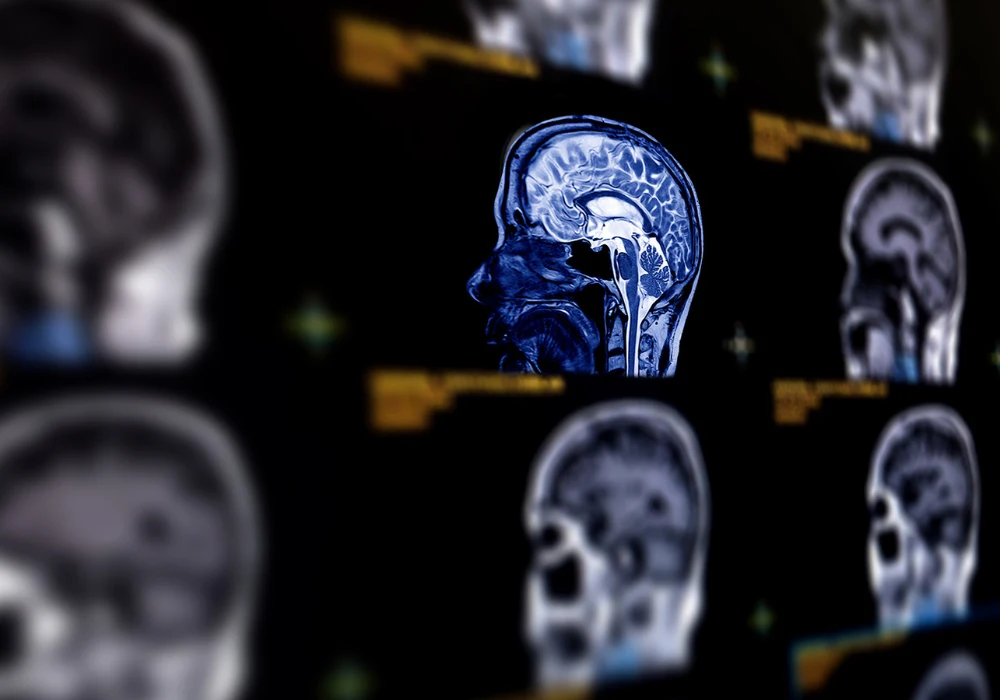
Neuroimaging can summarise how a brain compares with typical ageing by estimating a brain age and contrasting it with a person’s actual age. The difference, known as the brain age gap (BAG), indicates whether a brain appears older or younger than expected on a given scan type. BAGs drawn from structural, molecular, functional and diffusion imaging each highlight different aspects of brain health. Across neurodegenerative conditions, higher BAGs have been linked to worse cognition, greater likelihood of progression and, in early reports, treatment response. Used alongside established tests, BAGs can support risk assessment, guide trial enrolment and help track change over time when their strengths and limits are understood.
How Brain Age Is Estimated
Brain age models learn age patterns from scans of healthy adults, then predict an individual’s brain age from their imaging features. Approaches range from traditional regressions to modern neural networks. After validation, a BAG is computed by subtracting chronological age from predicted brain age. Because predictions can drift toward the average, simple corrections are applied so results are not biased by being very young or very old. Accuracy is assessed with standard errors and correlation measures to ensure the model generalises beyond the training set.
Must Read: Tracking Ageing from a Single Brain Scan
Each imaging modality offers a slightly different lens. Structural MRI captures patterns of atrophy spread across the brain rather than focusing on a single region. Molecular imaging can reflect metabolic change or protein accumulation before obvious shrinkage appears. Functional measures capture how networks communicate, and diffusion imaging is sensitive to microstructural integrity. Calculating BAGs per modality acknowledges that ageing is multifactorial and that no single scan explains it all.
What Different Modalities Reveal
Structural MRI–based BAGs are the most developed. They relate to cognitive performance, increase with clinical progression and distinguish people who later move from mild cognitive impairment to Alzheimer-type dementia. They integrate brain-wide patterns and can separate those at higher risk more effectively than single-region volumes. Elevated structural BAGs have also been described in Parkinson disease, multiple sclerosis and selected amyotrophic lateral sclerosis cohorts, aligning with disability in some contexts and with cognitive rather than motor change in others.
Molecular imaging adds a mechanistic angle. Ageing is associated with metabolic decline and protein pathology that PET or SPECT can detect. Early findings show metabolic BAGs align with structural BAGs yet may track non-Alzheimer trajectories in some people with mild cognitive impairment, while tau-based age patterns appear to follow symptom burden within the Alzheimer continuum. Evidence for amyloid and dopamine tracers is still limited, but the rationale for broader testing is strong.
Functional and microstructural signals extend coverage. Resting-state fMRI and electroencephalography reveal functional departures linked to Alzheimer disease with smaller effects in related syndromes. Sleep electroencephalography–based BAGs align with worse cognition and with modifiable risk factors, echoing the early role of sleep disturbance. Diffusion MRI–based BAGs may rise before obvious impairment, including in individuals who later develop mild cognitive symptoms, pointing to early white matter involvement.
Implications for Treatment and Trials
Baseline BAGs can relate to outcomes. People with milder structural BAGs have shown better response to symptomatic treatments despite starting with similar cognitive scores, and brain stimulation results have mapped more closely to BAG than to raw volume or symptom severity. This suggests BAGs capture diffuse vulnerability not obvious on a single clinical measure.
Intervention sensitivity is emerging. Structural BAGs have shifted following disease-directed therapy in multiple sclerosis, and short-term physiological or behavioural challenges have produced transient changes that then normalise. Longer lifestyle interventions have moved BAGs in a direction consistent with healthier ageing. Although these observations span different contexts, they point to BAGs as promising secondary or exploratory endpoints in trials that already collect imaging for eligibility, stratification or monitoring.
Adoption demands care. BAGs reflect training data, preprocessing choices, image quality and head motion, and they can vary across scanners. They index deviations from healthy ageing patterns rather than the full biology of disease, and they do not directly measure upstream processes that lack robust imaging markers. Interpreting BAGs alongside clinical evaluation and established biomarkers is therefore essential, with modality choice matched to the decision at hand.
Brain age gaps provide a concise, individualised view of how a brain diverges from expected ageing. Structural MRI currently offers the strongest evidence, while molecular, functional and diffusion imaging add complementary insights that may surface early change. Used with attention to technical limits and in context with recognised biomarkers, BAGs can support risk stratification, monitoring and evaluation of therapeutic impact across neurodegenerative conditions.
Source: Journal of Nuclear Medicine
Image Credit: iStock