ICU Management & Practice, Volume 24 - Issue 2, 2024
Family dynamics in ICU meetings are complex and often affected by emotions, stress, and differing perspectives. Effective communication and collaboration amid family members and healthcare professionals are crucial for steering these dynamics, facilitating shared decision-making, and assuring the best feasible patient’s care.
Introduction
Intensive care unit (ICU) teams often face various challenges when caring for critically ill patients in addition to direct patient care. Equally important is communication with families to provide support and information. Family meetings become fundamental platforms for bridging the gap between healthcare providers and families. They offer a space where complex details about a patient's condition, treatment modalities, and prognosis can be articulated with clarity and empathy. Informed decision-making depends on understanding, and these meetings provide a context for families to comprehend subtle differences, weigh potential outcomes, and actively participate in decisions that profoundly impact their loved ones.
It is not merely about information dissemination but a recognition of families as important partners in the care process. Through transparent and compassionate communication, healthcare providers empower families to navigate the complexities of critical care. This empowerment extends beyond the immediate decisions to build up a sense of resilience, a vital component in facing uncertain medical trajectories.
Moreover, family meetings in the ICU can be seen as a proactive measure in aligning medical interventions with the values and preferences of the patient. By engaging families in open discussions, healthcare providers not only respect the autonomy of the patient but also enhance the likelihood that treatment plans resonate with the individual's wishes. Gambhir et al. (2021) discussed the impact of a proactive and structured approach to conducting interdisciplinary family meetings with patients and their families, which led to improved patient understanding of their care and satisfaction.
Our Argument
Family meetings in the ICU are not mere procedural checkpoints but ethically necessary. They create a synergy between medical expertise and familial insights, fostering an environment where decisions are not imposed but shared—a collaborative approach that honours the dignity of patients and the profound role of their families in the journey through critical care. Among critically ill patients and their surrogates, a family-support intervention delivered by the interprofessional ICU team did not significantly affect the surrogates’ burden of psychological symptoms, but the surrogates’ ratings of the quality of communication and the patient- and family-centredness of care were better. The length of stay (LOS) in the ICU was shorter with the intervention than with usual care (White et al. 2018).
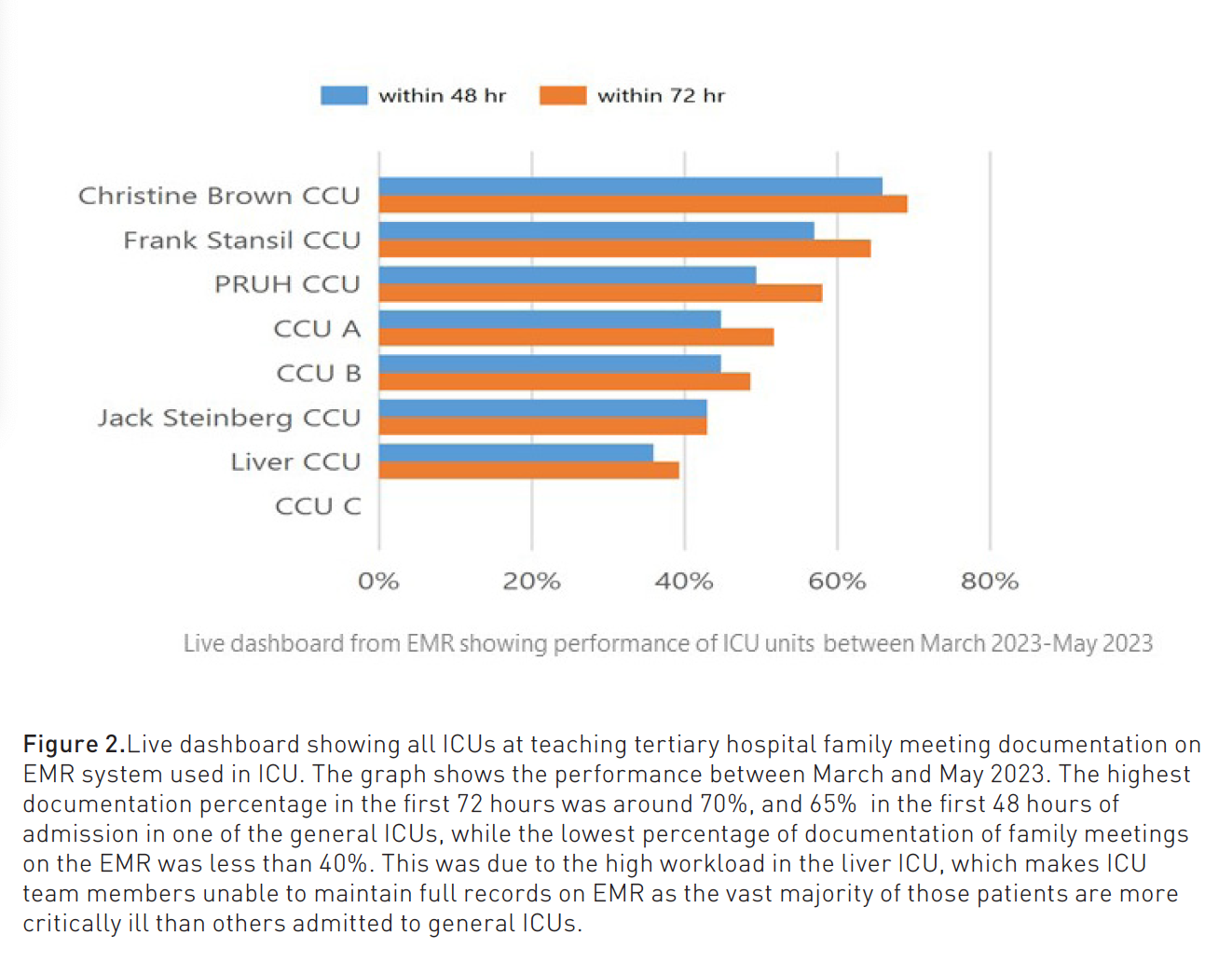
While it is challenging to maintain routine formal family meetings for every patient in the ICU due to clinical workload, it is crucial that junior and senior ICU doctors, as well as bedside nurses, should be involved in family discussions to formulate proper informative family meeting updates. Meetings and discussions with the family should be appropriately recorded and updated for the purpose of being adherent to the international and local standards of the best ICU practice when using electronic medical records (EMR), which would ensure quality improvement in ICU (Elkhonezy et al. 2023).
An intensive communication system within five days of ICU admission and weekly thereafter tested the effect of regular, structured family meetings on patient outcomes and reduced use of ineffective resources in the ICU. 135 patients from 5 ICUs were enrolled as the control group, followed by enrolment of intervention patients (n = 346). There were no significant differences between control and intervention patients in LOS, indicators of aggressiveness of care or treatment limitation decisions (ICU mortality, LOS, duration of mechanical ventilation, treatment limitation orders, use of tracheostomy or percutaneous gastrostomy). The analysis found that in the medical ICUs, the intervention was associated with a lower prevalence of tracheostomy among patients who died or had do-not-attempt-resuscitation orders in place (Daly et al. 2010).


Counterargument
While acknowledging the importance of communication with families in the ICU, it's valuable to consider the practical challenges and potential drawbacks associated with routine formal family meetings for every patient. There are multiple factors contributing to the challenges faced by the ICU team in maintaining formal and documented family meetings. These include but are not limited to overwhelming workload constraints and time sensitivity in ICU, ascritical care situations often demand immediate decision-making and interventions. Routine formal family meetings might introduce delays in providing timely care. Individualised patient and family needs and documentationwhile recording family meeting discussions are essential for adherence to guidelines. Mandating extensive documentation for every patient may divert valuable time and resources from direct patient care. Emotional cost and burnout of healthcare providersandconstant involvement in emotionally charged family meetings can take a toll on healthcare providers. Individual preferences for communication can vary as families come from diverse cultural backgrounds. A rigid approach to routine formal family meetings might lead to less effective communication.Hence, the affirmation should be on the quality rather than the quantity of family meetings.
Ensuring that when family meetings occur, they are well-prepared, focused, and responsive to family-specific needs can be more effective than achieving routine formal meetings. Nelson et al. (2009) described a simple toolkit and prototypes to promote more successful implementation of family meetings in the ICU, which include a family meeting planner, a meeting guide for families, and a documentation template. There is a need to standardise family meeting tools to help family members effectively engage in the process (Singer et al. 2016).
Importance of Family Discussion in the ICU
Imagine a scenario in the ICU where a critically ill and unresponsive patient is facing complex treatment decisions. In this situation, open and honest family discussions become instrumental in formulating the trajectory of care and the expected future outcome. A transparent conversation with the family about the patient's condition, potential interventions, and expected outcomes allows them to comprehend the gravity of the situation. By engaging the family in the decision-making process, healthcare providers not only provide crucial information but also create an environment where the family feels valued, heard, and included.
With such an approach, families can share insights into the patient's values and preferences. This information becomes invaluable, especially when deciding on treatment plans that align with the patient's wishes. Moreover, the shared decision-making process creates a sense of agency in the family, attenuating feelings of powerlessness often associated with critical care situations. When families are actively involved in decisions, they are more likely to understand the rationale behind treatments, potential risks, and realistic expectations for the patient's recovery.
Ethical Challenges Related to Family Discussion in the ICU
Navigating family discussions in the ICU presents healthcare professionals with various ethical challenges and dilemmas. Balancing the duty of truth-telling with the ethical imperative to maintain hope can be challenging. Respecting the autonomy of the patient and including the family in decision-making may be a challenge when conflicts arise as family members have differing opinions. Cultural or religious considerations may impact decision-making. Ensuring culturally competent communication poses an ethical challenge. Cultural sensitivity means what may be considered appropriate disclosure in one culture might be perceived differently in another. Deciding when to initiate discussions about the patient's condition and prognosis is ethically complex. Waiting too long might infringe on the family's right to be informed promptly while introducing discussions too early could cause undue distress.
Ethical challenges arise when deciding to withdraw life-sustaining treatments. Balancing the obligation to preserve life with the ethical principle of not prolonging suffering requires careful consideration. Subsequently, navigating end-of-life discussions and decisions presents ethical challenges. Determining when to transition from curative to palliative care involves balancing the duty to provide comfort and alleviate suffering with respecting the sanctity of life.Determining who has the authority to make decisions on behalf of the patient, particularly when the patient lacks decision-making capacity, poses ethical challenges, especially in families with conflicting opinions.
The family meeting is considered the best practice for achieving patient- and family-centred palliative care by involving palliative care specialists to engage patients and their families in a serious illness discussion and clarify the values of patients and caregivers, provide information, determine care preferences and identify sources of illness-related distress and burden (Glajchen et al. 2022).
The emotional toll on healthcare providers who engage in these discussions is an ethical concern. Balancing empathy with professional detachment, ensuring honest communication without causing emotional harm, and addressing the emotional needs of the healthcare team are all complex aspects.Allocation of resources in the ICU can pose ethical challenges, especially when discussing treatment options that might have financial implications. Striking a balance between providing the best care and considering the overall healthcare system's resource constraints requires ethical discernment.Ensuring continuity of care and consistency in cohesive and coherent communication when multiple healthcare professionals are involved might pose ethical challenges., especially in complex medical situations.
Addressing these ethical challenges in family discussions requires a thoughtful and patient-centred approach, emphasising open communication, cultural competence, and respect for the values and autonomy of both patients and their families.
Multi and Interdisciplinary Role in Family Meetings and Discussion
The ICU team plays a crucial role in family meetings and discussions, with each member contributing unique skills and perspectives. The team collaborates to provide not only medical information but also emotional support and guidance to the family. The ICU physician takes a central role in leading family discussions by providing medical information, explaining the patient's condition, discussing treatment options, outlining the prognosis and ensuring that medical details are conveyed in a clear and understandable manner.
Nursesare often the primary point of contact for families. They provide emotional support, answer questions, and ensure the family's needs are communicated to the broader team. They also play a crucial role in conveying the patient's day-to-day condition, which can help families understand the ongoing trajectory of care.
Social workers address the psychosocial aspects of critical care. They can assist families in coping with stress, provide support resources, and help navigate any non-medical challenges the family may face. Chaplains provide spiritual and emotional support. They can assist families in addressing existential concerns, facilitate rituals, and offer comfort during difficult times, mainly for those with religious or spiritual needs.
Pharmacistsplay a role in explaining medication regimens, potential side effects and interactions. They contribute valuable information regarding the pharmacological aspects of treatment and address any concerns related to medication. Occupational and physical therapists provide insights into the patient's physical condition and potential for rehabilitation. They discuss the patient's ability to perform activities of daily living and provide information on long-term functional outcomes.
Trainees, such as residents or fellows, may be involved in family meetings under the supervision of attending physicians to learn effective communication skills and understand the holistic aspects of patient care. A coordinated approach supports comprehensive care for the patient and their family. Multidisciplinary team collaboration among all team members is crucial. Regular interdisciplinary meetings ensure that everyone is informed about the patient's condition, reducing the risk of miscommunication.
Informed Decision-Making
It is a vital process that requires a comprehensive and compassionate approach. There are key elements contributing to informed decision-making:
- Clear and transparent communication about the patient's condition, diagnosis, and treatment options by using plain language and avoiding medical jargon helps ensure that family members can comprehend the information.
- Honest discussion about prognosis and sharing realistic expectations about the patient's prognosis is crucial. This includes potential outcomes, chances of recovery, and possible complications. It provides the family with a foundation for making decisions aligned with the patient's likely trajectory.
- Discussing the available treatment options and presentation of alternatives, including the benefits, risks, and potential side effects, allows families to understand the implications of each choice. This enables them to actively participate in decision-making.
Informed decisions should align with the patient's values, wishes and preferences. Discussions about the patient's previously expressed wishes should be encouraged, including any advanced care directives or living wills. Presenting a balanced view of the risks and benefits of treatment options helps families weigh potential outcomes. Understanding the potential benefits and burdens allows families to make decisions that align with the patient's best interests.
Furthermore, offering a structured opportunity for family members to ask questions and express concerns fosters an environment of trust. It provides clarity on any uncertainties and allows time for reflection before making decisions. If appropriate, healthcare professionals should support families in seeking second opinions. This ensures that families have access to diverse perspectives and can make decisions with more comprehensive information. The ICU team must understand and respect the cultural and spiritual values of the family. This includes considering beliefs about life, death, and medical interventions, which can significantly influence decision-making. Recognising the emotional impact of critical illness and treatment decisions should be highlighted throughout acknowledging the family's feelings, offering counselling services or involving pastoral care. Establishing a plan for follow-up discussions and regular updates ensures ongoing support and an opportunity to revisit decisions if circumstances change.
Informed decision-making in family discussions is not a one-time event but a process that evolves as the patient's condition changes. It requires ongoing communication, empathy, and a commitment to supporting families through the complexities of critical care decisions.
Emotional and Compassionate Support
This is a critical aspect of family discussions in the ICU, which could be achieved through:
- Active listening to family concerns, fears, and questions without interrupting. Empathy, expressing understanding and compassionbuild a trusting relationship.
- Acknowledging emotional distress that families may be experiencing, validating their feelings creates a safe space for open communication by using empathetic language and avoiding medical jargon to ensure that family members can comprehend the information without feeling overwhelmed.
- Acknowledge the complexities of grief and hope that families may be experiencing simultaneously. The collaborative approach facilitating shared decision-makingempowers them and helps reduce feelings of powerlessness.
- Being mindful of cultural and spiritual considerations, understanding and respecting diverse beliefs contribute to more compassionate care. We should Work collaboratively with support services such as social workers, counsellors, or psychologists hence these professionals can provide specialised emotional support tailored to the family's needs. In situations involving spiritual considerations, involve a chaplain or spiritual advisor. They can provide comfort and guidance aligned with the family's spiritual beliefs.
- Offering physical gestures such as a reassuring touch or offering a tissue can convey compassion. "Non-verbal cues can speak volumes in moments of emotional distress”. Ensure that the physical environment is conducive to supportive discussions. Arrange seating in a way that encourages open communication and maintain privacy when needed.
- After a family meeting, follow up with families to offer ongoing support. This demonstrates a continued commitment to their emotional well-being.
Challenges to Conduct Family Meetings in ICU
Anxiety, grief, and fear are commonemotional distresses. Language barriers or cultural differences may impede effective communication. Critical illnesses often involve uncertain prognoses and complex medical information in many ICU cases. Family members may have conflicting perspectives, values, and expectations, which may be highly challenging. It is sometimes difficult to determine the appropriate time to initiate family meetings, for which starting discussions too early may overwhelm families, while waiting too long may lead to frustration and anxiety. In some situations, this could be affected by time constraints and rotating medical teams. Privacy and space constraints can be a common challenge in the often crowded and bustling environment of the ICU.
End-of-life discussions can be emotionally charged and difficult, and balancing hope with the reality of the patient's condition requires sensitivity and skill. Moreover, healthcare professionals may not receive extensive training in communication skills; hence, it can affect the quality of discussions. It is worth understanding that multifaceted choices with ethical, medical, and emotional dimensions usually affect decision-making. Providing adequate grief and bereavement support to families may be challenging due to time constraints and resource limitations. Finally, one of the challenges impacted by time constraints in the fast-paced environment of the ICU is adequate documentation of family discussions and ensuring timely follow-up.
Patient-Centred Care
It is an approach to healthcare that places the patient at the centre of the decision-making process and emphasises the importance of meeting the individual needs and preferences of each patient. Family meetings are an essential part of the treatment of seriously ill patients. Using a structured approach throughout these meetings is key to achieving patient- and family-centred care for seriously ill patients (Widera et al. 2020). Patient-centred care (PCC) includes showing respect for patient values, empathy and compassion, using a holistic approach (viewing the patient as a whole person including psychological, social and medical needs), shared decision-making, effective communication, individualised care plans (tailored to the individual needs and preferences of each patient), respect for patient autonomy, timely and accessible care, continuous coordination of care, support for caregivers and involving them in the care process when appropriate, patient education through empowering patients with the knowledge to actively participate in their care and measuring patient satisfaction and outcomes using patient feedback to assess the quality of care and essentially respecting privacy and dignity.
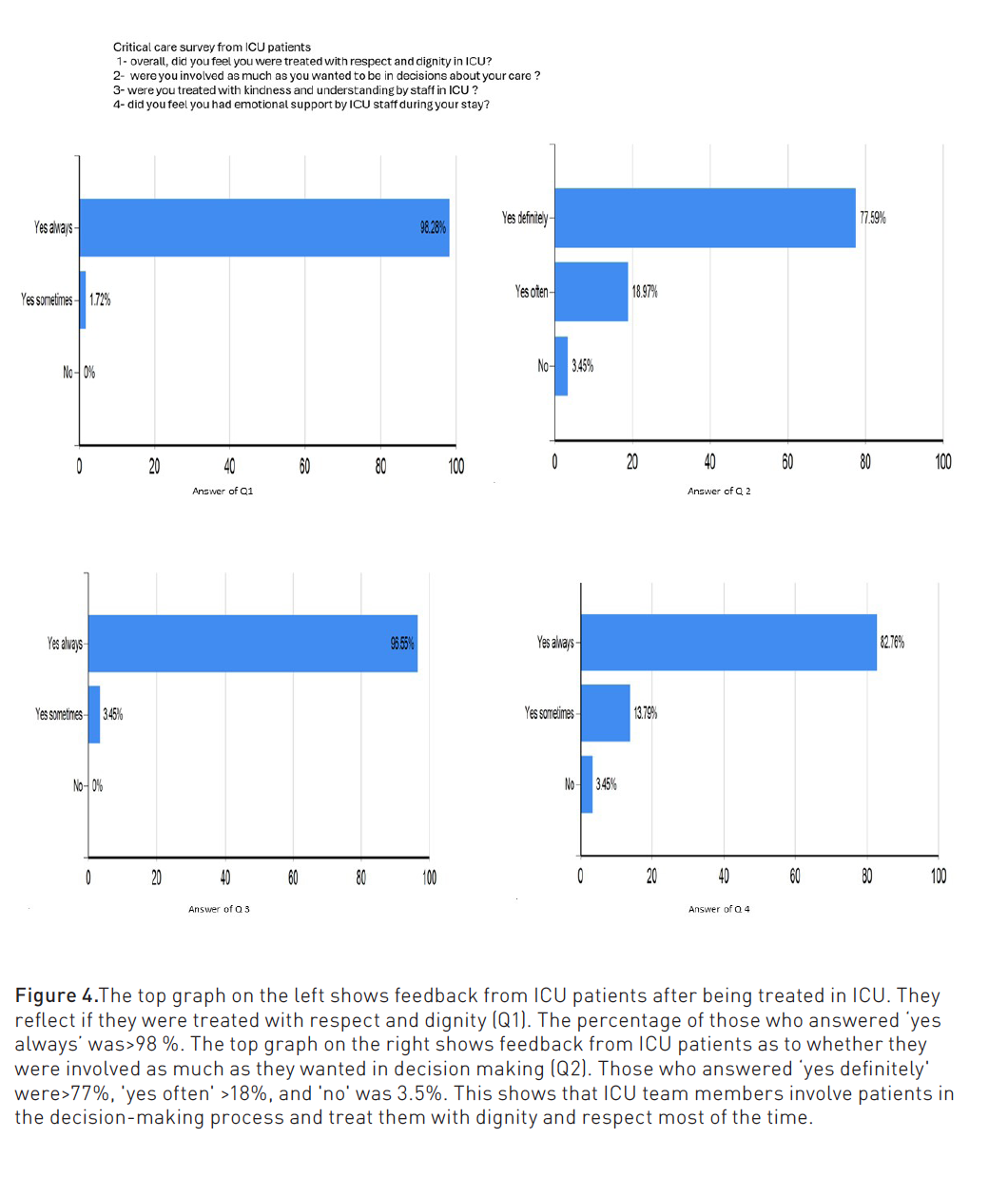
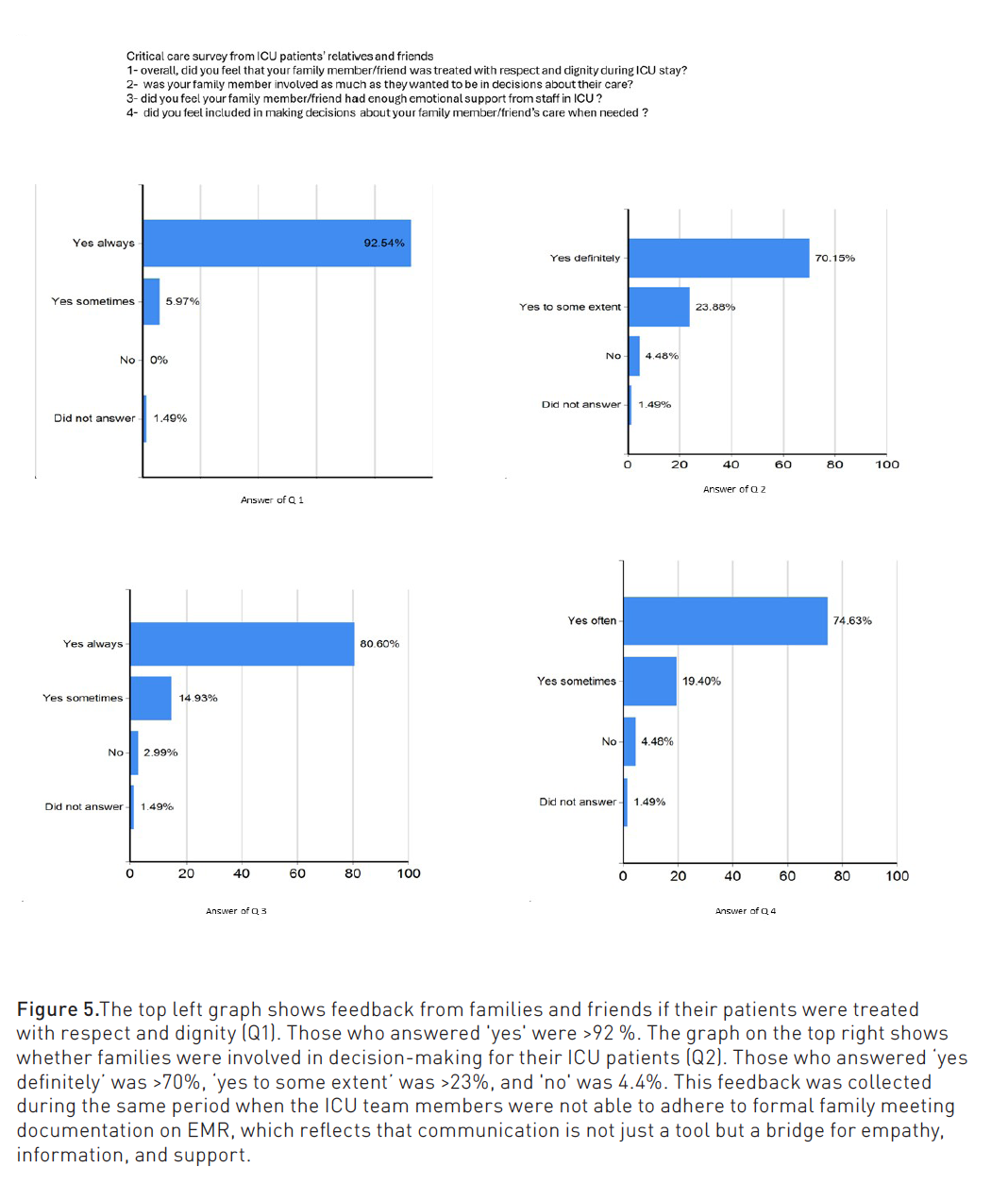
Current PCC efforts focus on patients’ personhood, patient-centred and family-centred communication, and interventions to improve family presence, support, and participation (Secunda et al. 2022).
How to Improve Family Meeting Communication and Documentation Skills in the ICU
In a multi-centre study, participation in an hour-long ICU communication and palliative skills workshop was associated with significant improvement in trainees' knowledge and attitudes toward family meetings (Munger et al. 2023).
Improving family meeting communication and documentation skills in the ICU involves a combination of training, practice, and a commitment to patient-centred care using variable tools. Communication skills improvement can be achieved via training programmes by attending workshops focused on communication skills in critical care settings, including simulated scenarios and role-playing exercises. Simulate family meetings by conducting regular role-playing sessions. This helps healthcare professionals practice effective communication in a controlled environment. Members of the healthcare team in communication training should attend interdisciplinary training, which fosters a multidisciplinary approach and improves coordination during family meetings.
Communication skills assessment and feedback together with continuous learning through literature, webinars, and educational resources would hugely improve family meeting communication. Consideration should be given to establish mentorship programmes where experienced members mentor those who are newer to family meetings. Conduct debriefing sessions after family meetings to discuss what went well and areas for improvement.
Specific training on empathy can enhance healthcare professionals' ability to understand and address the emotional needs of families. Utilising documentation skills improvement can be achieved via establishing clear protocols for family meetings, supplying standardised templates that guide healthcare professionals on what information to document during family meetings, training on documentation software if using EMR systems and ensuring proficiency in using the documentation software by providing training sessions. Using standardised language in documentation ensures clarity and reduces the risk of misinterpretation. Development of checklists for key points that need to be documented during family meetings ensures comprehensive documentation. Perform regular audits to identify areas for improvement with constructive feedback to the ICU team based on audit findings. Familiarise healthcare professionals with legal and ethical considerations in documentation to ensure accurate and compliant record-keeping.
Future Directions to Improve Family Meetings and Discussion in Intensive Care
As face-to-face communication with the family and visiting their patient was a huge challenge during the COVID-19 pandemic, the ICU staff has had to innovate and develop new communication strategies to address the barriers brought about by it. Elements such as ICU family liaison service, videoconferencing, hands-free communication devices, team roles and name labelswere usedas new strategies to improve communication in ICU during the pandemic (Chua 2022)
During the pandemic period, there were visitor restrictions, and few family meetings occurred in person. However, statistically significant fewer changes in patient goals of care occurred following video meetings compared to in-person meetings, providing support that limiting in-person meetings may affect patient care (Piscitello et al. 2021).
A U.K. survey studied ICU visiting and family communication during the COVID-19 pandemic. Significant changes were observed across NHS ICUs in how ICU teams interact with families. Many units adapted and moved towards distant and technology-assisted communication (Boulton et al. 2022).
Integration of technology such as telemedicine or virtual communication tools can enhance family meetings, mainly in remote healthcare delivery or during pandemics, as seen during the COVID-19 outbreak. Structured communication protocols may include guidelines for information disclosure, decision-making processes, and addressing emotional needs. Interdisciplinary training should focus not only on medical communication but also on emotional intelligence, empathy, and cultural competence.
Patient and family education about ICU can help facilitate more informed decision-making during family meetings. Earlier advance care planning discussions engage patients and families in conversations about their values, goals, and preferences regarding end-of-life care before crises occur.
Psychosocial support services, including counselling and chaplaincy, can help families cope with emotional challenges together with tools that facilitate shared decision-making between healthcare professionals and families. Decision aids and informational materials can help families understand complex medical information. Cultural competence training can help better understand and address the diverse needs and perspectives of families from different cultural backgrounds. Long-term follow-up and support can include post-ICU clinics or resources for coping with the aftermath of critical illness. Continuous quality improvement initiatives and regular feedback from families can be invaluable in refining communication practices.
Conclusion
This was an overview of an influential emotional narrative where the art of communication consolidates with the complexity of critical care. We advocate for the inclusivity of the entire ICU team, recognising the vital roles played by junior and senior doctors, alongside bedside nurses and interdisciplinary teams, in achieving patient-centred care. Communication is not just a tool but a bridge for empathy, information, and support, recapitulating through the corridors of uncertainty that characterise critical care. Despite the aspiration for structured family meetings, we urge an accurate understanding of the challenges within the ICU. Rather than a rigid adherence to routine formalities, we encourage flexibility, allowing healthcare providers to tailor their communication to the unique needs of patients and families. We found that it is all about the paradox of necessity and burden by underestimating the role of meticulous record-keeping and calling for a delicate balance that prevents administrative demands from eclipsing the human touch that defines pitying care.
Conflict of Interest
None.
References:
Boulton AJ, Jordan H, Adams CE et al. (2022) Intensive care unit visiting and family communication during the COVID-19 pandemic: A UK survey. J Intensive Care Soc. 23(3):293-296.
Chua CKZ (2022) New strategies to improve communication in the intensive care unit during the COVID-19 pandemic. Crit Care.;26(1):191.
Daly BJ, Douglas SL, O'Toole E et al. (2010) Effectiveness trial of an intensive communication structure for families of long-stay ICU patients. Chest. 138(6):1340-8.
Elkhonezy M, Setla S, Yusfu I (2023) Family meeting and discussion QI project April-May 2022, March-April 2023. King’s College Hospital NHS Foundation Trust. London, UK.
Gambhir HS, Goodrick S, Dhamoon A, Kaul V (2021) Impact of Structured and Scheduled Family Meetings on Satisfaction in Patients Admitted to Hospitalist Service. J Patient Exp. 8:23743735211002748.
Glajchen M, Goehring A, Johns H, Portenoy RK (2022) Family Meetings in Palliative Care: Benefits and Barriers. Curr Treat Options Oncol. 23(5):658-667.
Munger N, Konopka M, Chen E, Piscitello G (2023) Improving Quality of Family Meetings in the Medical Intensive Care Unit (FR205C). Journal of Pain and Symptom Management. 65(3): e275.
Nelson JE, Walker AS, Luhrs CA et al. (2009) Family meetings made simpler: a toolkit for the intensive care unit. J Crit Care. 24(4):626.e7-14.
Piscitello GM, Fukushima CM, Saulitis AK et al. (2021) Family Meetings in the Intensive Care Unit During the Coronavirus Disease 2019 Pandemic. Am J Hosp Palliat Care. 38(3):305-312.
Secunda KE, Kruser JM (2022) Patient-Centered and Family-Centered Care in the Intensive Care Unit. Clin Chest Med. 43(3):539-550.
Singer AE, Ash T, Ochotorena C et al. (2016) A Systematic Review of Family Meeting Tools in Palliative and Intensive Care Settings. Am J Hosp Palliat Care. 33(8):797-806.
Widera E, Anderson WG, Santhosh L et al. (2020) Family Meetings on Behalf of Patients with Serious Illness. N Engl J Med. 383(11):e71.
White DB, Angus DC, Shields AM et al. (2018) A Randomized Trial of a Family-Support Intervention in Intensive Care Units. N Engl J Med. 378(25):2365-2375.





















