High-grade gliomas (HGGs) are aggressive brain tumours with a grim prognosis, even with advancements in cancer treatment. Monitoring the progression of these tumours is crucial for effective patient management, but conventional MRI techniques often struggle to distinguish between tumour progression and treatment effects. Advanced MRI-based neuroimaging, including perfusion imaging and spectroscopy, has emerged as a promising tool to bridge this gap. However, its influence on clinical decision-making has not been extensively studied. This article explores the role of advanced neuroimaging in managing HGGs and its impact on neuro-oncologists clinical decisions.
Advanced Neuroimaging Techniques: Enhancing Tumour Assessment
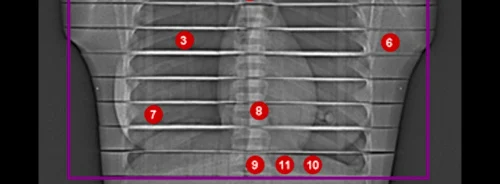
Advanced neuroimaging techniques, such as MR perfusion imaging and MR spectroscopy, have been developed to provide a more detailed assessment of brain tumours post-treatment. MR perfusion imaging measures blood flow within the tumour, identifying areas with abnormal blood vessel growth, which is indicative of tumour progression. MR spectroscopy, on the other hand, analyses the chemical composition of brain tissue, helping to differentiate between tumour recurrence and treatment-induced changes. These techniques significantly improve over conventional MRI, which often cannot accurately distinguish between tumour growth and the effects of treatments like radiation.
The diagnostic accuracy of these advanced imaging techniques has been well established, with studies showing their effectiveness in identifying tumour progression in patients with high-grade gliomas. However, their true value lies in translating these imaging findings into clinical decision-making. Neuro-oncologists rely on these advanced techniques to guide treatment decisions, such as whether to continue current therapies, change chemotherapy agents, or consider surgical intervention.
The Clinical Impact of Advanced Neuroimaging on Decision-Making
A prospective study conducted at a comprehensive cancer centre examined the impact of advanced neuroimaging on the clinical decisions made by neuro-oncologists treating patients with HGGs. The study included 63 patients who underwent 70 advanced neuroimaging sessions. The results revealed that advanced neuroimaging significantly influenced clinical decision-making in 44% of the episodes of care, where the neuro-oncologists intended management plans changed after receiving the neuroimaging results.
The changes in management decisions were particularly notable in cases where the advanced imaging showed either unexpected tumour progression or treatment effects that were not apparent on conventional MRI. For example, in cases where the initial plan was to enrol the patient in a clinical trial or change chemotherapy agents, advanced neuroimaging findings prompted alternative treatment strategies. This highlights the importance of incorporating advanced neuroimaging into routine follow-up protocols for patients with HGGs.
Challenges and Considerations in Implementing Advanced Neuroimaging
While the benefits of advanced neuroimaging in clinical decision-making are clear, challenges are associated with its widespread adoption. One of the primary concerns is the cost and resource utilisation involved in performing these advanced imaging techniques. Unlike conventional MRI, advanced neuroimaging requires specialised equipment, longer scan times, and expertise in image interpretation. Moreover, the additional sequences involved in advanced neuroimaging, such as perfusion and spectroscopy, increase the complexity of the imaging process.
Another challenge is the variability in interpreting advanced neuroimaging results. While the study showed that neuro-oncologists found advanced neuroimaging helpful in 93% of episodes, there were instances where the imaging results did not align with clinical expectations, leading to uncertainty in decision-making. This variability underscores the need for standardised protocols and training to ensure consistent interpretation of advanced neuroimaging across different clinical settings.
Conclusion
Integrating advanced MRI-based neuroimaging into the clinical management of high-grade gliomas represents a significant advancement in neuro-oncology. The ability of these techniques to differentiate between tumour progression and treatment effects provides neuro-oncologists with valuable information that directly impacts patient care. However, the challenges of cost, resource utilisation, and variability in interpretation must be addressed to fully realise the potential of advanced neuroimaging in routine clinical practice. As the field continues to evolve, further research is needed to refine the indications for advanced neuroimaging and to assess its long-term impact on patient outcomes. Ultimately, the goal is to ensure these advanced techniques are used effectively to improve patients' lives with high-grade gliomas.
Source: American Journal of Roentgenology
Image Credit: iStock