HealthManagement, Volume 25 - Issue 3, 2025
A machine learning model predicting patient adherence to medication shows potential to enhance Clinical Homecare services in the UK. Tailored, early support improves adherence and reduces medicines wastage, with even modest gains delivering significant cost savings. Scaling these interventions nationally could save millions annually and ease NHS pressures while supporting more patients with chronic conditions at home.
Key Points
- Enhanced Clinical Homecare improves medication adherence compared to standard support.
- Early intervention further increases adherence among patients with chronic conditions.
- A machine learning model accurately predicts future non-adherence risk.
- Adherence prediction enables more targeted and timely support for patients.
- Small adherence gains can lead to large national savings on medicines wastage.
Introduction
The cost of medicines wastage in the UK is substantial, affecting both healthcare providers and the pharmaceutical industry. An estimated €116–€930 million worth of dispensed NHS medicines are discarded annually, equivalent to about €1.2 in every €29 spent on primary care and community pharmaceutical products (Webb 2014). This issue is amplified by a 61.7% increase in prescription items dispensed in England between 2006 and 2024, reaching 1,112.9 million items in 2023/2024 (NHSBSA 2024).
Broadly speaking, medicines wastage arises from various factors. Patient-related (intrinsic) causes include both intentional and unintentional non-adherence (Hazell and Robson 2015), while system-related (extrinsic) factors include inadequate pharmacy reviews and oversized prescription packs (Alhomoud 2020; Hazell and Robson 2015).
Interestingly, the method by which patients receive their medication—such as traditional NHS delivery routes versus Clinical Homecare services—can also affect the extent and risk of medicines wastage. Clinical Homecare is believed to reduce wastage by minimising losses from missed appointments or damage during patient transit (NCHA 2024).
With nearly half of the UK population affected by long-standing health conditions (45.7% of men and 50.1% of women) (ONS 2022), Clinical Homecare services are becoming increasingly important. These services support the initiation and ongoing adherence to treatment for patients with chronic illnesses who would otherwise need frequent visits to hospitals or pharmacies. They typically involve the delivery of specialist medicines for self-administration at home, along with appropriate support and training from a Clinical Homecare provider (Zanni et al. 2024; NCHA 2024).
Given the rising prevalence of chronic conditions, it is beneficial for the health system to explore ways of both enhancing the capacity of Clinical Homecare, so that more chronic disease patients can be supported, and increasing the effectiveness of these services in improving medication adherence. Doing this can have a significant downstream effect on medicines wastage.
Experts in machine learning have long argued that predicting non-adherence risk in real time—using tools like motion sensors for rehabilitation, real-time measurement of medication dosing and wearable devices—can allow for the efficient and proactive implementation of interventions to support adherence in patients with chronic diseases (González-Villanueva L et al. 2013; Zheng Y et al. 2014).
Methodology
This study has the following objectives:
- to provide evidence that medication adherence improved when Clinical Homecare services are enhanced (ie tailored) and deployed early in a patient’s treatment journey;
- to outline a theoretical basis for further improvements in adherence if Clinical Homecare services are underpinned by medication adherence prediction;
- to build on existing research and estimate the additional reduction in medicines wastage that result from using adherence prediction to guide early deployment, service tailoring and expanded Clinical Homecare capacity.
Evidence of Improved Adherence with Proactive and Tailored Clinical Homecare
Analytical Approach
The study dataset consisted of anonymised registration data from patients receiving support from a UK-based Clinical Homecare provider (HealthNet Homecare). The processed data included a range of anonymised parameters such as primary diagnosis, therapy area, medication type, service status, socioeconomic and demographic details (eg age and gender), delivery confirmation records and information on the frequency and channels of patient-provider communication. Medication supply was calculated daily for each patient. The dataset covers the period from December 2023 to May 2025 and includes data from 185,387 patients.
The processed data is used to calculate each patient’s Proportion of Days Covered (PDC)—the percentage of days a patient has access to their medication relative to the prescribed schedule—on a daily basis. Periods of inactivity are excluded from the analysis, and PDC values are then binarised as either "Adherent" or "Nonadherent." A patient is considered adherent (PDC80) if, during the past 18 months of active engagement, they had access to medication on 80% or more of days. The calculation also accounts for stockpiling, with additional medication deliveries added to the patient’s existing supply.
The dataset is then further segmented to distinguish between patients receiving:
- Standard Clinical Homecare service: medication dispensing and delivery, with or without self-administration training; or
- Enhanced Clinical Homecare service: the standard service plus tailored, ongoing support to help maintain adherence.
The dataset is then filtered into these sub-datasets, with the proportion of adherent patients being calculated for each service level.
We also examined whether enrolling patients earlier in an Enhanced Clinical Homecare Service improves adherence. To do this, we reviewed patient registration data to determine when individuals were referred to Enhanced Nurse Support, then identified the date of their first interaction—defined as the point at which the patient accepted the service after being informed of the referral.
Results
We observed that a relatively higher proportion of the patients receiving Enhanced Clinical Homecare Support were adherent (PDC >80%) compared to those who are receiving just the Standard Clinical Homecare support: 90.73% vs 89.04% (an increase of 1.69%). This demonstrates the utility of the Enhanced/Tailored Clinical Homecare Support. Furthermore, the patients on the Enhanced service received more deliveries on average, across this 18-month timeframe.
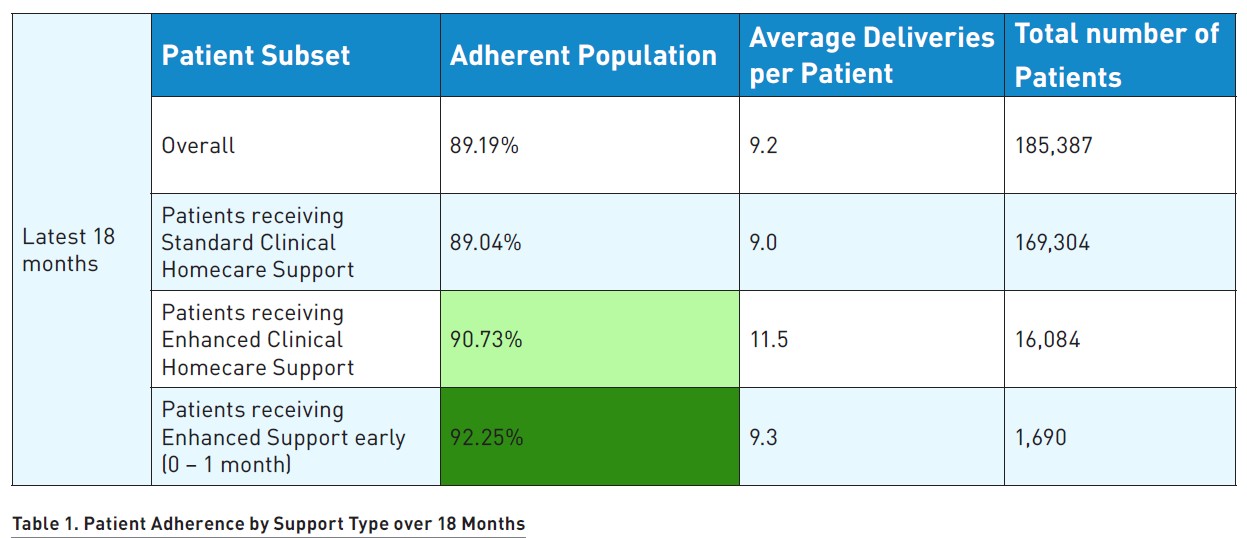
The results also show that early access to Enhanced services—within the first month after referral—leads to a further increase in adherence, reaching 92.25% (a 1.52% improvement). This supports the view that providing timely support early in the treatment journey benefits long-term medication adherence.
Theoretical Basis for Adherence Improvement through Medication Adherence Prediction
A Machine Learning Model Predicting Medication Adherence
The Machine Learning (ML) model used in this study is a Convolutional Neural Network (CNN) designed to identify patients at highest risk of future non-adherence, defined as having access to medication on fewer than 80% of days in a given month. Medication stock levels are calculated using delivery confirmation timestamps alongside prescription duration, assuming patients take their medication as prescribed. The model also accounts for stockpiling—common among chronic disease patients—by adding newly delivered quantities to any existing, unconsumed supply (Al Zoubi et al. 2021; Cameron et al. 2021).
Daily tracking of each patient’s medication stock enables the calculation of their Proportion of Days Covered (PDC) on a monthly basis. If a patient’s PDC falls below 80% for a given month, they are classified as nonadherent, allowing the data to be binarised into “adherent” and “nonadherent” categories. The PDC80 threshold is widely accepted as a standard for measuring adherence (Galozy and Nowaczyk 2020; Sayed et al. 2023; Kumamaru et al. 2018).
To train the predictive model, each patient’s most recent month on service is used as the target variable, with preceding medication supply data serving as input features for both training and inference. The resulting model achieved a high Area Under the Curve (AUC) of 98.6% and an adherence prediction accuracy of 92.8% (Malin et al. 2024).
Using Predicted Insight to Support Early Deployment and Better Tailoring of Clinical Homecare Services
Predicting a patient’s risk of nonadherence allows for the proactive implementation of support strategies aimed at preventing declines in adherence. Research shows that the factors influencing adherence are highly individualised and can change over time, even within the same patient (Kvarnström et al. 2021; Chauke et al. 2022). Therefore, any intervention designed to address poor adherence must account for the dynamic and patient-specific nature of these risk factors.
We have already established that adherence among chronic disease patients receiving Clinical Homecare support improves when that support is tailored—and improves even further when it is introduced early in the treatment journey. Therefore, any tool that enables earlier deployment and more personalised tailoring of support can further strengthen the impact of Clinical Homecare on medication adherence.
The machine learning model outlined earlier is specifically designed to support this goal. By providing early insight into which patients are most at risk of non-adherence, it allows care providers to both prioritise timely intervention and customise support based on individual risk profiles (HealthNet Homecare 2023).
This viewpoint on the positive impact of proactive action on adherence is consistent with findings from other research studies (Patel 2022; Stuurman-Bieze AG et al 2014) that have examined the benefits for long-term adherence by starting interventions early in the patient’s treatment and management journey.
Using Predicted Insight to Improve Clinical Homecare Capacity
Predicted insights from a machine learning model can help optimise decision-making around which Clinical Homecare service an NHS physician should refer a patient to (HealthNet Homecare 2023). With greater clarity on each patient’s individual risk of non-adherence, clinicians can make more informed decisions about who is likely to benefit most from specific types of homecare support.
The UK Clinical Homecare market is reportedly growing by over 20% each year (NCHA 2025), with at least 500,000—and potentially over 600,000—patients already receiving consultant- or nurse-led care in community settings (NCHA 2024; 2025). Given that an estimated 6.8 million people in the UK may be eligible for Clinical Homecare, and that most patients prefer treatment at home over hospital or outpatient care (NCHA 2024), demand for these services is expected to rise significantly.
Assessing suitable candidates for different levels of Clinical Homecare support can often be a time-consuming process, especially for chronic disease patients who self-administer their medication in the community, where prescribing physicians have limited visibility into long-term adherence patterns. Reducing the administrative burden associated with triaging and referring patients to Clinical Homecare can help providers respond more effectively to the growing demand for tailored or enhanced services.
Forecasted Medicines Wastage Savings through Clinical Homecare Enhanced with Adherence Prediction
Analytical Approach
The baseline impact of Clinical Homecare on medicines wastage is drawn from a 2024 study by the National Clinical Homecare Association (NCHA) (NCHA 2024), which employed the following data sources and methodology:
NHS/Hospital Delivery Data: The average number of medicine deliveries per patient in a hospital setting was estimated using the NHS’s 28-day repeat prescribing policy (Regal Chambers Surgery 2024). Under this policy, patients typically receive 13 deliveries annually, reflecting a monthly prescription cycle. This figure was used as a reference point to compare delivery frequency and related costs between hospital-based and Clinical Homecare models. The estimate is grounded in standard NHS prescribing procedures and medication dispensing guidelines.
Cost of Wasted NHS Medicine: Estimates for the cost of wasted NHS medicines were derived from a 2015 NHS England report focused on reducing pharmaceutical waste (NCHA 2024). These figures were adjusted for inflation from 2010 to 2021 using Bank of England data, applying an average annual inflation rate of 1.25%. This adjustment ensures that the estimates reflect current economic conditions and allows for more accurate analysis and comparison with recent data.
Prescription Data: The annual number of prescription items dispensed was taken from the NHS Prescription Cost Analysis for England 2022/23, which recorded a total of 1.18 billion items (NHSBSA 2024). This dataset offers a detailed overview of medication volumes across England and serves as a key reference point for assessing medication usage patterns and the potential scale of waste.
Average Cost of Clinical Homecare Medicine per Delivery: According to the 2024 NCHA report (NCHA 2024), the average cost of medicines per delivery in a Clinical Homecare setting is £1,350 (€1,575). This figure is a key metric for evaluating the economic efficiency of Clinical Homecare compared to hospital-based medication delivery.
NHS Total Spend: In the 2021/22 fiscal year, NHS expenditure on prescribing costs in hospitals and the community in England totalled £17.8 billion (€20.77 billion), as reported by the NHS Business Services Authority (NHSBSA 2023). This provides a macro-level context for understanding the financial scale of NHS medication costs and the potential impact of shifting to or expanding Clinical Homecare services.
Based on the above analysis, the NCHA identified the following:
- improved medication adherence in patients receiving Clinical Homecare compared to those not receiving it;
- the average number of medicine deliveries per patient within the Clinical Homecare setting;
- cost savings from reduced medicines wastage per delivery in Clinical Homecare.
Building on these findings, our study estimated how national-level cost savings could change if the improvements in adherence observed in our study population were replicated across the wider Clinical Homecare sector.
Results
National Results from the NCHA Study
According to the National Clinical Homecare Association (NCHA), the cost savings from reduced medicines wastage in Clinical Homecare are estimated at £2.13 (€2.49) per delivery, as a result of a 7.5% improvement in patient adherence (NCHA 2024).
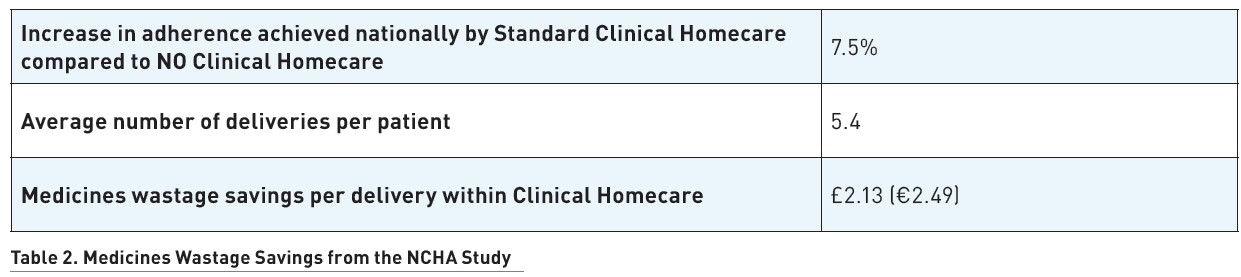
ith an average of 5.4 deliveries per patient annually, this equates to £11.55 (€13.48) in savings per patient each year. When applied to the estimated 600,000 patients currently receiving Clinical Homecare support in the UK, the total annual savings from reduced medicines wastage would be approximately £6.9 million (€8.1 million).
Assumptions on the Impact of Optimising National Clinical Homecare through Medication Adherence Prediction
As shown in Table 1, Enhanced Clinical Homecare support led to a 1.69% increase in adherence, with early implementation yielding an additional 1.52%—a combined improvement of 3.21% over standard support.
Assuming a conservative national rollout of a machine learning model that predicts patients at risk of poor adherence, thereby enabling earlier intervention and more tailored support, we estimate that only a fraction of this improvement may be replicated at scale. If the model achieves just a quarter (0.8%) or half (1.6%) of the observed adherence gain nationally, it will still result in substantial additional cost savings due to reduced medicines wastage.
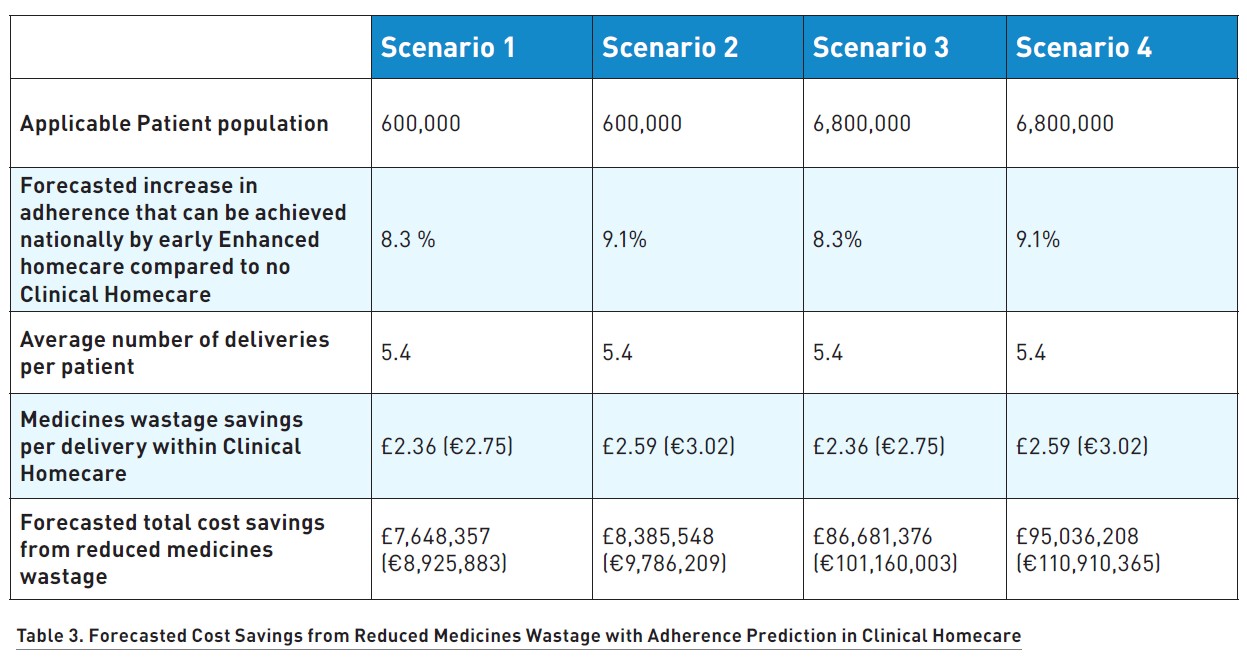
Table 3 outlines four forecast scenarios:
- The first two scenarios assume that medication adherence prediction replicates either a quarter (0.8%) or half (1.6%) of the 3.21% improvement observed through early and tailored Enhanced Clinical Homecare (as shown earlier). When added to the 7.5% adherence improvement previously reported by NCHA, the total projected improvements become 8.3% and 9.1%, respectively. These are applied to the current estimated national total of 600,000 patients receiving Clinical Homecare in the UK.
- The remaining two scenarios apply the same projected improvements (8.3% and 9.1%) to a hypothetical national expansion in which all 6.8 million patients who are eligible for Clinical Homecare receive such support.
Discussions & Conclusions
The results of this study address two issues that have been subject of active debate by a number of healthcare stakeholders: the impact of Clinical Homecare on medication adherence, and efforts to reduce medicines wastage. Providing comprehensive, wraparound support for patients with chronic conditions can meaningfully increase their likelihood of adhering to prescribed treatments.
Organisations such as the UK Steering Group on Improving the Use of Medicines have previously undertaken extensive reviews to explore how patients can be better supported in taking their medication as prescribed—recognising the dual benefit of improved health outcomes and greater value for the NHS (DOH 2012). However, no single approach can fully address the complex and variable nature of medication non-adherence. What works for one patient—or at one point in time—may not work for another (Patel 2021). For this reason, tailored interventions are likely to be more effective, particularly when introduced early, while patients remain more engaged. These interventions must also be adaptable, responding to changes in individual risk over time.
Furthermore, previous studies (NCHA 2024) have shown that Clinical Homecare can reduce the likelihood of prescriptions going unused due to early cancellations, patient non-adherence or damage during transit. Building on this, we argue that optimising Clinical Homecare through the use of adherence prediction could further amplify its impact on reducing medicines wastage.
Importantly, our findings demonstrate that even small increases in adherence—achieved through early, tailored support enabled by predictive tools—can lead to meaningful cost savings. This highlights how sensitive medicines wastage costs are to adherence rates and underscores the potential value of integrating adherence prediction into Clinical Homecare services.
In parallel, the UK NHS has begun adopting predictive analytics to support medication adherence. For instance, NHS Digital’s AI Knowledge Repository and OpenSAFELY platform are designed to enable large-scale predictive modelling across millions of records (Nab et al. 2024). Additionally, the INTENSE Trial Project—launched through a collaboration between NHS England, NIHR and academic partners—aims to improve adherence in patients with Type 2 diabetes using structured pharmacist support, AI-personalised SMS reminders and digital monitoring tools (Al-Jabr et al. 2021). These initiatives, whether used independently or alongside Clinical Homecare, may provide complementary benefits across a wide range of patient populations.
In conclusion, medication adherence prediction using machine learning models—such as the one presented in this study—has the potential to strengthen the benefits of Clinical Homecare in three ways:
- by expanding service capacity to support more patients;
- by enabling earlier interventions for those at risk of non-adherence; and
- by allowing for more personalised and responsive care.
Further research will be needed to assess the long-term impact of such tools on both adherence and medicines wastage at scale.
Conflict of Interest
Ejike Nwokoro, Ben Malin, Daniela Zanni and Joshua Hinton are employees of HealthNet Homecare.
References:
Al‑Jabr H, Farmer A, Bhattacharya D (2021) New community pharmacy‑led trial service aims to improve medication adherence in people with diabetes mellitus. Pharmaceutical Journal, 306 (7948).
Al Zoubi S, Gharaibeh L, Jaber H et al. (2021) Household Drug Stockpiling and Panic Buying of Drugs During the COVID-19 Pandemic: A Study From Jordan. Front Pharmacol, 12.
Alhomoud F (2020) Don't Let Medicines Go to Waste -A Survey-Based Cross-Sectional Study of Pharmacists' Waste-Reducing Activities Across Gulf Cooperation Council Countries. Front Pharmacol, 11:1334.
Cameron E, Moss S, Keitaanpaa S et al. (2021) Pharmacists’ experiences of consumer stockpiling: insights from COVID-19. J Pharm Pract Res, 51:464–471.
Chauke GD, Nakwafila O, Chibi B et al. (2022) Factors influencing poor medication adherence amongst patients with chronic disease in low-and-middle-income countries: A systematic scoping review. Heliyon, 8(6):e09716.
DOH (2012) Action Plan for Improving the Use of Medicines and Reducing Waste. Department of Health and Social Care Guidance.
Galozy A & Nowaczyk S (2020) Prediction and pattern analysis of medication refill adherence through electronic health records and dispensation data. Journal of Biomedical Informatics, 112
González-Villanueva L, Cagnoni S & Ascari L (2013) Design of a Wearable Sensing System for Human Motion Monitoring in Physical Rehabilitation. Sensors, 13:7735–7755.
Hazell B & Robson R (2015) Pharmaceutical waste reduction in the NHS. NHS Business Services Authority Report No 1/2015.
HealthNet Homecare (2023) How HealthNet are driving patient safety and positive experience through cost-effective Clinical Homecare. HealthNet Homecare Reports.
Kumamaru H et al. (2018) Using Previous Medication Adherence to Predict Future Adherence; Journal of Managed Care & Specialty Pharmacy, 24(11).
Kvarnström K, Westerholm A, Airaksinen M et al. (2021) Factors Contributing to Medication Adherence in Patients with a Chronic Condition: A Scoping Review of Qualitative Research. Pharmaceutics, 13(7):1100
Malin B, Kalganova T, Nwokoro E et al. (2024) Approaches to Improving Medication Adherence Prediction in Chronic Disease Patient. Int J Adv Life Sci, 16(1&2):33–43.
Nab L et al. (2024) OpenSAFELY: A platform for analysing electronic health records designed for reproducible research. Pharmacoepidemiol Drug Saf, 33(6).
NCHA (2024) Best Kept Secret: The Value of Clinical Homecare to the NHS, Patients and Society. National Clinical Homecare Association Report.
NCHA (2025) Overview of Clinical Homecare Services. National Clinical Homecare Association.
NHSBSA (2022) Prescribing Costs in Hospitals and the Community – England 2021/22. NHSBSA Statistics and Data Science Report.
NHSBSA (2023) Prescription Cost Analysis – England – 2022-23. NHSBSA Statistics and Data Science Report.
ONS (2022) UK health indicators: 2019 to 2020: Estimates to understand the UK population’s health status by sex. Based on the European Health Interview Survey (EHIS) for 2019 to 2020. Uses age-standardised rates. ONS Statistical Bulletin.
Patel T (2022) Medication nonadherence: Time for a proactive approach by pharmacists; Can Pharm J (Ott), 154(5):292–296.
Regal Chambers Surgery (2024) 28 Day Prescribing Policy, Company Website Report.
Sayed A, Himeur Y & Bensaali F (2023) From timeseries to 2D images for building occupancy prediction using deep transfer learning. Eng Appl Artif Intell, 119: 105786.
Stuurman-Bieze AG, Hiddink EG, van Boven JF et al. (2014) Proactive pharmaceutical care interventions decrease patients' nonadherence to osteoporosis medication. Osteoporos Int, 25(6):1807-12.
Webb R (2014) Improving medicines adherence and reducing waste. Eastern Academic Health Science Network.
Zanni D & Nwokoro E (2024) Enhancing healthcare outcomes and cost efficiency through patient support programs: a comprehensive analysis. International Journal of Pharmacy Practice, 32(2):12–13.
Zheng Y et al. (2014) Unobtrusive Sensing and Wearable Devices for Health Informatics. IEEE Trans. Biomedical Engineering, 61:1538–1554.