Ultrasound was not widely used outside the radiology suite or echocardiography laboratory 20 years ago. More recently, ultrasound has become common in emergency departments (EDs), perioperative care units, acute care floors in the hospital and in clinics. It is routinely used by physicians and advanced practice providers with variable training for diagnostic purposes and procedural guidance, often with little to no oversight by radiologists.
"It will be impossible to watch over every ultrasound examination performed at the point of care, which exacerbates the potential for patient harm with inadequately trained providers," says Amy E. Morris, MD, Division of Pulmonary and Critical Care Medicine, University of Washington. "It is therefore crucial that radiologists and POC ultrasound users work together to recognise its potential and its limitations, teach current and future care providers how to use it responsibly, and create an infrastructure that maximises quality of care while minimising patient risk."
This report by Dr. Morris, published in Current Problems in Diagnostic Radiology, provides a brief overview of key issues related to the increasing practice of point-of-care (POC) ultrasound: how it differs from complete ultrasound examinations, its potential to affect patient care, and issues of training, competency assessment, and ongoing quality assurance.
What POC Ultrasound Is, and What It Is Not
In any broad discussion of POC ultrasound, it is important to remember that it is a modality, not a specific application. The scope of practice differs by specialty. POC ultrasound examinations differ from complete studies in that they are:
Factors Driving the Increasing Use of POC Ultrasound
Smaller ultrasound machines, acceptance of ultrasound procedural guidance, and increasing exposure in medical school and graduate training programmes are driving the increasing use of procedural and diagnostic ultrasound at the bedside.
Machines capable of rendering high-quality images are smaller and less expensive, making it feasible for hospitals and clinics to purchase more units, and for providers to fit the machines into their inpatient and clinic rooms.
There is a well-established safety benefit of ultrasound guidance for several common invasive procedures such as thoracentesis and central venous catheter placement. In keeping with professional organisation guidelines and the Agency for Healthcare Research and Quality recommendations, in most institutions, it is considered the standard of care to place internal jugular venous catheters using real-time ultrasound needle guidance.
Recognising that POC ultrasound has the potential to be an important tool for diagnosis and clinical management, some medical schools have embraced the technology to augment anatomy lessons, and as an adjunct to the physical examination. In clinical clerkships, students at these and other medical schools are increasingly exposed to ultrasound at the POC, either as a planned part of their training or incidentally in clinical practice. In graduate medical education, ultrasound training is required and fairly standardised in emergency medicine residencies in the United States.
Utility of POC Ultrasound
POC ultrasound cannot supplant all aspects of the physical examination. However, if used appropriately, it is an extension of the physical examination, which can provide more rapid and accurate assessments.
One may question the ability of practitioners who are not radiologists, trained sonographers or cardiologists to accurately obtain and interpret ultrasound images. Review of the literature suggests that in appropriately narrow investigations, this is in fact the case. For example, internists with relatively brief transthoracic echocardiography training can obtain and interpret focused cardiac images to estimate left ventricular function with good accuracy, and focused ultrasound examinations performed by emergency medicine physicians have excellent sensitivity and specificity for detecting deep venous thrombosis and subcutaneous abscesses.
Less clear is how well these improved individual diagnostic findings translate into measurably more efficient clinical decision making and improved patient outcomes. These are more difficult end points to measure, and the evidence is far less robust, but there are some examples: the use of the focused assessment with sonography for trauma examination in the ED, which in patients with blunt trauma is associated with fewer CT scans, shorter hospital length of stay, and lower hospital bills.
Competency Assessment and Ongoing Quality Assurance
For physicians in practice, several national and international organisations offer training and certification in various aspects of POC ultrasound. The content and quality of educational offerings is not held to any universal standard, in part because the scope of practice varies by specialty. Outside emergency medicine, general consensus is emerging as to what should be included in the POC ultrasound skill set for providers in several areas of medicine, notably critical care.
In addition, prominent professional organisations have released consensus statements for certain examination types such as the focused assessment with sonography for trauma examination and focused transthoracic echocardiography, which helps to standardise educational content.
Establishing scope of practice and developing curricula are only the first steps toward assuring provider competence. Standards of assessment that encompass both examination performance and interpretation should be developed to ensure that providers are using POC ultrasound appropriately.
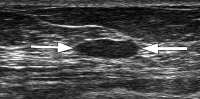
Both competence and ongoing quality assessment are hampered by the fact that unlike chest radiographs and CT scans, which have standard protocols such that they can be interpreted widely by providers who did not perform the examination themselves, POC ultrasound is by its nature individualised and brief. There are traditional cardiac views, and some anatomical structures are readily identified by their sonographic appearance, but some images will be difficult to interpret by someone who was not present at the time of the examination.
The essential advantage to POC ultrasound is that it is rapid, and in the urgent setting, it will not be practical to label every image in detail. Despite this limitation, for most common POC ultrasound examinations, it is possible to elucidate key required views, and users should be able to record their examinations for other providers to review and verify.
Summary
As ultrasound machines become smaller, indeed reduced to the size of mobile phone applications, medical students in the not-too-distant future may carry transducers next to the stethoscopes in their pockets. It would be impossible to disallow use of this technology altogether, and indeed inappropriate to do so, in light of the growing body of literature documenting its benefit.
As more providers use ultrasound at the POC, radiologists can take a leadership role in ensuring its effective use by collaborating to help shape standards of training and quality assurance.
Image Credit: Wikimedia Commons
"It will be impossible to watch over every ultrasound examination performed at the point of care, which exacerbates the potential for patient harm with inadequately trained providers," says Amy E. Morris, MD, Division of Pulmonary and Critical Care Medicine, University of Washington. "It is therefore crucial that radiologists and POC ultrasound users work together to recognise its potential and its limitations, teach current and future care providers how to use it responsibly, and create an infrastructure that maximises quality of care while minimising patient risk."
This report by Dr. Morris, published in Current Problems in Diagnostic Radiology, provides a brief overview of key issues related to the increasing practice of point-of-care (POC) ultrasound: how it differs from complete ultrasound examinations, its potential to affect patient care, and issues of training, competency assessment, and ongoing quality assurance.
What POC Ultrasound Is, and What It Is Not
In any broad discussion of POC ultrasound, it is important to remember that it is a modality, not a specific application. The scope of practice differs by specialty. POC ultrasound examinations differ from complete studies in that they are:
- Limited in scope, designed to achieve specific procedural aims (eg, direct the needle to the correct location) or answer focused questions (eg, does my patient have ascites?).
- Performed by the same care provider who will be using the information to direct immediate patient care management at the bedside.
Factors Driving the Increasing Use of POC Ultrasound
Smaller ultrasound machines, acceptance of ultrasound procedural guidance, and increasing exposure in medical school and graduate training programmes are driving the increasing use of procedural and diagnostic ultrasound at the bedside.
Machines capable of rendering high-quality images are smaller and less expensive, making it feasible for hospitals and clinics to purchase more units, and for providers to fit the machines into their inpatient and clinic rooms.
There is a well-established safety benefit of ultrasound guidance for several common invasive procedures such as thoracentesis and central venous catheter placement. In keeping with professional organisation guidelines and the Agency for Healthcare Research and Quality recommendations, in most institutions, it is considered the standard of care to place internal jugular venous catheters using real-time ultrasound needle guidance.
Recognising that POC ultrasound has the potential to be an important tool for diagnosis and clinical management, some medical schools have embraced the technology to augment anatomy lessons, and as an adjunct to the physical examination. In clinical clerkships, students at these and other medical schools are increasingly exposed to ultrasound at the POC, either as a planned part of their training or incidentally in clinical practice. In graduate medical education, ultrasound training is required and fairly standardised in emergency medicine residencies in the United States.
Utility of POC Ultrasound
POC ultrasound cannot supplant all aspects of the physical examination. However, if used appropriately, it is an extension of the physical examination, which can provide more rapid and accurate assessments.
One may question the ability of practitioners who are not radiologists, trained sonographers or cardiologists to accurately obtain and interpret ultrasound images. Review of the literature suggests that in appropriately narrow investigations, this is in fact the case. For example, internists with relatively brief transthoracic echocardiography training can obtain and interpret focused cardiac images to estimate left ventricular function with good accuracy, and focused ultrasound examinations performed by emergency medicine physicians have excellent sensitivity and specificity for detecting deep venous thrombosis and subcutaneous abscesses.
Less clear is how well these improved individual diagnostic findings translate into measurably more efficient clinical decision making and improved patient outcomes. These are more difficult end points to measure, and the evidence is far less robust, but there are some examples: the use of the focused assessment with sonography for trauma examination in the ED, which in patients with blunt trauma is associated with fewer CT scans, shorter hospital length of stay, and lower hospital bills.
Competency Assessment and Ongoing Quality Assurance
For physicians in practice, several national and international organisations offer training and certification in various aspects of POC ultrasound. The content and quality of educational offerings is not held to any universal standard, in part because the scope of practice varies by specialty. Outside emergency medicine, general consensus is emerging as to what should be included in the POC ultrasound skill set for providers in several areas of medicine, notably critical care.
In addition, prominent professional organisations have released consensus statements for certain examination types such as the focused assessment with sonography for trauma examination and focused transthoracic echocardiography, which helps to standardise educational content.
Establishing scope of practice and developing curricula are only the first steps toward assuring provider competence. Standards of assessment that encompass both examination performance and interpretation should be developed to ensure that providers are using POC ultrasound appropriately.
Both competence and ongoing quality assessment are hampered by the fact that unlike chest radiographs and CT scans, which have standard protocols such that they can be interpreted widely by providers who did not perform the examination themselves, POC ultrasound is by its nature individualised and brief. There are traditional cardiac views, and some anatomical structures are readily identified by their sonographic appearance, but some images will be difficult to interpret by someone who was not present at the time of the examination.
The essential advantage to POC ultrasound is that it is rapid, and in the urgent setting, it will not be practical to label every image in detail. Despite this limitation, for most common POC ultrasound examinations, it is possible to elucidate key required views, and users should be able to record their examinations for other providers to review and verify.
Summary
As ultrasound machines become smaller, indeed reduced to the size of mobile phone applications, medical students in the not-too-distant future may carry transducers next to the stethoscopes in their pockets. It would be impossible to disallow use of this technology altogether, and indeed inappropriate to do so, in light of the growing body of literature documenting its benefit.
As more providers use ultrasound at the POC, radiologists can take a leadership role in ensuring its effective use by collaborating to help shape standards of training and quality assurance.
Image Credit: Wikimedia Commons
References:
Morris AE (2014) Point-of-Care Ultrasound: Seeing the Future. Curr Probl
Diagn Radiol 2015;44:3–7. DOI:
http://dx.doi.org/10.1067/j.cpradiol.2014.05.012
Latest Articles
Ultrasound, Radiology, echocardiography, point-of-care, POC, emergency medicine
Ultrasound was not widely used outside the radiology suite or echocardiography laboratory 20 years ago. More recently, ultrasound has become common in eme...