Duke Medicine researchers have created a 3D map of the human brain stem at an unprecedented level of detail using MRI technology. In a report published in Human Brain Mapping, the researchers say the new 3D model would be useful to brain surgeons treating conditions such as tremors and Parkinson’s disease with deep brain stimulation (DBS).
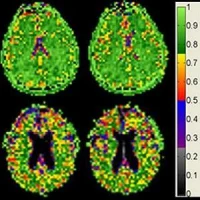
Many neurosurgeons currently rely on lower resolution CT and MRI scans and geographic coordinates relative to the planes of the brain to guide them when placing electrodes into the thalamus. What they are targeting is a circuit called the dentatorubrothalamic tract or DRT (shown as an X-shaped pathway in the accompanying image).
Surgeons must often remove and reinsert electrodes and test frequencies to find the spots inside the thalamus where, for instance, the electric current subdues the hands of a patient with debilitating tremors. This indirect targeting is the standard of care for DBS, which involves risk. Moving an electrode requires another pass through delicate tissue, and complications from DBS can include haemorrhage, seizure, or memory problems.
The new 3D map "will potentially help us reach the optimal target the first time. It could eliminate trial and error and make the surgery safer,” says neurosurgeon Nandan Lad, MD, PhD, director of the Duke NeuroOutcomes Center and one of the study's authors.
The map was produced from a 10-day scan of a healthy donor’s postmortem brain stem in a 7-Tesla MRI system, and then converted into a 3D model that can be proportionally scaled to fit a person’s unique brain anatomy using a high-performance computing cluster.
“These images are 1,000 times more detailed than a clinical MRI. You can actually see the nerve fibres in the brain, how they’re crossing, and the subtleties of contrast between gray and white matter in the brain far beyond what a clinical scan could offer,” explains senior author G. Allan Johnson, director of the Duke Center for In Vivo Microscopy where the brain stem was scanned.
To test the accuracy of the 3D model, the Duke team conducted a retrospective study of 12 patients who had already been treated successfully for tremors using DBS. The team used the 3D model to predict the best placement for the electrodes in each patient. The predictive computer model and the actual successful electrode placements correlated for 22 of 24 electrodes in the dozen patients, the team says, adding that they will soon begin a prospective study using the model to guide DBS surgery.
The team will also pursue high-resolution imaging of other circuits in the brain, brain stem and spinal cord to develop new treatments for other conditions.
Source and image credit: Duke Medicine
Many neurosurgeons currently rely on lower resolution CT and MRI scans and geographic coordinates relative to the planes of the brain to guide them when placing electrodes into the thalamus. What they are targeting is a circuit called the dentatorubrothalamic tract or DRT (shown as an X-shaped pathway in the accompanying image).
Surgeons must often remove and reinsert electrodes and test frequencies to find the spots inside the thalamus where, for instance, the electric current subdues the hands of a patient with debilitating tremors. This indirect targeting is the standard of care for DBS, which involves risk. Moving an electrode requires another pass through delicate tissue, and complications from DBS can include haemorrhage, seizure, or memory problems.
The new 3D map "will potentially help us reach the optimal target the first time. It could eliminate trial and error and make the surgery safer,” says neurosurgeon Nandan Lad, MD, PhD, director of the Duke NeuroOutcomes Center and one of the study's authors.
The map was produced from a 10-day scan of a healthy donor’s postmortem brain stem in a 7-Tesla MRI system, and then converted into a 3D model that can be proportionally scaled to fit a person’s unique brain anatomy using a high-performance computing cluster.
“These images are 1,000 times more detailed than a clinical MRI. You can actually see the nerve fibres in the brain, how they’re crossing, and the subtleties of contrast between gray and white matter in the brain far beyond what a clinical scan could offer,” explains senior author G. Allan Johnson, director of the Duke Center for In Vivo Microscopy where the brain stem was scanned.
To test the accuracy of the 3D model, the Duke team conducted a retrospective study of 12 patients who had already been treated successfully for tremors using DBS. The team used the 3D model to predict the best placement for the electrodes in each patient. The predictive computer model and the actual successful electrode placements correlated for 22 of 24 electrodes in the dozen patients, the team says, adding that they will soon begin a prospective study using the model to guide DBS surgery.
The team will also pursue high-resolution imaging of other circuits in the brain, brain stem and spinal cord to develop new treatments for other conditions.
Source and image credit: Duke Medicine
Latest Articles
healthmanagement, MRI, 3D, deep brain stimulation, DBS, DBS surgery
Duke Medicine researchers have created a 3D map of the human brain stem at an unprecedented level of detail using MRI technology.