Radiology has always been a field that is focused on imaging and equipment and the specific output of these tools. However, at the very heart of this specialty is the satisfaction of the patient in terms of the right test, shorter exam times, better diagnostic, reduced exposure to radiation and so on.
There is no doubt that the science of imaging has progressed tremendously. However, from the days of the unknown "x-ray" in 1895 to the new and exciting tools used in human imagery today, the patient has always remained a bi-product for this segment. Passivity was always expected from them. Hold still, follow directions, wait for results etc. were all part of the proper patient behaviour.
Today, patients are no longer passive. With the introduction of patient surveys, online communication and information technology, patients have been provided the opportunity to say what they want and what they need. Patients are now more vocal and more aggressive in voicing their concerns about privacy, identity theft and costs.
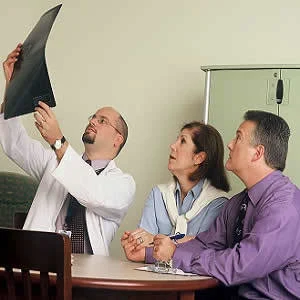
Patients today want to understand their imaging exam and want more accessibility to radiologists. By doing so, they are better able to deal with findings from their imaging exam and are more positive about the results. Therefore, adding a thank you note with the report or a postprocedural summary or information about the radiology team are all little measures that can enhance patient understanding and improve patient satisfaction.
The wave of the future will thus involve more patient engagement and demand for more information. It will involve interactive participation in care. For radiologists, this means that they will need to pay attention to the whole patient experience and will need to be more patient friendly. This collaborative approach offers many benefits and can help address patient concerns in real time and improve communication between patients and radiologists.
“At
the end of the day, every one of us is going to be a patient,” says Andrea Borondy Kitts, MS, MPH, a mechanical engineer executive turned lung cancer patient advocate. “We are vulnerable. But the reality is that all of the life
experiences and expertise we have are still there and part of our
person.”
Therefore, it is important to understand a patient's background, have a more interactive relationship with them and improve collaboration to optimise patient care.
Source: Diagnostic Imaging
Image Credit: Wikimedia Commons