Artificial intelligence is already reshaping healthcare by enhancing diagnostic capabilities, particularly in imaging. In vascular medicine, where diseases such as abdominal aortic aneurysms (AAA), carotid artery disease and peripheral artery disease affect over 200 million people worldwide, AI-guided imaging offers a powerful opportunity to improve detection and treatment. Yet despite the promise of these technologies, their integration into routine clinical practice remains limited. Much of this is due to persistent challenges in commercialisation. Financial constraints, regulatory barriers and difficulties with implementation and guideline integration continue to prevent AI from reaching its full potential. Understanding how to navigate these issues is crucial to translating innovations into clinical and operational impact.
From Technical Feasibility to Clinical Utility
One recent example demonstrates both the promise and the complexity of turning AI innovation into practice. A deep learning algorithm was developed to support nurses without ultrasound training in performing AAA screening. With a cohort of 184 patients at an outpatient cardiology clinic, the algorithm guided nurses in real time on probe placement and automatically detected and measured the aorta. The median patient age was 72, and many had comorbidities such as hypertension, diabetes and heart disease. Results showed 100% sensitivity and 97.8% specificity, with the majority of scans achieving diagnostic quality comparable to physician-performed ultrasounds. The average scan time was just 37 seconds.
Must Read: Comparing Open- and Closed-Source LLMs for Radiology Error Detection
This tool could address systemic issues in AAA screening, which is currently underutilised due to shortages of imaging specialists, particularly in low-resource settings. Most AAAs are discovered incidentally rather than through targeted screening, despite guideline recommendations. Undetected AAAs can rupture, with mortality rates reaching 80%. The AI-enhanced solution offers a scalable and efficient method for expanding screening access and improving outcomes. Nevertheless, even such validated tools face barriers to widespread use. They require oversight from trained clinicians, further validation across diverse settings and most importantly, a structured path to commercialisation involving regulatory approval, reimbursement and integration into clinical guidelines.
Blueprints for Successful Deployment
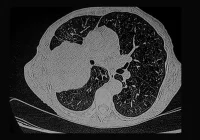
The journey from algorithm to clinical adoption can be informed by the experience of companies that have successfully commercialised medical AI. One such company, founded in the United States in 2016, initially focused on neurological care but expanded to cardiovascular and oncologic domains. It developed FDA-cleared AI algorithms capable of analysing CT scans, ECGs and echocardiograms to support clinical decisions related to cerebral aneurysm, intracranial haemorrhage, stroke, pulmonary embolism and AAA. These tools are now generating more than $40 million (€36.8 million) in annual revenue.
Several strategic elements underpinned this success. A multidisciplinary team of clinicians and engineers worked collaboratively, developing algorithms validated in peer-reviewed publications. From the outset, the company implemented standardised medical device development practices within a quality management system and sought ISO certification. Importantly, they aligned development with regulatory requirements early in the process. Health technology assessments were employed to demonstrate potential cost savings, such as $11 million (€10.1 million) annually in the UK for AI-assisted stroke detection. These evaluations helped secure over $290 million (€266.8 million) in private investment.
In addition, the company actively engaged with healthcare payers. By aligning with clinical guidelines and reimbursement mechanisms, it ensured that its tools were not only approved but also financially viable and clinically supported. This case highlights the importance of parallel progress in technical, regulatory and commercial domains, all of which must align to achieve meaningful adoption.
Challenges Hindering Commercial Scale
While successful models exist, most AI tools do not reach widespread clinical use. A significant obstacle is the funding gap between validation and deployment. Academic grants often cease once a prototype is validated, but further investment is needed for product refinement, compliance work and scale-up. Private investors play a vital role in this stage but are generally risk-averse, particularly with technologies targeting niche markets like AAA, which affects fewer than 5% of the global population. To attract funding, developers must present compelling business cases that clearly quantify clinical value, economic savings and revenue potential.
One advantage in such niche markets is reduced competition. While heart disease and cancer technologies face crowded landscapes, tools for vascular conditions offer investors opportunities to dominate smaller but underexploited areas. Furthermore, the same AI frameworks can often be extended to related pathologies, such as carotid or peripheral artery disease, which also rely on imaging for diagnosis. A systematic health technology assessment can help establish cost-effectiveness and sociocultural value, strengthening the case for adoption.
Beyond investment, regulatory approval is a major hurdle. The process differs across jurisdictions and products targeting international markets must accommodate multiple frameworks. In the United States, approval often follows the FDA’s 510(k) pathway, which requires demonstrating equivalence to an existing, approved device. Regulatory planning should begin at the earliest stages and continue through development. Consultation with regulatory experts and programmes, such as the FDA’s Q-Submission service, is essential to avoid costly rework later. Good Machine Learning Practice principles, jointly endorsed by agencies in the US, UK and Canada, provide a guide for quality development.
Reimbursement is another critical step. Most AI tools do not have dedicated billing codes and securing them requires engagement with insurers, clinicians and patient groups. Modifying established codes to accommodate new technologies involves advocacy, negotiation and evidence. In some cases, support from professional societies is instrumental in establishing reimbursement. Without this, even approved tools may be financially inaccessible.
Integration into clinical practice guidelines represents the final step toward legitimacy. These guidelines influence whether physicians adopt new tools. For AAA screening, different organisations issue conflicting recommendations. The Society for Vascular Surgery includes broader screening criteria than the US Preventive Services Task Force, which limits its recommendation to men aged 65–75 with a smoking history. Wider adoption of AI tools that reduce screening costs could help harmonise these guidelines and encourage use by both specialists and generalists.
Artificial intelligence is already enhancing vascular imaging, but its potential will remain unrealised unless more AI tools transition from research prototypes to integrated clinical systems. Achieving this requires a clear commercialisation roadmap that addresses funding, regulatory approval, reimbursement and clinical guideline alignment. Successful examples show the importance of multidisciplinary collaboration, early regulatory planning and sustained investment. Developers must align technical innovation with business and policy strategy to overcome systemic barriers. By embedding these considerations from the beginning, AI developers and health leaders can ensure that impactful technologies are deployed where they are needed most.
Source: npj digital medicine
Image Credit: iStock