A radiation exposure extraction engine that detects anomalous radiation events has been developed.
Ronald Summers, MD, PhD, of iCAD, presented results from a study of the software at the 2014 Radiological Society of North American (RSNA) annual meeting.
The study aimed to detect anomalous radiation events by taking into account patient and exam-specific clinical characteristics, as current practice is based on a general threshold for all patient sizes and exams. The researchers implemented a statistical method for context-dependent CT radiation sentinel event detection directly from the DICOM header. They developed a patient- and scan-specific radiation exposure outlier detector low-cost fully automated system that is seamlessly integrated with the Picture Archiving and Communication System (PACS).
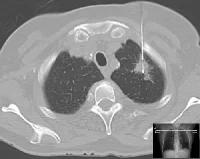
The radiation exposure extraction engine (RE3), built using open source software, continually queries the PACS, extracts the information to a standalone workstation, analyses the image for scan parameters, extracts it as a text file and outputs as business intelligence.
The researchers used a multivariable regression model that used scanned body volume and water equivalent diameter instead of body mass index (BMI). Patient and scanner parameters (study description, scan length, dose length product (DLP), patient age, scanner model) were obtained for computed tomography (CT) chest, abdomen and pelvis data from a 2 month period (n=892). The software was trained to be nonsensitive to outliers. BMI data was acquired from RIS. A multivariable regression was applied with scanner model, age, BMI, BMI*scan length, height and weight as predictors for DLP. Using leave-one-out cross validation, we predict a DLP for each exam. All exams with observed DLPs greater than two standard deviations (95th percentile) from the mean residual were flagged. All studies were also analysed with a simple thresholding model to identify exams with DLPs over two standard deviations above the mean of all exams. Exams flagged by the context-dependent and independent methods were checked for factors in patient weight and multi-phase exams.
18 anomalous exams were detected, with a mean DLP of 2678 mGy*cm (1350 to 4101). The context-independent thresholding detected 43 with a mean DLP of 2765 mGy*cm (2206 to 4101). 11 exams were detected by both methods. The average BMI for exams detected by the context-dependent model (n=7) was 25.6 ±6.5 kg/m2, and that of those only by the thresholding model (n=32) was 36.9±5.2 kg/m2 (mostly obese patients). The average number of acquisitions for exams detected only by the context-dependent model was 1.6 ± 0.8 passes and that of the thresholding model was 2.7±0.58 passes (mostly multi-phase exams).
Summers explained that their model takes into account clinical context and therefore detects patient-specific outliers missed by simple thresholding, but does not falsely flag exams that would be detected by simple thresholding due to high exposure from patient weight and multiple phases.
When asked what they do with data outliers, Summers explained that they hold weekly quality assurance meetings. These do not occur commonly, but when they do, they act on them as quickly as possible, and inform both the patient and the referring physician.
Claire Pillar
Managing Editor, HealthManagement
Ronald Summers, MD, PhD, of iCAD, presented results from a study of the software at the 2014 Radiological Society of North American (RSNA) annual meeting.
The study aimed to detect anomalous radiation events by taking into account patient and exam-specific clinical characteristics, as current practice is based on a general threshold for all patient sizes and exams. The researchers implemented a statistical method for context-dependent CT radiation sentinel event detection directly from the DICOM header. They developed a patient- and scan-specific radiation exposure outlier detector low-cost fully automated system that is seamlessly integrated with the Picture Archiving and Communication System (PACS).
The radiation exposure extraction engine (RE3), built using open source software, continually queries the PACS, extracts the information to a standalone workstation, analyses the image for scan parameters, extracts it as a text file and outputs as business intelligence.
The researchers used a multivariable regression model that used scanned body volume and water equivalent diameter instead of body mass index (BMI). Patient and scanner parameters (study description, scan length, dose length product (DLP), patient age, scanner model) were obtained for computed tomography (CT) chest, abdomen and pelvis data from a 2 month period (n=892). The software was trained to be nonsensitive to outliers. BMI data was acquired from RIS. A multivariable regression was applied with scanner model, age, BMI, BMI*scan length, height and weight as predictors for DLP. Using leave-one-out cross validation, we predict a DLP for each exam. All exams with observed DLPs greater than two standard deviations (95th percentile) from the mean residual were flagged. All studies were also analysed with a simple thresholding model to identify exams with DLPs over two standard deviations above the mean of all exams. Exams flagged by the context-dependent and independent methods were checked for factors in patient weight and multi-phase exams.
18 anomalous exams were detected, with a mean DLP of 2678 mGy*cm (1350 to 4101). The context-independent thresholding detected 43 with a mean DLP of 2765 mGy*cm (2206 to 4101). 11 exams were detected by both methods. The average BMI for exams detected by the context-dependent model (n=7) was 25.6 ±6.5 kg/m2, and that of those only by the thresholding model (n=32) was 36.9±5.2 kg/m2 (mostly obese patients). The average number of acquisitions for exams detected only by the context-dependent model was 1.6 ± 0.8 passes and that of the thresholding model was 2.7±0.58 passes (mostly multi-phase exams).
Summers explained that their model takes into account clinical context and therefore detects patient-specific outliers missed by simple thresholding, but does not falsely flag exams that would be detected by simple thresholding due to high exposure from patient weight and multiple phases.
When asked what they do with data outliers, Summers explained that they hold weekly quality assurance meetings. These do not occur commonly, but when they do, they act on them as quickly as possible, and inform both the patient and the referring physician.
Claire Pillar
Managing Editor, HealthManagement
Latest Articles
CT, radiation dose, RSNA 2014, #RSNA14
A radiation exposure extraction engine that detects anomalous radiation events has been developed. Ronald Summers, MD, PhD, of iCAD, presented results fro...