Inflammatory bowel disease (IBD) refers to chronic inflammation of all or part of the digestive tract. An article published in Surgical Clinics of North America lists the different radiologic techniques used for assessing IBD, including their key advantages and disadvantages.
Plain Radiographs
Plain abdominal radiographs can diagnose complications from IBD and should be a first imaging study in critically ill patients to evaluate for free intraperitoneal air. Perforation is identified by free air on an upright abdominal radiograph and should be ordered on any patient with acute onset abdominal pain.
Radiographs can be portable, are widely available, quick, painless, inexpensive, and have low radiation dose exposure. However, plain radiographs do not give much detailed information and cannot make a definitive diagnosis of IBD.
Contrast Radiologic Studies
Upper gastrointestinal series with small bowel follow through (SBFT) is useful in diagnosing stricturing Crohn’s disease; it also may diagnose fistulas related to Crohn’s disease. This procedure involves ingestion of a barium solution with subsequent radiologic imaging of the small intestine with fluoroscopy and radiograph.
Double-contrast barium enema is performed by inserting a tube in the rectum, instilling barium to outline the colon and rectum, then passing air through the tube to enhance the detail. Finally, multiple radiographs are obtained from different views. Disadvantages are preprocedure laxative preparation, discomfort from the test, and radiation exposure.
Computed Tomography
Abdominal CT scans can evaluate the entire gastrointestinal tract and other intra-abdominal organs that may exhibit extraintestinal manifestations of IBD. CT scanning is not a very sensitive test for detecting the mucosal abnormalities of mild or early ulcerative colitis.
CT enterography (CTE) uses oral contrast, intravenous contrast, and thin-cut multiplanar CT image acquisitions. It is useful for the evaluation of suspected or known Crohn’s disease and can detect dilation, obstruction, fistulas, and abscesses. These studies should be used when clinically indicated because there is increasing concern for repeated exposure to radiation from CT scanning performed in patients with IBD.
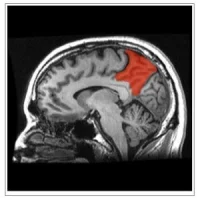
Magnetic Resonance Imaging
MRI and associated techniques, such as magnetic resonance enterography (MRE), are noninvasive, nonionising imaging modalities useful in evaluating intestinal and extraintestinal pathology, particularly in Crohn’s disease. MRI can significantly alter treatment plans from medical to surgical or vice versa.
MRI's chief strength is the ability to discern active inflammation from fibrosis in abnormal and thickened bowel. MRI is superior to other imaging modalities including CT in detecting perineal fistulas and sinus tracts with reported sensitivities of more than 80%.
MRI is significantly more expensive than plain radiograph, ultrasound, and CT. For the young IBD population, repeat imaging is common and MRI may therefore be cost-effective when balanced against the costs of complications from excess radiation exposure.
Ultrasound (US)
US for IBD requires high-frequency (5–17 MHz) linear array probes for the US machine, as these probes provide increased spatial resolution of the intestinal wall, which is essential for the assessment of wall diameter and wall layer discrimination. US does not provide a continuous and complete examination of the small and large bowel.
Small intestine contrast US is a new technique in which a nonabsorbable contrast solution (eg, polyethylene glycol 3350) is given orally before abdominal US. As with all US tests, its sensitivity and specificity highly depends on the experience of the operator and is not commonly performed at this time.
Capsule Endoscopy (CE)
CE provides state-of-the-art imaging of the mucosal lining of the intestines, particularly in the small bowel; CE is an expensive test but is outpatient, noninvasive, with no nonionising radiation. Patients swallow an approximately 11x26 mm pill that contains a video camera, LED lights, a radio transmitter, and battery. The pill transits through the small bowel in approximately 4 hours and colon in 24 to 48 hours before being excreted. Video images up to six frames per second are wirelessly transmitted to a portable device and downloaded to a computer.
Although CE has a clear role in the management of occult gastrointestinal bleeding, there is no established role of this new technology in the present management of IBD. Besides higher costs, additional limitation for CE includes its nontherapeutic capabilities. Future studies need to investigate the comparative effectiveness of CE with other imaging modalities.
Source and image credit: Surgical Clinics of North America
Plain Radiographs
Plain abdominal radiographs can diagnose complications from IBD and should be a first imaging study in critically ill patients to evaluate for free intraperitoneal air. Perforation is identified by free air on an upright abdominal radiograph and should be ordered on any patient with acute onset abdominal pain.
Radiographs can be portable, are widely available, quick, painless, inexpensive, and have low radiation dose exposure. However, plain radiographs do not give much detailed information and cannot make a definitive diagnosis of IBD.
Contrast Radiologic Studies
Upper gastrointestinal series with small bowel follow through (SBFT) is useful in diagnosing stricturing Crohn’s disease; it also may diagnose fistulas related to Crohn’s disease. This procedure involves ingestion of a barium solution with subsequent radiologic imaging of the small intestine with fluoroscopy and radiograph.
Double-contrast barium enema is performed by inserting a tube in the rectum, instilling barium to outline the colon and rectum, then passing air through the tube to enhance the detail. Finally, multiple radiographs are obtained from different views. Disadvantages are preprocedure laxative preparation, discomfort from the test, and radiation exposure.
Computed Tomography
Abdominal CT scans can evaluate the entire gastrointestinal tract and other intra-abdominal organs that may exhibit extraintestinal manifestations of IBD. CT scanning is not a very sensitive test for detecting the mucosal abnormalities of mild or early ulcerative colitis.
CT enterography (CTE) uses oral contrast, intravenous contrast, and thin-cut multiplanar CT image acquisitions. It is useful for the evaluation of suspected or known Crohn’s disease and can detect dilation, obstruction, fistulas, and abscesses. These studies should be used when clinically indicated because there is increasing concern for repeated exposure to radiation from CT scanning performed in patients with IBD.
Magnetic Resonance Imaging
MRI and associated techniques, such as magnetic resonance enterography (MRE), are noninvasive, nonionising imaging modalities useful in evaluating intestinal and extraintestinal pathology, particularly in Crohn’s disease. MRI can significantly alter treatment plans from medical to surgical or vice versa.
MRI's chief strength is the ability to discern active inflammation from fibrosis in abnormal and thickened bowel. MRI is superior to other imaging modalities including CT in detecting perineal fistulas and sinus tracts with reported sensitivities of more than 80%.
MRI is significantly more expensive than plain radiograph, ultrasound, and CT. For the young IBD population, repeat imaging is common and MRI may therefore be cost-effective when balanced against the costs of complications from excess radiation exposure.
Ultrasound (US)
US for IBD requires high-frequency (5–17 MHz) linear array probes for the US machine, as these probes provide increased spatial resolution of the intestinal wall, which is essential for the assessment of wall diameter and wall layer discrimination. US does not provide a continuous and complete examination of the small and large bowel.
Small intestine contrast US is a new technique in which a nonabsorbable contrast solution (eg, polyethylene glycol 3350) is given orally before abdominal US. As with all US tests, its sensitivity and specificity highly depends on the experience of the operator and is not commonly performed at this time.
Capsule Endoscopy (CE)
CE provides state-of-the-art imaging of the mucosal lining of the intestines, particularly in the small bowel; CE is an expensive test but is outpatient, noninvasive, with no nonionising radiation. Patients swallow an approximately 11x26 mm pill that contains a video camera, LED lights, a radio transmitter, and battery. The pill transits through the small bowel in approximately 4 hours and colon in 24 to 48 hours before being excreted. Video images up to six frames per second are wirelessly transmitted to a portable device and downloaded to a computer.
Although CE has a clear role in the management of occult gastrointestinal bleeding, there is no established role of this new technology in the present management of IBD. Besides higher costs, additional limitation for CE includes its nontherapeutic capabilities. Future studies need to investigate the comparative effectiveness of CE with other imaging modalities.
Source and image credit: Surgical Clinics of North America
References:
Morris MS, Chu DI (2015) Imaging for Inflammatory Bowel Disease. Surgical Clinics of North America. Published online: September 07, 2015.
DOI: http://dx.doi.org/10.1016/j.suc.2015.07.007
Latest Articles
healthmanagement, inflammatory bowel disease, MRI, CT, radiologic exams, Crohn's disease, ulcerative colitis
Inflammatory bowel disease (IBD) refers to chronic inflammation of all or part of the digestive tract. An article published in Surgical Clinics of North America lists the different radiologic techniques used for assessing IBD, including their key advantag