outcome: Conservative treatment was proposed. Return to sport at 9 days without evidence of re-injury.
Discussion
In this paper, we have categorised sports injuries using three different classification systems, and have found discrepancies in terms of the severity of the injury. In turn, we find that injuries with similar radiological characteristics result in RTS of different durations.
US offers a fast, inexpensive and dynamic muscle assessment for detection and severity assessment of muscle injuries. However, it has low sensitivity in the diagnosis of some type of lesions (deep muscle compartments, proper connective tissue evaluation) (Balius et al. 2014).
3-Tesla MRI technology allows us to obtain better images of muscle architecture and muscle injuries, especially the level and quantity of connective tissue injured. MRI is usually performed unilaterally (affected limb only) by using a dedicated surface coil to ensure higher resolution images with thinner sections and smaller field of view. A skin marker should be placed over the area presenting symptoms, according to the clinical orientation. It is helpful to perform fluid-sensitive sequences (T2 weighted in our case) with a moderate echo time (TE) (less than 50 ms) to obtain proper resolution of the connective tissue (Siriwanarangsun et al. 2016). These sequences allow for i) the detection of oedematous changes around the myotendinous and myofascial junctions, ii) an accurate assessment of the connective tissue, and iii) the delineation of intramuscular or perifascial fluid collections or haematomas. T1-weighted spin-echo sequences are useful for assessing subacute haemorrhage or haematomas, and also for detecting atrophy and fatty infiltration and scar tissue in chronic injuries. To accurately evaluate the morphology and extent of muscle injuries, multi-planar acquisitions (axial, coronal, and sagittal) are required.
In our experience, early acquisition of magnetic resonance imaging is important for adequate diagnosis of acute muscular injuries. However, a recent study reported that there were no significant day-to-day changes in the extent of the oedema during the first week following acute hamstring injury (Wangensteen et al. 2017).
Striated muscle tissue stands out for its great contractile function, which depends largely on the connective tissue associated with it and the essential role of this connective tissue for maintaining the integrity and proper function of the muscle (Fuller et al. 2006, Balius et al. 2013). The skeletal muscle architecture contains connective tissue at different locations and with different thicknesses. Its predominant role is to transmit the contractile forces, although in case of fasciae, raphes or extracellular matrix, it also acts as a structural unit (Gillies and Lieber 2011; Brukner et al. 2018). In addition, in case of pure contractile connective tissue, we can observe differences between free tendons and intramuscular tendons or connective tissue (Brukner et al. 2018). While this differentiation is clinically very important for determining the severity and prognosis of muscle injuries, in the literature these structures have generally been referred to indistinctly (Balius et al. 2013).
Also, currently classifications only partly distinguish between these structures. We propose that currently classifications include the type of the functionally or structurally compromised tissue, as well as its thickness (mild, medium or significant). We consider fascias and raphes as having mild thickness; aponeurosis, septa and distal portion of the intramuscular tendon as having medium thickness; and the proximal portion of the intramuscular tendon and free tendon as having significant thickness (Table 3).
In addition to the complex histoarchitectural configuration of the muscle, the distribution of the connective tissue within it is unique and unrepeatable for each muscle belly (Balius et al. 2013; Lieber and Friden 2000). Given the great variety of muscle groups and the multiple factors that influence injuries, the recovery time of these injuries is very variable, even for injuries that occur in the same muscle or muscle group (Lieber, Friden 2000). Current muscle injury classifications encompass all muscles indiscriminately, which is a limitation for objectively determining the degree of severity. Based on our analysis of the players in this study, we believe that many injuries with different severities are included in the same category based on the MRI results. Despite this, the time to RTS differs markedly between cases, mainly because it also depends on other non-imaging factors. Of all of these cases, Case 6 shows the most consistent categorisation according to the three classification systems, in terms of the degree of severity and prognosis. In this case, we consider that there has been a significant compromise of the "functional" thick connective tissue, which was associated with a long RTS (Prakash et al. 2018).
These classifications do not take into account congenital or adaptive anatomical variants (underlying scar), which are fundamental in the analysis, as we have shown in Cases 2 and 4. On the other hand, the appearance of incidental cicatricial lesions in the absence of a clinical history of a previous injury could cause problems in classifying the injury (Case 1 and 6). Similarly, we have observed progressive clinical presentation over time, or "subacute", (Case 3), with late acquisition of MRI in which cicatricial lesions were associated, and where it was difficult to assign the category "R".
Each injury has anatomical particularities that could result in an over-evaluation of its severity, and therefore prolong the RTS. For example, in Case 4 the lesion involved vascular venous structures that caused abundant interstitial and intermuscular fluid. The RTS was the same as in Case 2, although Case 2 was classified as a 3b injury according to Munich Consensus Classification. In contrast, the Munich classification does not consider isolated interstitial oedema to be an indirect lesion (Case 7).
According to the FCB-Aspetar classification, from a radiological point of view, we consider that for some injuries we overestimated the degree of severity (Cases 1, 2, 3, 6 and 8). This issue is based on whether the "G2-3" consideration depends a quantifiable gap between muscle fibres. That said, we note that this classification has the advantage that it allows one to directly categorise connective tissue injuries using the letter "r". In the FCB-Aspetar classification, in some cases it can be difficult to determine the location of the lesion between proximal and distal, depending on the tissue involved. This is true in Case 5, in which the raphe was involved, and in which it has been difficult to reach a consensus to determine if it is proximal or distal.
Another important factor in determining RTS is the physical condition of the player. For example, while Case 3 involved an injury with poor prognosis and involvement of thick functional connective tissue, this did not result in a higher RTS than other less severe cases. In this same case, the mixed morphology of the connective tissue involvement could have conditioned a longer RTS. Thus, it would be interesting for future classification to include the type of rupture of the connective tissue (longitudinal, transversal, mixed, etc.); currently classifications only distinguish between partial and complete ruptures.
Finally, we believe that while several radiological signs are used in existing classifications, not all of allow consistent grading of injury. In our opinion, oedema (CSA) and intermuscular fluid are not very influential factors in the severity of the injuries. In contrast, compromised connective tissue has a highly relevant role but is currently only poorly specified in current classifications.
Standardised classifications for defining the severity and prognosis of muscle injuries help sports medicine professionals to determine the most appropriate therapeutic approach and RTS. However, the histological complexity and peculiarity of each muscle belly means that current image classifications are not infallible. In addition, not all of the many radiological signs available are equally relevant in terms of prognosis. Perhaps developing a severity classification for each muscle group, and taking into account each factor in a particular way, would bring us closer to a more consistent and effective evaluation system for muscle injury.
Conflicts of interest: None to be declared.
Funding: None.
Authors’ contributions: J. Isern-Kebschull and S. Mechó: guarantors of integrity of the entire study; J. Isern-Kebschull, S. Mechó and X. Yanguas: literature search; J.M., G.R. and J.P: data collection and clinical studies; J. Isern-Kebschull, S. Mechó and X. Alomar: analysis; J. Isern-Kebschull and S. Mechó: writing of the manuscript. All authors: interpretation of data, manuscript revision for important intellectual content, and approval of the final draft.
Acknowledgements
The authors thank Francesc López Ferrer (radiographer at FCB-ASB MR) and Gavin Lucas (www.the papermill.eu) for critical reading and language editing.
Abbreviations and acronyms
Fútbol Club Barcelona (FCB), Return to Sport (RTS), Myotendinous Junction (MTJ), Munich Consensus Classification (MCC), British Classification System (BC), FCB Barcelona and Aspetar Classification (FCB-A).
Key Points
- US and MRI are currently the most widely used techniques for confirming sports-related muscle injuries.
- MRI is the most sensitive technique for properly characterising muscle injuries.
- Recently, three new classifications have been proposed: the Munich Consensus Classification, the British Classification System, and the FC Barcelona and Aspetar Classification.
- Standardised Classifications help professionals in sports medicine to define the most appropriate therapeutic strategy and RTS following muscle injuries.
Next Article: Achieving zero avoidable patient deaths by 2020
References:
Allen GM (2007) Ultrasound in sports medicine—a clinical evaluation. Eur J Radiol 62: 79–85
Balius R, Rodas G, Pedret C, Capdevila L, Alomar X, Bong DA (2014) Soleus muscle injury: sensitivity of ultrasound patterns. Skeletal Radiology 43(6): 805–812
Balius R, Alomar X, Rodas G, et al (2013) The soleus muscle: MRI, anatomic and histologic findings in cadavers with clinical correlation of strain injury distribution. Skeletal Radiology 42(4): 521–530
Blankenbaker D, De Smet AA (2004) MR-imaging of muscle injuries. Appl Rad 33: 14–17
Brukner et al (2018) Does the intramuscular tendon act like a free tendon? Br J Sports Med Month 0: 1-2
Ekstrand J, Hägglund M, Waldén M (2011) Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med 39(6): 1226–1232
Elliott MC, Zarins B, Powell JW, Kenyon CD (2011) Hamstring muscle strains in professional football players: a 10-year review. Am J Sports Med 39(4): 843–850
Fleckenstein JL, Weatherall PT, Parkey RW, Payne JA, Peshock RM (1989) Sports-related muscle injuries: evaluation with MR imaging. Radiology 172: 793–798
Fuller CW, Ekstrand J, Junge A, Andersen TE, Bahr R, Dvorak J, et al (2006) Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Br J Sports Med 40: 193–201
Gillies AR, Lieber RL (2011) Structure and function of the skeletal muscle extracellular matrix. Muscle & Nerve 44(3): 318–331
Lieber RL, Friden J (2000) Functional and clinical significance of skeletal muscle architecture. Muscle Nerve 23(11): 1647–1666
Mueller-Wohlfahrt HW et al (2013) Terminology and classification of muscle injuries in sport: The Munich consensus statement. Br J Sports Med 47(6): 342-50
Orchard J, Best TM, Verrall GM (2005) Return to play following muscle strains. Clin J Sport Med 15: 436–41
Pollock N et al (2014) British athletics muscle injury classification: a new grading system. Br J Sports Med 48(18): 1347-51.
Prakash A, Entwisle T, Schneider M, et al (2018) Connective tissue injury in calf muscle tears and return to play: MRI correlation. Br J Sports Med 52(14): 929–933
Siriwanarangsun P, Statum S, Biswas R, Bae WC, Chung CB (2016) Ultrashort time to echo magnetic resonance techniques for the musculoskeletal system. Quant Imaging Med Surg 6: 731-43
Valle X et al (2017) Muscle injuries in sports: a new evidence-informed and expert consensus-based classification with clinical application. Sports Med 47(7): 1241-53
Wangensteen A, Bahr R, Van Linschoten R, et al (2017) MRI appearance does not change in the first 7 days after acute hamstring injury—a prospective study. Br J Sports Med 51: 1087–92
Waterworth G, Wein S, Gorelik A, Rotstein A (2017) MRI assessment of calf injuries in Australian Football League players: findings that influence return to play. Skeletal Radiol 46: 343–350









