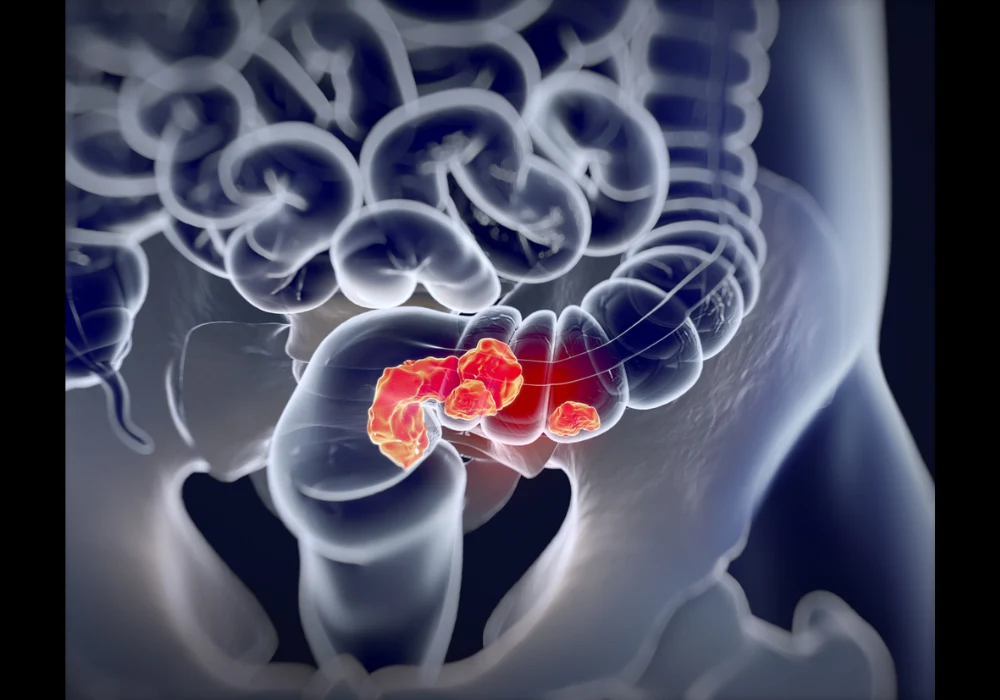
Achieving clear resection margins is critical in the surgical management of locally recurrent rectal cancer (LRRC), as it is closely linked to improved overall and disease-free survival. However, the feasibility of complete resection varies widely depending on tumour location and biological behaviour. A recent retrospective study published in Radiology: Imaging Cancer aimed to assess how pelvic compartment involvement and MRI-derived tumour characteristics influence surgical outcomes and long-term prognosis in LRRC. By using a standardised MRI reporting checklist, researchers examined the relationships between anatomical and morphological tumour features, resectability and oncologic outcomes, offering insights that may enhance patient selection for curative surgery.
Pelvic Involvement and Resection Outcomes
Among the 328 patients included, MRI revealed that central compartment involvement was most common and associated with the lowest risk of positive resection margins. In contrast, lateral and posterior compartment involvement significantly increased the likelihood of R1 resections. Specifically, central recurrences—predominantly located at the anastomosis—were associated with better resectability, likely due to their positioning within soft tissue and relative distance from vital structures. Lateral tumours were the most challenging to resect completely, often due to their proximity to neurovascular structures and pelvic bones.
Must Read: MRI Criteria to Distinguish SRUS from Rectal Cancer
Detailed anatomical analysis further refined these observations. Within the anterior compartment, ureter and prostate involvement were linked to higher odds of incomplete resection, while in the posterior and lateral compartments, factors such as cranial extension to the sacrum or lumbar spine, vascular invasion and obturator muscle involvement were predictive of positive margins. Multivariable analysis identified ureter involvement, periosteal or bony cortex invasion and vascular infiltration as significant contributors to incomplete resections. These findings highlight the importance of comprehensive anatomical assessment in preoperative planning.
Prognostic Implications of Compartment Involvement
Survival outcomes also differed according to compartment involvement. Central compartment involvement correlated with improved overall and disease-free survival, whereas lateral involvement was associated with significantly worse outcomes. These trends persisted even after controlling for resection margin status. The findings suggest that lateral recurrences may be biologically more aggressive, not merely technically more difficult to remove. While anterior compartment involvement was linked to decreased disease-free survival, posterior involvement did not show a significant independent effect on either survival metric.
The better prognosis associated with central recurrences may reflect their aetiology. These tumours often arise at the anastomotic site and may result from surgical technique issues rather than aggressive tumour biology. In contrast, lateral recurrences may stem from missed or untreated pelvic lymph node involvement, indicating a more systemic and resistant disease process. This reinforces the view that anatomical location offers indirect insight into tumour biology, influencing both surgical strategy and anticipated outcomes.
Tumour Morphology and Biological Behaviour
MRI-derived morphological features also influenced surgical and oncologic outcomes. Tumour size had an inverse relationship with resectability, as larger tumours were more likely to result in positive margins. Mucinous tumours were associated with better resectability, while solid tumours were linked to increased risk of incomplete resection. Tumour border type proved especially relevant: well-defined tumours were more likely to be completely resected, whereas spiculated or irregular borders correlated with a higher risk of positive margins.
When examining survival outcomes, fibrotic tumours were the only type significantly associated with reduced disease-free survival. Tumours with irregular borders trended towards worse prognosis, although not reaching statistical significance. These features may serve as indicators of poor biological behaviour, with therapy-resistant or invasive tendencies. Among patients with R0 resections, neither fibrotic nor solid tumours retained a significant association with disease-free survival, suggesting that complete resection may partially counterbalance adverse morphology.
MRI evaluation of tumour morphology therefore provides an important layer of prognostic information. While size and resectability are important, features such as fibrosis and border definition may reveal deeper insights into tumour behaviour. Incorporating these findings into routine reporting can support multidisciplinary decision-making, enabling more informed patient selection and surgical planning.
The study demonstrated that MRI-derived tumour characteristics, including compartment involvement and morphological features, significantly influence resectability and survival outcomes in patients with LRRC. Central compartment involvement and well-defined tumours are associated with improved prognosis, while lateral involvement, fibrotic structure and spiculated or irregular borders are linked to worse outcomes. These findings support the standardisation of MRI reporting in LRRC to facilitate better prognostication and patient selection. Multidisciplinary teams may benefit from incorporating detailed anatomical and morphological assessments into treatment planning, helping to balance surgical ambition with oncologic benefit. Further prospective research is needed to validate these findings and refine the prognostic use of MRI in this patient population.
Source: Radiology: Imaging Cancer
Image Credit: iStock