HealthManagement, Volume 23 - Issue 3, 2023
The scale of destruction wreaked on human life and happiness by cancer hardly needs any illustration. Significant disparities exist between countries, caused primarily by differences in national wealth and income. OncoSeek provides good accuracy in detection and diagnosis and will be a game-changing and life-saving multi-cancer early detection test.
Key Points
- 84% of the global population lives in low- and middle-income countries (LMICs) with a lack of medical infrastructure, personal financial resources and basic diagnostics out of reach.
- Cancer is often only recognised and diagnosed late in these regions.
- When diagnosed early, treatments like surgery and radiotherapy are still possible and available at a relatively low cost, whereas late-stage cancer requires more advanced and expensive treatments that are out of the question in a low- and middle-income setting.
- An AI-enhanced algorithm can help optimise accuracy. OncoSeek provides good accuracy even in early-stage detection and diagnosis.
The Patient’s Experience
After being diagnosed with Stage 3 cancer of the cervix, Patient D.A.O communicated how unfair it was that, after spending five years visiting health facilities and spending everything she had on her national insurance (150,000 Ksh {Kenyan Shilling, at the time of writing 1USD was equivalent to approximately 140 KSh}), she finally learned that she had a late-stage cancer which cannot be cured because it was diagnosed too late. We had failed her.
A second patient, L.O.O., who was diagnosed with Stage 4 cancer of the oesophagus and needed to have a stent fitted to continue eating after a late diagnosis, could not hold back his tears telling me how he had spent almost 3,000,000 Ksh over the past 3-4 years in different private hospitals seeking diagnosis, treatment and cure for the fact that he could no longer eat solids, and because he had never had insurance cover, he had to use all his savings and sell his parcels of land to receive a very late diagnosis, and an oesophageal stent for swallowing, as he waited for his death.
The third patient, M.S.O., was diagnosed with Stage 4 cancer of the prostate after spending 870,000 Ksh at various public health facilities, private clinics and laboratories due to difficulty urinating. His children had to stop schooling because he could no longer pay their college fees, and he lost his job due to long-term sickness absence. His wife also left due to the difficult task of caring for him while sick and the loss of income, which meant a big change in his home life.
These stories were taken from the recent personal experience of Dr Arthur Ajwang, a General Practitioner at the Kisumu Teaching and Referral Hospital in Kenya.
Dr Ajwang characterises the situation as follows: “Late diagnosis of cancer in the low- and middle-income countries, especially in Africa, contributes to 70-80% of annual cancer mortality. There is also the issue of misdiagnosis at many levels of the healthcare system, e.g. when vague symptoms mean that healthcare workers do not have a high index of suspicion and go on to perform multiple diagnostic tests looking for other diagnoses, which can take years, not to mention thousands of shillings and a toll on the patients and their relatives before cancer is finally diagnosed in very late stages. Another handicap is that, despite several cancer screening techniques being available in clinical practice, the high cost of these methods and the need for specialised infrastructure and skilled technicians limit their application.”
Statistics and Patterns
These personal observations can be underpinned by the following statistical evidence:
- 84% of the global population lives in low- and middle-income countries (World Bank data for 2021).
- Cancer mortality after diagnosis in LMICs is much higher than in high-income countries (Sung et al. 2021).
- Mortality rates in sub-Saharan Africa now rank among the highest in the world (Sung et al. 2021).
- Low survival rates in sub-Saharan Africa are largely attributable to late-stage presentation (Sung et al. 2021).
- One study (McCormack et al. 2020) concludes that a projected 416,000 women will die from breast cancer in sub-Saharan Africa between 2020 to 2029, yet with downstaging (diagnosis at an earlier stage) and improved treatment at least a third of these deaths could be prevented.
Late-stage diagnosis results in vast numbers of unnecessary deaths and devastation of the financial and social position of families and children. Reasons for late diagnosis are many (Khama Rogo Lecture 2022), including:
- Low levels of cancer awareness and lack of knowledge.
- Lack of access to trained medical staff.
- Long distance from medical facilities.
- Fraudulent medical practices.
- Technical limitations.
- Lack of money.
Design Parameters for the Scientist
These are the factors that the scientist has to take into account to develop a useful diagnostic tool for this specific context (Luan et al. 2023). Their diagnostic method needs to meet the following basic criteria:
- High-accuracy diagnosis based on one single blood sample.
- Capacity to detect multiple cancers.
- Contribution to early detection and diagnosis.
- Universal, standardised and automatic technical laboratory platform.
- Technical laboratory platform within three days of postal delivery to maintain blood sample quality.
- Cost is low enough for broad application in LMICs.
Additional design choices include:
- Use of multiple protein assays and artificial intelligence to reduce false positives.
- Need to assist in finding tissue of origin.
- Need for upgradability to improve specificity, sensitivity and coverage of more cancer types.
The result is a diagnostic using a panel of seven Protein Tumour Markers (PTMs). The core of the diagnostic is an AI-enhanced algorithm called OncoSeek that has been trained and validated with 7,565 blood samples to calculate the Probability Of Cancer (POC) based on the quantities of the seven PTMs plus the age and sex of the person involved. The results were then verified with the data from a second cohort (provided by Johns Hopkins University School of Medicine) of 1,817 samples.
Thanks to the AI algorithm, a very high specificity (probability of a negative result if the disease is not present) of 92.9% was obtained. This is desirable in any setting, but especially in LMICs because false positives cause the patient great anxiety and require extra cost for subsequent verification of the diagnosis by other means. High specificity means lower sensitivity (probability of a positive result if the disease is actually present), or in other words, more missed positives. In the present version, the sensitivity is 51.7% and in cases where the test result is positive, OncoSeek also delivers a first indication of the Tissue Of Origin (TOO) with an accuracy of 66.8%.
This performance makes OncoSeek suitable for diagnosing more types of cancer at earlier stages, thus improving the outcome for the patient by treating the disease when it is typically most responsive to therapy. In the early stages, surgery and radiotherapy are regularly successful, and they are also often available in low-income settings, as opposed to therapies for advanced-stage cancers, like complex chemotherapy, targeted therapy or immune therapy. The OncoSeek test requires a simple tube of blood which can be drawn by a nurse or a midwife and then sent by mail for analysis in a central laboratory with standard lab equipment. In many countries, one central laboratory will be sufficient because the test relies on protein quantities rather than Whole Genome Sequencing, which is more costly. The total cost of the test is the sum of the costs connected to taking the blood sample, mailing the sample to the central laboratory, operating standard lab equipment, processing the data and communicating the results, all of which are available and affordable for very many people in LMIC, showing that the diagnostic meets the design criteria and choices mentioned earlier.
Next Step
Until now, we have described the journey of the diagnostic from the patient to the clinical laboratory and scientific literature. Now this method needs to be made widely available to the medical community and to millions of patients in more than a hundred LMICs which will involve implementing the following workflow thousands of times every day: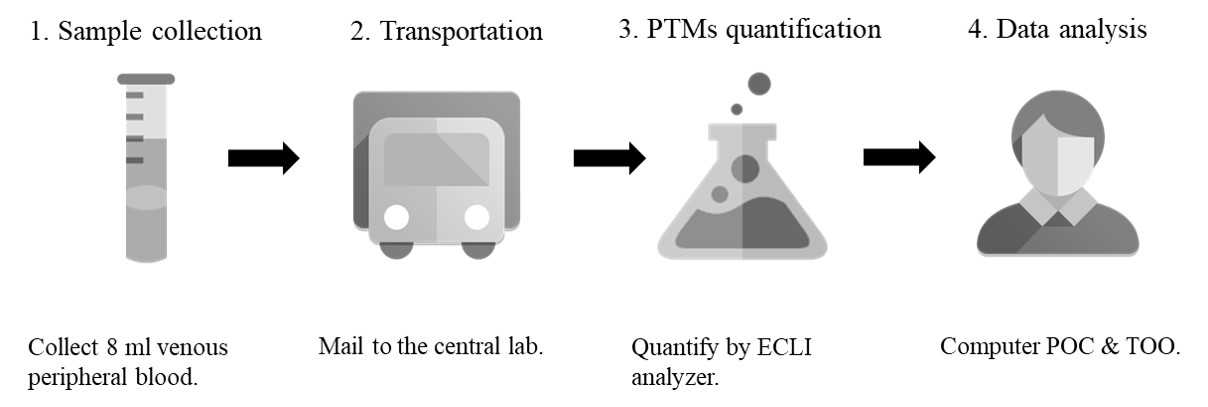
In each country, it starts with gaining acceptance, often by means of a trial, followed by the implementation of an efficient and reliable process and quality guarantees. All process steps need to be designed and contracted with great reliability and at the lowest possible cost, and they also need to comply with national conventions and standard practices. The Inspire2Live Foundation is working closely with SeekIn (the biotech company behind OncoSeek) to find potential investors and coordinate the project implementation and management.
The road ahead is still long but let us take strength in the vision that Dr Ajwang and his patients expressed. “The stories I have heard from oncology patients in the clinic have been quite depressing and heart-wrenching. I shared with them about the innovation of the new multi-cancer screening test kit that we can diagnose multiple cancers early with just a small amount of blood drawn from their veins, and they were happy about it. L.O.O. said that this would be a game changer and lifesaver for his children and relatives, and though he may be dead by the time it starts being used, he will rest peacefully knowing that it will save lives early”.
OncoSeek will save millions of lives in low- and middle-income countries by diagnosing multiple cancers at an earlier stage and starting at a low price expected to continue to fall every year, thus avoiding unnecessary mortalities and saving costs for the families. It will be a game-changing and life-saving multi-cancer early detection test in Kenya and across Africa.
Conflict of Interest
Tieolo Jongmans is an executive for Inspire2Live. Shujia Hao is the CFO for SeekIn Inc.
References:
Khama Rogo lecture. Available at https://inspire2live.org/congresses/inspire2live-annual-congress-amsterdam-14-16-september-2022/
Luan Y, Zhong G, Li S et al. (2021) A panel of seven protein tumour markers for effective and affordable multi-cancer early detection by artificial intelligence: a large-scale and multicentre case-control study. EClinicalMedicine. 61:102041.
McCormack V, McKenzie F, Foerster M et al. (2020) Breast cancer survival and survival gap apportionment in sub-Saharan Africa (ABC-DO): a prospective cohort study. Lancet Glob Health. 8(9):e1203-e1212.
Sung H, Ferlay J, Siegel RL et al. (2021) Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 71(3):209-249.


















