Modern cancer care urgently demands new approaches. Lives are at risk, and an everincreasing number of cancer patients and complex examinations constitute more of the radiologist’s workload than ever before. Faster and more accurate diagnoses clearly support the end goal—better patient care—but precisely how to achieve this has proven elusive.We spoke with key opinion leaders from the Netherlands, Sweden, the UK, and the US to better understand the changes affecting radiology, and listened as they weighed in on the most important challenges and developments in the field.
Opportunities exist not only for radiology to improve traditional reading and reporting functions, but also, critically, to further the new collaborative paradigm that puts radiology at the forefront of diagnosis and patient management.
I invite you to read what these experts have to say.
 Mats Björnemo, Vice President of
Product Management at Sectra
Mats Björnemo, Vice President of
Product Management at Sectra
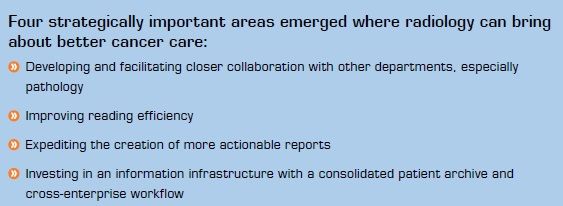
Area 1: Developing and facilitating closer collaboration with other departments, especially pathology
Integrated Diagnostics
Integrated diagnostics is a powerful new concept in cancer care. Professor Dr. Bruce A. Friedman, Emeritus Professor of Pathology at the University of Michigan Medical School, defined integrated diagnostics in a 2012 presentation as “the seamless collaboration among the diagnostic specialists, most notably pathologists and radiologists.” The goals of integrated diagnostics are straightforward: “To reduce the time and expense of diagnostic processes and provide clinicians with practical and actionable results.” These simple, recognizable goals come with tantalizing theorized rewards, including radically reducing the time from when a patient first walks into a practice to final diagnosis from weeks to days.
Professor Dr. Paul van Diest, head of the Department of Pathology at University Medical Centre Utrecht, talks about what integrated diagnostics could actually look like in practice:
No idea, but we are thinking about it all the time! This is something that we started about a year ago. We are starting to get a feeling that there is added value in bringing together diagnostic information from different laboratory disciplines and trying to make more sense of the data, rather than just looking at individual data from individual departments…it’s based on bringing diagnostic information together from different disciplines and trying to look for added value, so you need algorithms that mine these data and find patterns that point to diseases or diagnoses in a better way.
Will integrated diagnostics actually come to pass, or will it remain merely theoretical? Prof. van Diest answers: “It’s complicated, yes, but it’s gaining more and more momentum—more and more people are starting to talk about this in different parts of the world. The time is right to start doing this.”
Before integrated diagnostics can step out of the realm of theory, pathology and radiology must collaborate more closely than they do today. Streamlined communication of concepts and images between radiology and pathology facilitates the work of both departments. Prof. van Diest elaborates:
The first step in the chain is always imaging, and the second step is usually tissue or cellular diagnosis. Now there always needs to be feedback between the two disciplines: pathologists need to check whether the biopsy was representative by correlating back to the images, and radiologists like to know, if they made a diagnosis, that it’s correct; we like to see their results and they like to see ours. So the closer we bring them together, the lower the threshold is to look at each other’s results and images, provide the optimal feedback, and learn from each other’s results.
But is close physical proximity required to achieve improved feedback and learning? Not necessarily, according to Prof. van Diest, provided that both parties are using the same technology:
A certain proximity is not always that important; you can do a lot in a digital way. Sometimes you simply need to talk to people, and the optimal feedback is not just through ones and zeroes.Having said that, working digitally on both ends is quite important, because that tremendously facilitates access to data and images.
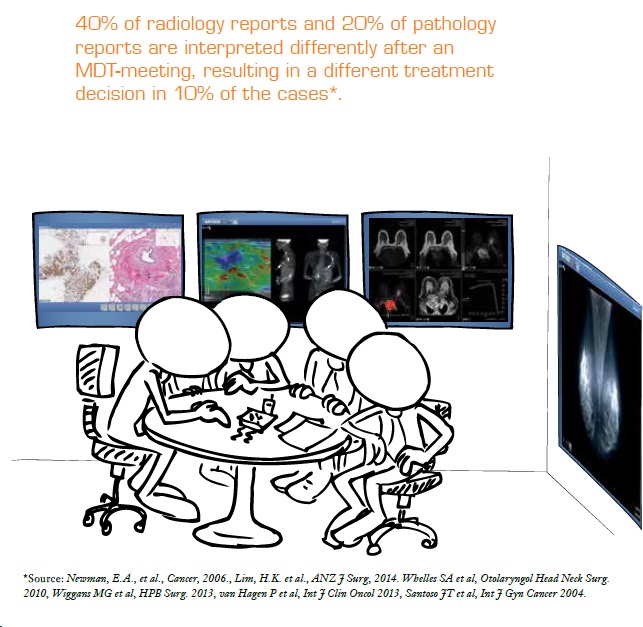
Having radiology and pathology on the same IT platform also reduces costs, not requiring separate systems. Beyond this, a shared system facilitates the MDT (multidisciplinary team meeting) — the pathologist can better participate with images on the same digital platform, ready for display and discussion.
Dr. Brendan Devlin, consulting radiologist since 1988 and former lead radiologist of NIPACS in Northern Ireland, comments: “One of the drivers for less-than-full pathology participation in the MDT has been the slowness of looking at individual slides, changing the slides, looking at a different image and changing the focus, etc.” He identifies a preferable scenario where “the opportunity to have instantly available digital images, bookmarked by the pathologist in advance, greatly facilitates their discussion.”
In the MDT, instead of just sending reports between departments or to the referring physician, the doctors involved come together to discuss their shared cancer patients. Meetings often include radiology, pathology, oncology, and surgery. Diagnoses and treatment plans are made with the combined expertise of the group, with the members acting in concert to develop patient pathways and treatment plans. Dr. Devlin elaborates: “We perform quality assurance and review what has already been done…it’s a good opportunity for professional discussion, which involves a degree of professional skepticism as well—everyone tests how robust your case is, how robust your diagnosis.” The best decisions for the patient are made based on all of the information and perspectives presented at that high-powered table.
Area 2: Improving reading efficiency
Screening programs, more complicated examinations, and an aging population have all contributed to the huge quantity of scans awaiting the radiologist’s review. Fortunately, tools that improve reading efficiency allow the radiologist to continue delivering the best possible care even in the face of increasing demands.
Dr. Devlin discusses how optimally efficient PACS software should function to improve reading efficiency:
I want to see that the PACS software radiologists are using is attuned to their needs, and facilitates what they have to do, almost in advance. The analogy would be the surgeon turning to the nurse of many years’ experience, looking for a particular instrument, and the nurse is standing there with the instrument in hand, ready for the surgeon to take…I would like to think of the software programs as knowing what we’re doing and facilitating what we’re doing, so that we can concentrate not on the process but rather on the diagnosis, which is really what we’re there for.
He provides specific examples of how software would facilitate reading:
Examinations may have, nowadays, up to a couple of thousand images, and we may have to review these images in multiple planes—MR systems have images in multiple planes that must be reviewed and collated—so the more we can have software that facilitates this, the better. Therefore, we’re looking at an increasing tendency to index lesions in cancer cases, and at anatomical registration, particularly for follow-up studies, so that we can more quickly review the very many more surveillance scans that are now being requested—so they can be done quickly, efficiently, and effectively.
Dr. Stamatia Destounis, Fellow of the American College of Radiology and Partner at Elizabeth Wende Breast Care in Rochester, New York, speaks about how certain reading and screening tasks are time-consuming but indispensable, and how the ability to perform all tasks at a single workstation improves efficiency:
It’s great to be able to interface with all our different modalities—MRI, ultrasound, and digital breast tomosynthesis—at one workstation. Reading the DBT images takes a long time, and so does performing a screening ultrasound examination, but these may provide more comprehensive care for the patient. I don’t think there are any radiologists who feel that we’re spending too much of our time on these additional studies; we’re happy to do them because we’re finding lesions that need to be found.

While software tools improve reading efficiency, they are useless if the PACS goes offline. Shannon Demay, PACS Administrator at Elizabeth Wende Breast Care, stresses this: “No downtime. We can’t afford to have our PACS go down for any reason—not an archive issue, or a pre-fetch issue, whatever issue—we can’t afford that.”
The number and complexity of the different systems and applications designed to save time can sometimes have the opposite effect. Demay addresses the need for seamless integration between different systems and applications:
We perform ultrasound, MRI, and biopsy procedures at our main facility; we see over 300 screening patients a day, and many stay for their results. But we also have three satellites where we perform mammograms and ultrasounds, and our radiologists are reading those studies remotely. Those patients may be waiting at the satellite for their results as well, so we need everything to work together seamlessly. The more integration we have with other systems and applications the better, because that means one less click for the doctors. Integration with our dictation and RIS systems helps doctors get through their worklists, through their day, and reduces distractions. We want to provide our radiologists with an environment where they can concentrate on reading, not on how to navigate from application to application.
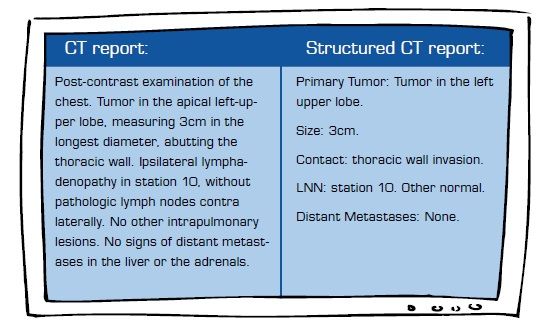
Area 3: Expediting the creation of more actionable reports
Rich and structured reports will allow the radiologist to provide more-actionable reports in less time, contributing even more to the entire patient-care team.
Rich reporting involves linking text in the diagnostic report to images or other data, which will make reports more actionable not only for clinicians but also for diagnosticians on subsequent review. Dr. Devlin describes how rich reporting will improve the communication of diagnostic certainty and key messages:
Starting at the basic level, I think it would be good if we could, while describing a particular lesion in the report, click on a word and link it to an image where we highlight a mass and change the view or color. The clinician who is later reading the report could click on the highlighted word and have the image pop up that best shows the abnormality. You try to make these reports more real for people…it all has to do with transforming and transmitting not just the diagnosis but also the diagnostic certainty level to the clinician. Some reports are quite long, so the more we can make sure that the actual messages are getting through, the better.
Dr. Devlin stresses that, though it sounds easy, successful implementation will require strong collaboration with clinicians: “It’s not that we can’t do it; it’s just not as easy as it might sound. It will demand a lot of work with clinicians to explore that reality.”
Structured reports will standardize both information layout and terminology, expediting report creation and presenting key information in an easier-to-read format for clinicians and other diagnosticians. But important considerations must be addressed before they will become common in radiology.
Dr. Devlin discusses how the structured report should be intuitively integrated with the image-reading process: “We have to make sure that it doesn’t actually damage the diagnostic process by making people focus too much on the mechanics of populating the fields of the report; it needs to be incorporated into the process of how the radiologist looks at the studies and not distract them from the essential intense scrutiny of the image findings.”
He goes on to identify an important benefit: “Structured reporting is good for ensuring that there are no gaps in the report. If the fields are there and they’re empty, then you know you probably haven’t said anything about the internal mammary nodes, for example, and that you probably should.”
Dr. Destounis comments on how breast care radiology has begun to adopt structured reporting:
“Several facilities have structured reporting, with systems that characterize lesions and give locations in the breast; doctors are able to just click on things, and the structured report works very well.” But dictation has long been a standard reporting practice, and to compete, structured reports must contain robust selection options to accommodate the nuance of what the radiologist
must express. Dr. Destounis explains:
There’s always the limitation of the drop-down box in how many choices you have, and when you’re dictating the lesion characteristics, the lesion location, or the exam, the available choices may not reflect exactly what you want to say. But I do know that many facilities and hospitals have structured reporting. If we get there, the hope is that the system is accommodating, trainable, and easy to use, and has a lot of choices. Because if I have to edit most of the report because the choices are not there, then it doesn’t really help me—it makes my life miserable. In a multi-radiologist practice, you’ll have to figure out how to agree on how the report should be structured, and what the most important features of an integrated dictation system are.
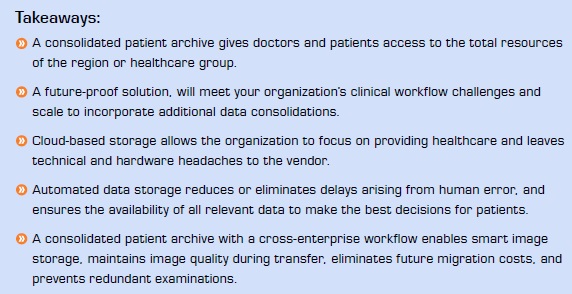
Area 4: Investing in an information infrastructure with a consolidated patient archive and cross-enterprise workflow
A consolidated patient archive provides access to all patient information, resulting in faster and more accurate diagnoses; a cross-enterprise workflow balances workloads and enables collaboration with other doctors and facilities when specialty expertise and second opinions are required. Both are pivotal to successful patient-centered cancer care.
NIPACS is a success story, a consolidated patient archive that provides all healthcare trusts in Northern Ireland access to patient images and reports. Dr. Devlin explains why automating the data storage process is beneficial:
”MDT preparation requires no human interaction in terms of sending CDs, or importing this, that, or the other. It’s all an intrinsic part of the design and configuration of the system. This saves a lot of time and improves the quality of decision-making: there is no incomplete decision-making made on the basis of incomplete data. Every time manual interaction is required, the possibility for delay increases, because things don’t happen. If the post doesn’t arrive, we can’t have the discussion.
That kind of thing is to be avoided at all costs, and a joined-up IT system achieves that.”
Dr. Devlin offers concrete proof of a consolidated, integrated archive’s success: A NIPACS MDT audit revealed that 100% of completed studies and authorized reports were available for review during the audit period.

The Stockholm VNA
Stockholm County represents one of the many healthcare providers and governing bodies now seeking to define visions of more patient-centered healthcare. Gustav Alvfeldt, Information Architect and Project Manager with the Stockholm County Council, spoke at a conference in August about their recent VNA rollout. A VNA, or vendor-neutral archive, is one option for enterprise clients looking for a consolidated patient record archive and workflow function.
Alvfeldt describes two overarching goals of their archive: “To avoid moving the patient around unnecessarily, and to use the resources of the region rather than only those of the hospital.” The Stockholm region contains the largest number of patients in Sweden, comprising 2.2 million inhabitants and 2000 healthcare providers. Five public and five private hospitals offer radiology
services, each with their own storage solutions, RIS and PACS, and together provide 1.6 million exams every year—and all will be connected through the VNA.
But the archive does not stop at centralizing radiology records. The VNA will also house and structure data from other departments to enable closer collaboration between them and support the county’s patient-oriented perspective. The county decided to implement a regional cloud-based VNA with built-in workflow intelligence to enable the efficient flow of images and information between all healthcare providers and ultimately improve the quality of care. Storing the archive in a cloud allows the county to focus on healthcare issues, leaving the vendor responsible for hardware maintenance and upgrades. “We wanted a VNA on steroids—not just storage, but intelligence around the storage…a total information infrastructure” says Alvfeldt.
Why is such an infrastructure important? Alvfeldt explains:
Patients today move around a lot more. For radiology this means that, before any given exam, the healthcare provider has to look for previous history from any of the other radiology departments in the region. In cancer care, having the complete patient history is crucial to making the correct diagnosis.
Doctors who know a patient’s complete history will not schedule that patient for unnecessary, redundant examinations if records of previous exams that suffice are already in the archive. Avoiding redundant exams is important for many reasons: expediting diagnosis and overall treatment, minimizing radiation exposure, reducing costs, and increasing overall patient satisfaction.