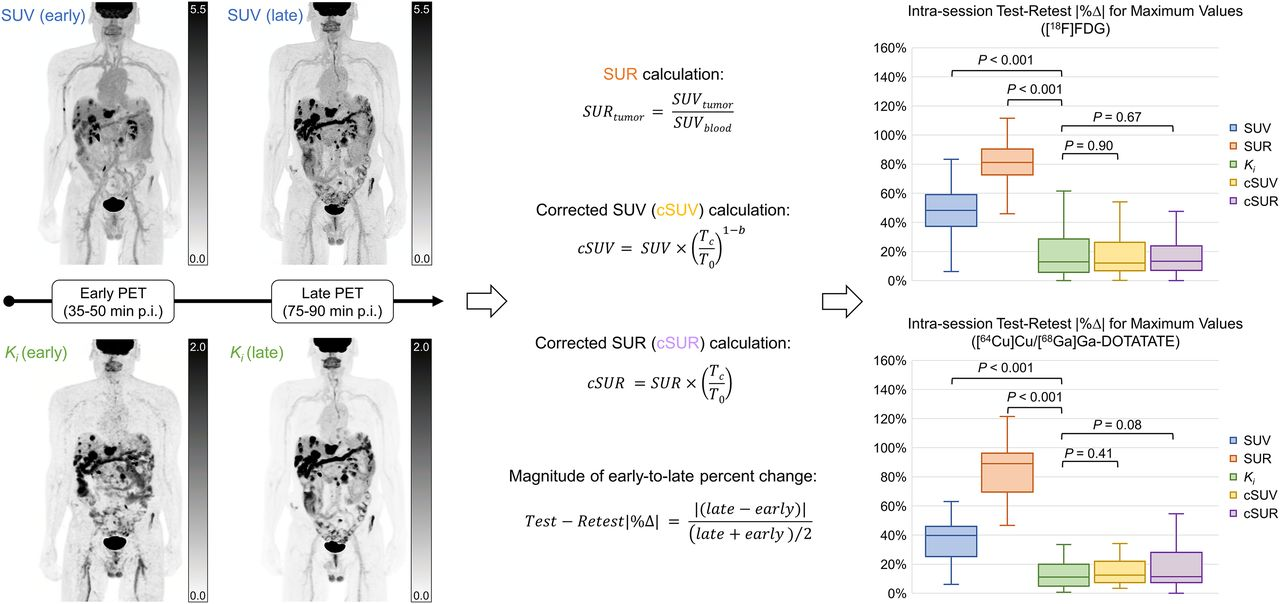
Oncologic PET/CT imaging plays a critical role in the diagnosis, treatment planning, and monitoring of cancer patients. However, one of the significant challenges in PET/CT is the time dependence of traditional metrics like Standardised Uptake Value (SUV). This time dependence can introduce variability in tracer uptake measurements, affecting the reliability of the data. To address these challenges, researchers have proposed various alternative metrics that minimise time dependence, such as the net influx rate (Ki), corrected SUV (cSUV), and corrected Standardised Uptake Ratio (cSUR). This article explores these metrics and their potential to provide more consistent and reliable oncologic PET/CT imaging data.
The Limitations of SUV in Oncologic PET/CT Imaging
The Standardised Uptake Value (SUV) is a widely used PET/CT imaging metric for quantifying tumour tracer uptake. However, SUV is sensitive to several factors, including patient weight, glucose levels, and, most importantly, the time elapsed between tracer injection and image acquisition. As tumours accumulate tracers continuously, variations in the uptake time can lead to significant differences in SUV measurements between scans. This time dependence limits SUV's effectiveness as a reliable biomarker for treatment response, particularly in busy clinical settings where exact scan timing is difficult to maintain.
The time dependence of SUV creates challenges in comparing sequential scans for monitoring treatment efficacy. Even minor variations in uptake time can lead to discrepancies in SUV measurements, potentially leading to incorrect interpretations of tumour response. This variability highlights the need for more stable metrics that can provide consistent data regardless of the timing of the scan.
Exploring Ki and Its Role in PET/CT Imaging
The net influx rate (Ki) is derived from dynamic PET/CT imaging and represents the rate at which the tumour tissue takes up the tracer over time. Unlike SUV, which is prone to increase with time, Ki is expected to remain relatively constant once steady-state conditions are achieved between the blood and tissue compartments. This makes Ki a promising candidate for reducing PET/CT imaging time dependence.
Ki has shown potential as a prognostic biomarker in various cancer types, sometimes outperforming SUV-based metrics. However, calculating Ki requires dynamic imaging and estimating arterial input functions (AIFs), which can be time-consuming and technically challenging. Additionally, motion-related errors during dynamic imaging can introduce further variability in Ki measurements. Despite these challenges, Ki remains a valuable tool for providing more stable and reliable oncologic PET/CT imaging data.
The Potential of Corrected SUV and SUR
Corrected SUV (cSUV) and corrected Standardised Uptake Ratio (cSUR) have been proposed as alternatives to traditional SUV and SUR metrics. These corrected metrics adjust for differences in uptake time, aiming to provide more consistent measurements across scans. cSUV is calculated by retrospectively modifying the observed SUV based on the actual versus targeted uptake times. Similarly, cSUR adjusts the tumour-to-blood ratio for uptake time, potentially allowing it to estimate Ki without needing dynamic imaging.
Studies have shown that cSUV and cSUR exhibit lower time dependence than their uncorrected counterparts. In particular, cSUR has demonstrated a strong correlation with Ki, making it a promising surrogate marker for dynamic imaging-derived metrics. This is particularly advantageous in clinical settings where dynamic imaging may not be feasible or practical. By minimising time dependence, cSUV and cSUR can improve the accuracy and reliability of PET/CT imaging in assessing tumour activity and treatment response.
Conclusion
The quest for time-independent metrics in oncologic PET/CT imaging is essential for improving the reliability and consistency of data used in cancer diagnosis and treatment monitoring. While traditional metrics like SUV are widely used, their time dependence can introduce variability and affect the accuracy of treatment assessments. Ki, derived from dynamic imaging, offers a more stable alternative but comes with its own set of challenges. Corrected metrics like cSUV and cSUR provide a practical compromise, reducing time dependence without the need for dynamic imaging.
As PET/CT technology continues to evolve, adopting these corrected metrics could lead to more accurate and reliable assessments of tumour activity, ultimately improving patient outcomes. Further research and validation of these metrics in diverse patient populations will be crucial in determining their effectiveness in routine clinical practice.
Source Credit: Journal of Nuclear Medicine
Image Credit: iStock