Low-field magnetic resonance imaging (MRI) gains renewed attention as advances in hardware and software narrow the performance gap with high-field systems. Historically sidelined for lower signal-to-noise ratio and reduced spatial resolution, low-field platforms now integrate optimised magnet designs, improved radiofrequency coils and AI-enabled reconstruction that together raise diagnostic utility. The appeal extends beyond image quality. Lower purchase prices, simpler siting and reduced maintenance are unlocking access in settings where conventional 1.5-T or 3.0-T scanners are impractical. Reduced susceptibility artefacts near metal, quieter operation and larger or open geometries add patient-centred advantages. Low-field MRI shifts from a niche alternative to a practical option for acute neuroimaging, neonatal care, musculoskeletal assessments and selected cardiac applications, while remaining clear about its current limitations.
Must Read: LowGAN Enhances Portable MRI for MS Imaging
Access, Portability and Patient Experience
Cost and infrastructure have long constrained MRI availability. Lower magnet mass and weaker fringe fields can trim transport and installation demands, while sealed or cryogen-light designs reduce the burden of quench pipes and boil-off. Compact footprints decrease room requirements and energy use, widening feasibility in resource-limited hospitals and outpatient sites. These factors, taken together, are making MRI procurement and operation more attainable where budgets and buildings previously stood in the way.
Portability is a defining advantage. The emergence of bedside brain imaging has brought cross-sectional diagnostics into intensive care and emergency environments, avoiding risky transfers for unstable patients. Feasibility projects have extended the concept to in-home imaging and pre-hospital pathways, showing how mobile low-field units can be embedded in vehicles or integrated into stroke networks. These deployments support scenarios where speed, continuity of care and environmental constraints limit access to fixed suites.
Safety and comfort also favour lower fields in specific contexts. Lower specific absorption rate and reduced magnetic forces can help in patients with certain implants, though risk assessment remains essential and heating effects can still occur. Reduced susceptibility improves imaging near metal, supporting postoperative and orthopaedic follow-up. Quieter operation and larger bores or open configurations can ease claustrophobia and have been associated with better tolerance and fewer terminated scans, which matters in paediatrics and for anxious patients. Together, these factors strengthen the case for placing scanners closer to the point of care and tailoring services to patient needs.
Clinical Utility Across Key Pathways
Neuroimaging is a central use case. Earlier low-field platforms were hampered by long acquisition times and muted contrast, but AI-enabled reconstruction now shortens exams and improves conspicuity. Protocols refined for low field have approached higher-field diagnostic performance for stroke, hydrocephalus, intracranial haemorrhage, tumours and demyelinating disease. Portable ultra-low-field systems have shown high concordance with standard measures for lesion burden and mass effect, supporting decision-making when conventional MRI or computed tomography access is limited. These developments are expanding neuroimaging capacity across emergencies, intensive care and ward-based pathways.
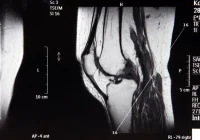
Musculoskeletal imaging is another area of traction where siting flexibility and cost matter. Dedicated extremity and compact systems paired with optimised coils and advanced reconstruction have delivered acceptable image quality for common joint and soft tissue questions. Metal artefact reduction at low field adds practical value in arthroplasty surveillance, postoperative reviews and sports injuries. While the smallest or most subtle findings may still favour high-field systems, the balance of image quality, comfort and operational simplicity is driving broader adoption in outpatient and community settings.
Neonatal and paediatric imaging benefit from low noise, tailored hardware and bedside access. Point-of-care systems designed for neonatal intensive care allow cross-sectional assessment without transport, complementing cranial ultrasound and reducing logistical risk. For selected cardiac applications, 0.55-T imaging shows promising feasibility signals. Lower susceptibility and specific absorption rate can improve stability around cardiac devices and reduce off-resonance artefacts in cine sequences. Volumetric measures have correlated closely with higher-field references in small cohorts, supporting the case for targeted use where implant burden is high or access is constrained. Commercial offerings now span neonatal point-of-care units, compact whole-body scanners with large bores and sealed cryogen subsystems, head-and-neck systems situated outside conventional suites and mobile ultra-low-field platforms aimed at bedside brain imaging or procedure guidance.
Technical Constraints and Evolving Solutions
Constraints remain intrinsic to lower fields. Signal-to-noise ratio scales with field strength, often necessitating longer acquisitions or more aggressive reconstruction. Diffusion imaging on portable platforms can be vulnerable to electromagnetic interference and gradient limitations, and fat suppression is harder because fat-water frequency separation narrows as field strength drops. Sequence optimisation, Dixon-based techniques, compressed sensing and parallel imaging are helping to stabilise image quality and shorten scans, but careful protocol design remains essential.
Certain clinical tasks still favour higher fields. Applications demanding very high spatial fidelity, complex gating or rapid vascular dynamics can expose low-field boundaries, including reduced temporal resolution and electrocardiographic distortion in some cardiac contexts. Upright and ultra-low-field systems have shown limited concordance for specific endovascular follow-up questions. Even so, rapid progress is evident. Deep learning reconstruction is improving effective resolution and artefact handling, while innovations in magnet engineering, including self-shielded designs, are pushing portability further. As coils, gradients and reconstruction continue to mature, the usable envelope of low-field imaging is expanding across body regions and clinical questions.
Low-field and portable MRI are transitioning into credible clinical options where access, workflow and patient comfort are decisive. Evidence supports targeted use in acute brain assessment, neonatal care, musculoskeletal practice and selected cardiac scenarios, with distinct strengths around portability, siting and metal artefact behaviour. Important caveats persist, including lower signal-to-noise ratio, diffusion and fat-suppression challenges at very low fields and residual limitations for demanding vascular or cardiac tasks. Continued gains in magnet engineering, coil design and AI-driven reconstruction are positioning low-field MRI as a pragmatic complement to high-field systems, extending service reach while containing cost and infrastructure demands.
Source: European Radiology Experimental
Image Credit: iStock