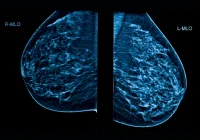
Minimally invasive image-guided biopsy is central to diagnosing suspicious breast lesions while reducing complications, costs and cosmetic impact compared with diagnostic surgery. Multiple techniques are in routine use—fine-needle aspiration (FNA), core-needle biopsy (CNB) and vacuum-assisted biopsy (VAB)—and can be performed under ultrasound (US), mammography or tomosynthesis with or without contrast-enhanced mammography (CEM), and magnetic resonance imaging (MRI). Variation in practice persists, particularly where evidence comparing techniques and imaging combinations is limited. An international expert panel used a structured RAND/UCLA process to articulate practical, consensus-based recommendations covering first-line technique selection by imaging modality, adaptations for specific US-visible lesion types and sizes and re-biopsy strategies for radiological–pathological discordance and high-risk findings. The guidance aims to standardise decision-making and support accurate, efficient diagnosis.
Standard Approaches by Imaging Modality
US guidance is the default first-line route for tissue sampling when the lesion is visible, reflecting procedural ease, real-time targeting and patient comfort. In this context, CNB is generally preferred for masses larger than 5 mm, balancing diagnostic accuracy with cost and a low complication profile. FNA is discouraged for diagnostic work-up of solid US-visible lesions because it cannot provide histology, does not distinguish in situ from invasive disease and does not yield receptor status, however, it remains useful for drainage where indicated.
When lesions are visible only on mammography, tomosynthesis or CEM, VAB is recommended as the first choice. Larger sample volumes improve sensitivity and specificity and reduce underestimation compared with FNA or CNB. For extensive calcifications, sampling separate foci with two VAB passes is advised to characterise disease extent and limit underestimation. CNB is a fallback only when VAB is not available or feasible.
For MRI-only lesions, VAB is likewise recommended. If VAB cannot be performed, MRI-guided localisation with surgical excision is the alternative. In selected contexts, and depending on suspicion and clinical factors, short-interval imaging follow-up may be acceptable where neither CEM- nor MRI-guided biopsy is available and the result would not alter immediate management.
Technique Choice for Ultrasound-Visible Lesions
Technique selection under US depends on lesion size, composition and the sampling goal. For small masses under 5 mm, VAB is preferred because CNB carries a meaningful sampling miss risk at this size. As these lesions are often completely removed during VAB, marker placement in the biopsy cavity is essential to ensure future localisation if needed.
For masses over 5 mm, CNB is usually recommended, with VAB reserved for selected circumstances. Simple or complicated cysts in symptomatic patients warrant FNA for relief; asymptomatic cysts do not require sampling. Complex cystic and solid lesions with small solid components under 5 mm favour VAB due to underestimation risk and potential non-visualisation of the solid part after collapse, again, marker placement is important. Where the solid component exceeds 5 mm, no consensus was reached: options include CNB when safe and technically straightforward, VAB, extended vacuum-assisted biopsy (EVAB) or surgical excision. If the lesion collapses during sampling, a post-biopsy marker should be placed.
Must Read: Standardising Ultrasound-Guided Biopsy in Gynaecological Oncology
Small intraductal masses under 5 mm are best approached with VAB, acknowledging the likelihood of complete removal with this method, CNB is an alternative but risks underestimation and requires adequate sampling. For architectural distortion visible on US—typically a non-mass pattern—VAB is recommended regardless of size to mitigate underestimation across the diverse benign and malignant causes, EVAB can be considered upfront to secure diagnostic certainty. For calcifications visible on US, VAB is advised, with specimen radiography to verify calcifications in the samples and mandatory post-biopsy marker placement.
For axillary or intramammary lymph nodes, the panel did not reach consensus between FNA and CNB. Where proof of metastatic involvement alone suffices, FNA can be used, but when results may influence treatment selection or require molecular characterisation, CNB is preferred due to higher sensitivity and richer histology. Abscesses should be drained by FNA using an adequately large needle and combined with antibiotics, with US monitoring of resolution, recurrent cases may warrant CNB to exclude alternative pathology. CNB is recommended for mastitis not responding to antibiotics, with cores from the inflamed area or multiple areas if diffuse, to exclude inflammatory breast cancer.
Re-biopsy, High-risk Findings and Procedure Objectives
Re-biopsy is indicated after insufficient sampling, radiological–pathological discordance or when a lesion requires removal. Clarifying the procedural intent is critical. VAB is a diagnostic technique, EVAB is defined as a VAB procedure using a higher tissue yield to obtain a definitive histological diagnosis, targeting roughly 4 g of tissue while not aiming for complete excision. Vacuum-assisted excision (VAE) is a therapeutic intent procedure intended to remove the lesion entirely.
For proven benign lesions under 3 cm that a patient wishes to have removed, VAE is recommended, with surgical excision as backup. For lesions over 3 cm, either surgical excision or VAE can be considered based on lesion location and breast size. In radiological–pathological discordance after CNB, most panellists favoured VAB or EVAB over repeat CNB, except where a missed fibroadenoma is suspected and retargeting may resolve the mismatch. After discordant VAB, EVAB, VAE or surgery are all options, no consensus was reached, and choices should reflect risk and feasibility.
For lesions of uncertain malignant potential (B3), approaches vary by subtype and prior technique. Incidental findings of lobular neoplasia or flat epithelial atypia on CNB commonly led to recommendation for EVAB, with VAB or VAE as alternatives depending on histology, after VAB, follow-up may suffice or EVAB can be considered. Complex sclerosing lesions, including radial scars, generally warrant EVAB after an initial CNB or VAB, if negative, follow-up is appropriate. Papillary lesions larger than 1.5 cm, with or without atypia, and smaller papillary lesions with atypia should undergo EVAB, small papillary lesions without atypia may be followed. For phyllodes tumours found on CNB or VAB, surgical excision is advised, although VAE can be considered for small benign tumours under 2 cm. For ductal carcinoma in situ (DCIS) diagnosed on CNB or VAB, surgical excision is recommended, additional imaging or VAB sampling is indicated only if it would alter treatment planning.
The consensus recommendations prioritise US guidance where feasible, reserve VAB for lesions visible only on mammography, tomosynthesis, CEM or MRI and tailor US-guided technique choice to lesion size and composition. Clear differentiation between diagnostic EVAB and therapeutic VAE helps align sampling with clinical objectives, particularly in discordant results and B3 lesions. Standardising selection of imaging modality and needle technique, the guidance supports accurate diagnosis, reduces underestimation and provides pragmatic pathways for re-biopsy, offering clinicians a coherent framework to inform everyday breast biopsy decisions.
Source: Insights into Imaging
Image Credit: iStock