Despite underlying physiological differences and a different set of risk factors, diagnosis, management, and treatment strategies for hypertension do not account for sex and gender variances.
Evidence-based guidelines for hypertension treatment from clinical trials are similar between males and females; however, most of these trials do not include any risk stratification of sex and gender (Wenger et al. 2018). Even from the start of medical education, students are taught a single set of risk factors and treatments to be applied to both sexes despite any underlying physiologic differences. The Center for Disease Control (CDC) estimates that 1 in 3 people have hypertension, and with half the population being female, the impact of not accounting for sex and gender variances can lead to poorer quality of care and worse outcomes.
Risk Factors: How Important are the Sex and Gender Differences?
Although hypertension becomes more prevalent with age in both males and females, the timeframe of onset is unique for each. Hypertension rates in premenopausal women are lower when compared to men of the same age cohort (Muiesan et al. 2016) whereas, after age 50, women have a higher rate of hypertension than men (Benjamin et al. 2018). Regardless of gender, all people with hypertension are at an increased risk of developing cardiovascular disease (CVD). The differences, however, fall within the risk factor profile. For example, men tend to have the more traditional risk factors whereas women often will present with less traditional risk factors (Tziomalos et al. 2014).
Traditional Risk Factors
- Tobacco use
- Hyperlipidaemia
Non-traditional risk factors
- Renal disease
- Abdominal obesity
In females, onset of menopause is associated with a 2-fold increase in the risk of HTN and increased cardiovascular risk (Barton and Meyer 2009). Blood pressure levels at this time depend on age and duration of menopause, suggesting oestrogen deficiency to be a contributing factor. After a woman undergoes menopause, she is found to have an elevated BMI as compared to before, as well as abnormal glucose metabolism (Nuzzo et al. 2010). These sex-related factors may contribute to the development of metabolic syndrome, which in turn leads to an elevated blood pressure and increased risk of CVD.
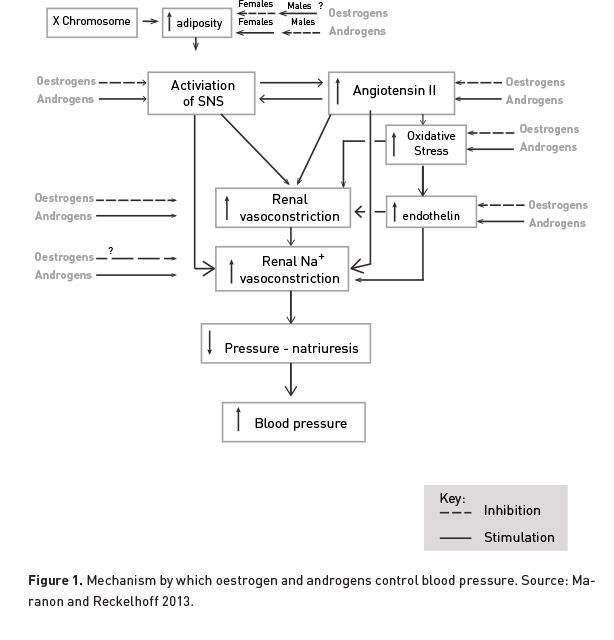
There are currently multiple hypotheses regarding why women have a unique set of risk factors for hypertension compared to men, the first of which involves the role of female sex hormones. While a female is premenopausal, she is benefiting from oestrogen’s protective effects. Oestrogen has been found to activate nitric oxide, leading to inhibition of the sympathetic system, thus causing vasodilation (Samad et al. 2008). Women have more arterial oestrogen receptors than men, and a premenopausal woman, who has the highest level of oestrogen production, is able to most benefit from the vascular effect (Tadic et al. 2019).
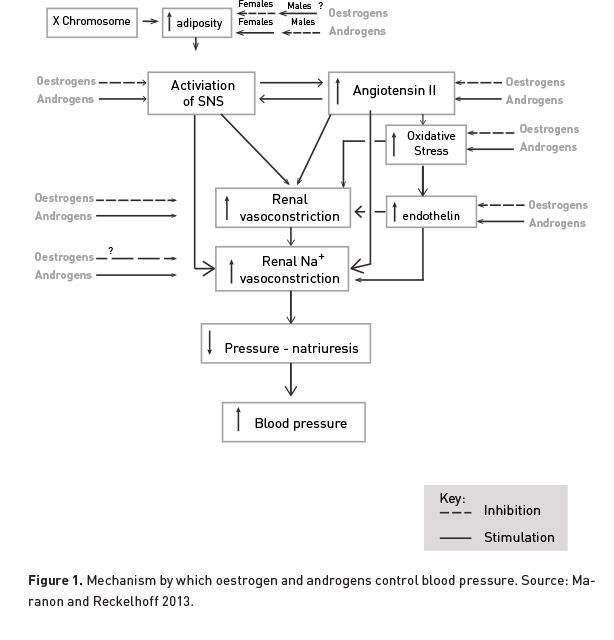
A second hypothesis regarding female-specific pathophysiology of hypertension suggests that a greater anti-inflammatory immune profile in women with hypertension may be a compensatory mechanism to limit increases in blood pressure. Evidence shows that ovarian hormones can reduce plasma renin levels and ACE activity, thus leading to decreased angiotensin 2 levels. Angiotensin type 2 receptors, which promote an anti-inflammatory profile, have greater activity in women (Lombardi et al. 2017).
Diagnosis and Treatment of Hypertension
Current guidelines in diagnosis of hypertension require multiple office visits with elevated blood pressure. Menopausal women often have more fluctuation in blood pressure measurements than men, which can lead to a lower likelihood of positive diagnosis (Kagitani et al. 2015). Despite the differences in risk factors, there is limited data regarding gender-specific screening strategies for hypertension.
The National Health and Nutrition Examination Survey (NHANES) from 1999-2011 showed a discrepancy of awareness and treatment of hypertension between gender. Young adults, particularly young males, were found to have poorer control of hypertension compared to all other age cohorts and age-matched females. The NHANES study estimated a difference of 28% of improved hypertension awareness, 60% difference in treatment for hypertension, and a 52% difference in control of blood pressure in younger women. The incongruity is hypothesised to be due to more frequent healthcare visits by young adult women versus age-compared men (Zhang and Moran 2017).
In November 2017, the American Heart Association published new recommendations for blood pressure control and treatment. These guidelines were based off the SBP Intervention Trial (SPRINT), a 2015 study that reported intensive blood pressure control was associated with lower all-cause mortality compared to standard blood pressure control in patients with high risk of CVD. The results of the SPRINT trial were eagerly awaited to aid in creating updated guidelines, but there have been significant critiques of the study and how broadly it can be applied. The average age of the participants was 70, and just about 30% of the participants were women (Wenger et al. 2016).
Treatment targets of hypertension are not gender-specific, and men and women generally demonstrate similar responses to medication. In women, thiazide-type diuretics are the preferred first-line therapy due to the additional benefit of protection from bone loss and hip fractures (Mosca et al. 2011). If there are any other known comorbidities, the patient should additionally be treated with a beta-blocker and an ACE inhibitor.
The side effect profile of antihypertensive drugs has been noted to vary between sexes. Women are 1.5-1.7 times more likely to develop side effects than men (August and Oparil 1999). With diuretic use, women are more likely to develop hyponatraemia, hypokalaemia, and arrhythmias. Women also more commonly develop ACE-inhibitor related cough and calcium-channel blocker-related peripheral oedema (August and Oparil 1999).
Physicians and researchers have previously considered the effectiveness of hormone therapy on blood pressure control. There have been multiple studies done with inconclusive results, some showing an improvement in BP control, some showing further increases and blood pressure, and some showing no effect.
REGARDS (Madsen et al. 2019) noted that increasing hypertension and incident ischaemic stroke was almost 2x more prevalent in women compared with men and suggested that blood pressure control and risk factor reduction utilise a sex-specific approach.
Comorbidities, Mortality, and Other Considerations
The leading cause of death in the United States is heart disease, and the primary modifiable risk factor for heart disease is hypertension. Although a larger percentage of men (24.4%) die from heart disease than women (22.3%), women are more likely to develop adverse consequences as a result of their hypertension (Arias et al. 2013). For each 10 mmHg increase in SBP in women, there is a 25% increased risk of developing CVD. In men, the risk is only increased by 15% (Wei et al. 2017).
A study that analysed blood pressure control rates among hypertensive women with CAD showed that women who had a prior MI or revascularisation procedure were at a higher risk for stroke, MI, and death (Sava et al. 2019). These women were also women with elevated blood pressures and also more likely to develop left ventricular hypertrophy, diastolic dysfunction, increased arterial stiffness, diabetes, stroke, and chronic kidney disease (Wenger et al. 2018).
Conclusion
Sex and gender are important facets of a patient’s healthcare experience. Although there are numerous similarities in risk factors and treatment between the sexes, there are gender-related differences in underlying physiology and pharmacokinetics, as well as social and environmental factors, that can affect clinical decision-making. Further research with an accurate representation of the general population is becoming more prominent, but without exploring these concepts with medical students, patients will not be receiving the best possible personalised care.
Key points
- 1 in 3 people have hypertension and half of this population is female.
- Not accounting for sex and gender variances can lead to poorer quality of care and worse outcomes.
- Women have a unique set of risk factors for hypertension compared to men.
- Sex and gender are important facets of a patient’s healthcare experience and must be considered to ensure best possible personalised care.
Arias E, Heron M, Xu J (2013) United States life tables. Natl Vital Stat Rep, 66:64.
August P, Oparil S (1999) Hypertension in women. J Clin Endocrinol Metab, 84:1862-66.
Barton M, Meyer MR (2009) Postmenopausal hypertension: mechanism and therapy. Hypertension, 54:11-18
Benjamin EJ, Virani SS, Callaway CW et al. (2018) Heart disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation, 137:e67-492.
Kagitani H, Hoshide S, Kairo K (2015) Optimal indicators of home BP variability in premenopausal women and associations with albuminuria and reproducibility: the J-HOT home BP study. Am J Hypertens, 28:586-594.
Lombardi M, Severi P, Mazza A et al. (2017) Sex differences in hypertension: A question worth asking? Ann Clin Hypertens,1:1-5.
Madsen TE, Howard G, Kleindorfer DO et al. (2019) Sex Differences and Stroke Risk in the REGARDS Study. Hypertension., 74:00-00
Maranon R, Reckelhoff JF (2013) Sex and gender differences in control of blood pressure. Clinical Science, 125:311-8.
Mosca L, Benjamin EJ, Berra K et al. (2011) Effectiveness-based guidelines for the prevention of cardiovascular disease in women – 2011 update: a guideline from the American Heart Association. Circulation, 123:1243-62.
Muiesan ML, Salvetti M, Rosei CA et al. (2016) Gender differences in antihypertensive treatment: myths or legends? High Blood Press Cardiovasc Prev, 23:105-13
Nuzzo A, Rossi R, Modena MG (2010) Hypertension alone or related to the metabolic syndrome in menopausal women. Expert Rev Cardiovasc Ther, 8:1541-8.
Samad Z, Wang TY, Frazier CG et al. (2008) Closing the gap. Treating hypertension in women. Cardiology in Review, 16:305-13.
Sava RI, Chen YE, Smith SM et al. (2019) Risk and Blood Pressure Control Rates Across the Spectrum of Coronary Artery Disease in Hypertensive Women: An Analysis from The INternational VErapamil SR-Trandolapril STudy (INVEST). Journal Of Women’s Health.
Tadic M, Cuspidi C, Grassi G et al. (2019) Gender-specific therapeutic approach in arterial hypertension—Challenges ahead. Pharmacological Research, 141:181-188.
Tziomalos K, Giamptzis V, Baltatzi M et al. (2014) Sex-specific differences in cardiovascular risk factors and blood pressure control in hypertensive patients. J Clin Hypertens, 16:309-312.
Wei YC, George NL, Chang CW et al. (2017) Assessing sex differences in the risk of cardiovascular disease and mortality per increment in systolic blood pressure: a systematic review and meta-analysis of follow-up studies in the United States. PLoS One, 12:e0170218.
Wenger NK, Arnold A, Bairey Merz CN et al. (2018) Hypertension across a woman’s life cycle, 71;1797-1813.
Wenger NK, Ferdinand KC, Bairey Merz CN et al. (2016) American College of Cardiology Cardiovascular Disease in Women Committee. Women, hypertension, and the Systolic Blood Pressure Intervention Trial. Am J Med, 129:1030-6.
Zhang Y, Moran AE (2017) Trends in the prevalence, awareness, treatment, and control of hypertension among adults in the United States, 1999-2014. Hypertension, 70:736-42.