Tracheostomies are among the most common procedures performed in critically ill patients, and intensive care nurses can take an active role in helping restore speech to patients with tracheostomies, according to a report published in the journal Critical Care Nurse. Nursing assessments and interventions to help patients regain the ability to speak after a tracheostomy are described in the report.
“Losing the ability to speak after a tracheostomy adds to the stress, fear and frustration of being critically ill,” says lead author Linda L. Morris, PhD, APN, CCNS, FCCM, who is a tracheostomy specialist/consultant. "Restoring speech to a patient after a tracheostomy allows them to more fully and effectively express their needs and wishes, participate in their plan of care and converse with their loved ones and caregivers.”
Speaking after a tracheostomy depends on having an adequate supply of air reach the vocal cords with a minimum of resistance, and the tracheostomy tube itself is an important factor related to phonation, or the ability to make sound with one’s vocal cords. In addition, changing the type of tube and its diameter or length can help avoid complications and lead to greater success in phonation.
The report summarises different approaches to restore phonation in patients with a tracheostomy, including special considerations related to nursing interventions. The methods vary, depending on whether the patient is spontaneously breathing, being treated with intermittent mechanical ventilation or is fully ventilator dependent.
Critical care nurses work as part of an interdisciplinary team that includes respiratory therapists, speech pathologists, advanced practice nurses and physicians to coordinate care and develop a patient-specific communication plan, which is essential to the goal of voice restoration. Early involvement of this team, the report notes, can improve clinical outcomes and patient satisfaction by reducing the time needed for phonation.
“An essential component of successfully helping a patient regain the ability to speak is to determine which option or options are most appropriate, and nurses need to be aware of all the options available,” explains Dr. Morris, also an associate professor of clinical anaesthesiology, Feinberg School of Medicine, Northwestern University, Chicago. The co-editor/author of the 2010 edition of “Tracheostomies: The Complete Guide,” she also serves on the board of directors for the Global Tracheostomy Collaborative.
Source: American Association of Critical-Care Nurses
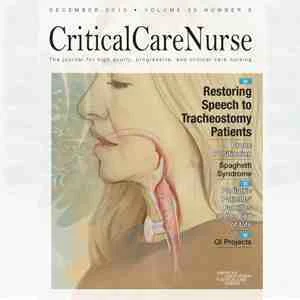
Image credit: Pat Thomas Medical Illustration
“Losing the ability to speak after a tracheostomy adds to the stress, fear and frustration of being critically ill,” says lead author Linda L. Morris, PhD, APN, CCNS, FCCM, who is a tracheostomy specialist/consultant. "Restoring speech to a patient after a tracheostomy allows them to more fully and effectively express their needs and wishes, participate in their plan of care and converse with their loved ones and caregivers.”
Speaking after a tracheostomy depends on having an adequate supply of air reach the vocal cords with a minimum of resistance, and the tracheostomy tube itself is an important factor related to phonation, or the ability to make sound with one’s vocal cords. In addition, changing the type of tube and its diameter or length can help avoid complications and lead to greater success in phonation.
The report summarises different approaches to restore phonation in patients with a tracheostomy, including special considerations related to nursing interventions. The methods vary, depending on whether the patient is spontaneously breathing, being treated with intermittent mechanical ventilation or is fully ventilator dependent.
Critical care nurses work as part of an interdisciplinary team that includes respiratory therapists, speech pathologists, advanced practice nurses and physicians to coordinate care and develop a patient-specific communication plan, which is essential to the goal of voice restoration. Early involvement of this team, the report notes, can improve clinical outcomes and patient satisfaction by reducing the time needed for phonation.
“An essential component of successfully helping a patient regain the ability to speak is to determine which option or options are most appropriate, and nurses need to be aware of all the options available,” explains Dr. Morris, also an associate professor of clinical anaesthesiology, Feinberg School of Medicine, Northwestern University, Chicago. The co-editor/author of the 2010 edition of “Tracheostomies: The Complete Guide,” she also serves on the board of directors for the Global Tracheostomy Collaborative.
Source: American Association of Critical-Care Nurses
Image credit: Pat Thomas Medical Illustration
References:
Morris LL et al. (2015) Restoring Speech to Tracheostomy Patients. Crit
Care Nurse, 35(6): 13-28. doi: 10.4037/ccn2015401
Latest Articles
healthmanagement, critically ill, intensive care, nurses, tracheostomy, speech, mechanical ventilation
Tracheostomies are among the most common procedures performed in critically ill patients, and intensive care nurses can take an active role in helping restore speech to patients with tracheostomies, according to a report published in the journal Critical