Stroke remains a leading global health concern, ranking as the second most common cause of death worldwide. Among the various types of strokes, acute anterior-circulation large vessel occlusion (LVO) strokes are particularly challenging, often leading to severe disability or death. The advent of endovascular thrombectomy (EVT) has revolutionised the treatment of these strokes, offering significant improvements in patient outcomes. However, a critical complication of EVT is intracranial haemorrhage (ICH), which can severely compromise recovery and increase mortality. While combining EVT with intravenous alteplase has been shown to enhance functional outcomes, it also raises the risk of ICH. Thus, accurately predicting ICH risk post-EVT is vital for developing personalised treatment strategies that minimise complications and improve patient safety.
The Critical Need for Predicting Intracranial Haemorrhage in EVT
Intracranial haemorrhage is a major concern in the management of stroke patients undergoing EVT. The occurrence of ICH not only diminishes the beneficial effects of EVT but also poses a significant threat to patient survival and quality of life. Identifying patients who are at increased risk for ICH allows clinicians to implement preventive measures, such as adjusting the use of anticoagulants or selecting alternative therapeutic strategies. The risk factors for ICH include the thrombus's size and composition, the patient's baseline health condition, and the extent of blood-brain barrier (BBB) disruption during the procedure. By understanding and predicting these factors, medical professionals can better navigate the delicate balance between effective clot removal and minimising hemorrhagic risks.
Thrombus Composition and Blood-Brain Barrier Disruption: Key Factors in ICH Risk
The composition of a thrombus, including its density and structure, significantly influences the success of EVT and the likelihood of complications such as ICH. During EVT, the mechanical removal of the clot can inadvertently damage the arterial wall, leading to BBB disruption. This disruption facilitates the leakage of blood components into the brain parenchyma, causing inflammation, oedema, and potentially exacerbating the risk of ICH. The perithrombus region, the area immediately surrounding the thrombus, is particularly susceptible to these adverse effects. The initial assessment of patients using non-contrast CT (NCCT) and CT angiography (CTA) scans provides critical insights into these regions, but traditional evaluation methods are often subjective and limited. This underscores the need for more objective, data-driven approaches to accurately assess and predict ICH risk.
Radiomics: A Cutting-Edge Approach to Predicting ICH Post-EVT
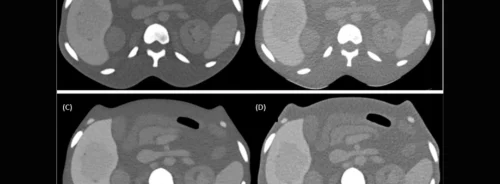
Radiomics is an innovative field that involves extracting a large number of quantitative features from medical images, which can reveal patterns and characteristics not visible to the naked eye. This approach has shown great promise in oncology and is now being applied to stroke imaging. Analysing the radiomic features from intrathrombus and perithrombus regions makes it possible to identify subtle changes in tissue characteristics that correlate with an increased risk of ICH. This study extracted CT-based radiomics features from patients undergoing EVT, focusing on the thrombus and its surrounding tissue. The goal was to develop a predictive model that could accurately identify patients at higher risk for ICH, thereby guiding clinicians in tailoring their interventions more effectively.
The process involved delineating regions of interest (ROIs) on CT images, extracting radiomic features, and constructing predictive models using advanced statistical methods. The study found that radiomic features from the perithrombus region, in particular, were strongly associated with ICH risk, highlighting the critical role of BBB integrity in post-EVT outcomes. The predictive model could provide a comprehensive assessment of ICH risk by integrating these radiomics data with clinical information, such as patient demographics and comorbidities.
The application of radiomics in predicting intracranial haemorrhage after EVT represents a significant advancement in stroke care. This study demonstrates that radiomics can provide valuable insights into the characteristics of thrombus and surrounding tissues, offering a more nuanced understanding of the factors contributing to ICH. Developing predictive models incorporating intrathrombus and perithrombus radiomic features can significantly enhance the precision of ICH risk assessment, leading to more personalised and safer treatment strategies. However, the study also highlights the need for further research, particularly in validating these models across diverse populations and clinical settings. Future work should focus on integrating radiomics with other emerging technologies, such as deep learning, to refine and expand predictive capabilities. By leveraging these advancements, healthcare providers can improve the outcomes of stroke patients undergoing EVT, ultimately reducing the incidence and impact of ICH.
Source Credit: European Journal of Radiology
Image Credit: iStock